Symptoms: prolonged elevated temperature, temperature 37, progressive increase in body temperature, rapid heartbeat, clouding, loss of consciousness, nausea, weakness, convulsions, heaviness in the head, headache, feeling of heat, feeling of cold, chills, excruciating thirst, increased nervous excitability, irritability, neurosis, hallucinations, pale skin, redness of the skin, insomnia, shortness of breath, excessive sweating, chest pain, abdominal pain.
Low-grade fever is an elevated body temperature that lasts for a long period of time. In diseases of the autonomic nervous system, this temperature can last for months and years, and the amplitude of its fluctuations usually does not exceed 37 - 37.8 degrees.
As a rule, elevated body temperature reflects some kind of inflammatory process inside the body, caused by infections, parasites, allergens, or even oncology. The cause of low-grade fever in adults is often sought in diseases of the thyroid gland (hyperthyroidism), and in children - in inflammation of the tonsils. However, it also happens that numerous clinical studies do not reveal any pathologies, and the removal of tonsils does not lead to normalization of body temperature. Then it makes sense to talk about problems in the functioning of the autonomic nervous system.
In our practice, this symptom occurs very often. It is associated with dysfunction of thermoregulation, one of the main functions of the autonomic nervous system. Actually, it is precisely thanks to this function of this part of the nervous system that we are able to observe on a thermogram (thermal imaging study) disturbances in one or another vegetative node.
Low-grade fever may be accompanied by general malaise, wave-like manifestations of increased sweating, feelings of heat or cold, chills and other symptoms that usually accompany elevated body temperature or a general disorder of the autonomic nervous system (headache, rapid heartbeat, etc.).
Cases from practice
Woman, 21 years old, student.
In December 2013, a young girl came to the clinic. For the last few months, my body temperature has constantly remained at 37.2-37.5. The physique is asthenic, the skin is pale, with excessive sweating, from time to time I felt hot. At times, the symptoms were accompanied by increased irritability and anxiety. I experienced headaches several times a week. I often experienced general weakness, melancholy, and dizziness.
First, the patient turned to a therapist, who prescribed her a series of examinations: general and biochemical analysis of urine and blood, X-ray of the lungs, ultrasound of internal organs, etc. The causes of the elevated temperature could not be identified. The doctor said that this was primary hyperthermia against the background of vegetative dystonia, that this was normal and would go away with age. You need to gain a little weight, walk more in the fresh air, rest, do physical exercise, you can take vitamins.
In this state, studying and working became more and more problematic: it was “difficult to understand,” I was constantly thirsty and, as a result, had to go to the toilet, and often needed to leave the room and go out into the fresh air. The girl’s parents were looking for options to alleviate this diagnosis and came to our clinic.
The autonomic disorder arose due to a stressful lifestyle and mild traumatic brain injury at the age of 14 years.
After two courses of treatment, the girl completely recovered.
Woman, 25 years old.
A young girl contacted us in 2015. Since February 2014, she began to experience panic attacks (vegetative crises).
About a year before the first attack of inexplicable fear, the girl underwent surgery under general anesthesia. Immediately after this, symptoms such as sleep disturbance and increased anxiety began to appear. In addition, with a strong psycho-emotional stress (“overworried”), the girl’s temperature rose to 37.5 degrees and could last for several hours.
The patient's general condition was characterized by constant anxiety and chills. The extremities were usually cold. I was worried about the heaviness in the neck area.
She underwent one course of treatment at the Clinical Center for Autonomic Neurology. Already during treatment, panic attacks stopped bothering me. Soon the patient noted a steady improvement in her condition. A month after the course, I felt completely healthy.
Features of the course of influenza in certain categories of neurological patients
Summary. The article discusses issues related to the peculiarities of the course of influenza against the background of neurological diseases: influenza in epilepsy and other conditions characterized by increased convulsive readiness, influenza in certain pathologies of the peripheral nervous system, influenza in neuromuscular diseases and multiple sclerosis, influenza and cerebral vascular pathology . In a number of patients with diseases of the nervous system, infection with the influenza virus and the development of the infectious process are accompanied by an increased risk of worsening the course of the disease, worsening the prognosis, the need for hospitalization, and an unfavorable outcome of the infection. The feasibility and priority of influenza vaccine prevention in individuals with specific nosologies that fall within the competence of a neurologist are discussed. Vaccine prevention in many cases is recognized as an effective measure to prevent severe influenza in neurological patients and the development of complications. The clinician needs in-depth knowledge of the indications and limitations of influenza vaccine prophylaxis in patients with pathology of the nervous system.
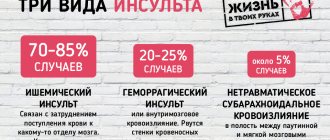
The neurotropic properties of some viruses and, as a consequence, their tendency to damage the central and peripheral nervous system (NS) are well known and described in the literature. In addition to viruses that have a targeted damaging effect almost exclusively on neurons (an example would be the tick-borne encephalitis virus), NS pathologies can be caused by known viruses, for which neurotropism is a rather atypical property. Here it is appropriate to mention the viruses of measles, herpes simplex, human immunodeficiency, etc. In addition, it is now known that respiratory viruses can also cause NS pathology. Thus, the neurological complications of influenza have been described in sufficient detail, including dementia, epileptiform seizures, cerebrovascular diseases, febrile seizures, toxic encephalopathy, encephalitis, meningitis, transverse myelitis, subarachnoid hemorrhages [1, 2]. It so happened that an increase in cases of the development of symptoms characteristic of Parkinson’s disease and “lethargic encephalitis” was registered precisely after the “Spanish” influenza pandemic of 1918 [3]. Influenza virus RNA and pathogen antigens are found in brain cells, as well as in the ganglia of the vagus and trigeminal nerves at the earliest stages of infection [4]. The possibility of spread of the influenza virus by retrograde axonal transport, its ability to overcome the blood-brain barrier, induce the production of cytokines, as well as macrophage and lymphocytic infiltration of nervous tissue have been shown [5]. Thus, in addition to the direct damaging effect on neurons, the influenza virus can cause pathological chemokine-induced reactions - for example, H3N2 is not able to replicate in the central nervous system (CNS), but it can increase the level of TNF-α in the hippocampus, as well as potentiate the proliferation of microglia [6]. However, most authors recognize that even today the exact mechanism of the damaging effect of the influenza virus on the elements of the central and peripheral nervous system remains unclear.
It is logical to assume that the adverse effects of the interaction of NS with the influenza virus are reciprocal in nature. The course of seasonal and pandemic influenza in patients with existing neurological diseases may have its own significant characteristics. In real clinical practice, the presence of chronic pathology of the central or peripheral NS can be of great importance for patient management tactics and prognosis. However, the literature contains very scanty descriptions of the characteristics of the course of influenza against the background of neurological diseases. Also, the feasibility and priority of influenza vaccine prevention in individuals with specific nosologies that fall within the competence of a neurologist remain the subject of many years of discussion.
Influenza in epilepsy and other conditions characterized by increased convulsive readiness
Of all the neurological symptoms of influenza, febrile seizures are most often described [7]. Norwegian researchers have found that having a previous diagnosis of epilepsy significantly increases the risk of hospitalization if infected with seasonal influenza. Epilepsy was registered in 5.3% (2017-2018 epidemic season) and 4.4% (2018-2019 epidemic season) of children hospitalized with influenza [8]. Considering the data that in Norway, Great Britain, and Finland epilepsy is diagnosed in 0.5% of children in the general population, the difference seems quite significant. Thus, among patients with epilepsy, the risk of hospitalization for influenza is increased. In the United States, epilepsy is recognized as a significant risk factor for severe influenza and an increased risk of fatal outcomes of influenza in children due to a greater likelihood of developing respiratory failure [9].
A study in Bavaria found that chronic neurological disorders occurred in 8.2% of children hospitalized for influenza. Along with other concomitant pathologies (bronchial asthma, obesity), patients with NS diseases more often required respiratory support in the form of oxygen supply and artificial ventilation [10]. Australian authors point to an increased risk of developing uncontrolled seizures during respiratory infections in children with cerebral palsy (CP), which in turn may increase salivation. Hypersalivation is especially characteristic of generalized tonic-clonic seizures. Increased salivation and decreased level of consciousness increase the risk of aspiration. Taking antiepileptic drugs, mainly due to their side effects of sedation, also increases the risk of aspiration. In addition, benzodiazepines, especially clonazepam, themselves increase salivation. Therefore, when managing patients with epilepsy and severe influenza, attention should be paid to optimizing antiepileptic therapy, which can reduce the risks of respiratory disease by reducing the likelihood of aspiration [11].
According to a study conducted in Taiwan, in adults, epilepsy was classified as a condition that significantly increases the risk of death from seasonal influenza in all age groups (including adults and older patients), especially during epidemic periods [12]. .
Influenza in some pathologies of the peripheral nervous system
Diseases of peripheral nervous system are usually mentioned together with influenza in the context of complications of influenza infection [13]. Cases of Guillain–Barré syndrome (GBS) associated with influenza are especially often described in the literature [14]. There is no doubt about the key role of the influenza virus in inducing the synthesis of autoantibodies aimed at peripheral NS antigens. In particular, this is evidenced by the detection in the blood of patients during the acute stage of development of the syndrome of antibodies to peripheral myelin, capable of fixing complement [15]. It is assumed that cell membrane conjugates, such as gangliosides, are also targets of the autoimmune process. A previous influenza infection serves as a provoking factor that triggers an autoimmune reaction. In addition, several studies have shown that influenza or influenza-like illness can also cause the development of Miller-Fisher syndrome, which is characterized by pathogenetic mechanisms similar to those of GBS [16].
The literature describes a case of clinical deterioration during influenza infection in a patient suffering from Lewis–Sumner syndrome (LSS) [17]. LSS is considered an asymmetric sensorimotor variant of chronic inflammatory demyelinating polyneuropathy (CIDP) with predominantly distal involvement of the extremities and electrophysiological signs of multifocal motor conduction blocks. Involvement of cranial nerves is rarely reported. A 57-year-old patient suffered from KCC for a long time (14 years), the clinical course was described as stable, clinical manifestations of iRODS score 45/48 (mild). Against the background of pneumonia caused by the influenza A virus (H1N1), which lasted for 4 days, the patient developed left-sided peripheral paresis of the facial muscles with a pronounced predominance in the lower half, dysphagia, dysphonia, paresis of the neck muscles, sensorimotor dysfunction of the left hand and a sharply worsened motor deficit in the right lower limb (to the symptom of “drop foot” was added a violation of plantar flexion and extension in the knee joint). The condition turned out to be so severe and deteriorated so rapidly that a cerebrovascular accident was suspected, which was not confirmed by dynamic neuroimaging. Electrophysiological examination confirmed an exacerbation of CIDP with the appearance of increased latency of the facial nerve, more so on the left. The exacerbation began to stop on the 2nd day from the beginning, and on the 6th day of antiviral therapy, the condition improved almost to its previous status, even without the use of immunomodulators and corticosteroids. However, relief could not be called complete, and after 3 months the iRODS score was 42/48. The authors suggest that there was a viral neuritis, which may develop due to the ability of the influenza virus to block the functioning of sodium channels.
Diabetic polyneuropathy in influenza is discussed mainly in light of the fact that patients with diabetes mellitus (DM) have an increased risk of hospitalization and severe infection compared with individuals without DM [18]. Diabetes is recognized as one of the most common underlying conditions and a risk factor for complications of H1N1 influenza [19].
Influenza in neuromuscular diseases
Myalgia is one of the most common extrapulmonary manifestations of influenza [20]. The influenza virus has a tropism for muscle cells, especially immature ones, so influenza-associated myositis is not uncommon in pediatric practice, but lesions of motor units also occur in adults. Influenza B is characterized by a greater tendency to damage muscles [21]. In an experiment, during influenza infection, the expression of genes involved in inflammation increased in the skeletal muscle tissue, and this process was characterized by the most pronounced and prolonged peak activity in older individuals [22]. In humans, elevated blood levels of creatine phosphokinase correlated with worse influenza outcomes (length of stay in the intensive care unit, increased incidence of pulmonary and extrapulmonary complications) [23]. This gives serious grounds to assume a more severe course of influenza in patients with neuromuscular diseases.
Indeed, the literature describes a clinical case of influenza infection in a 5-year-old patient with spinal muscular atrophy. The disease was characterized by a fulminant onset, an extremely severe course, early development of signs of impaired vital functions (heart rate - 200 beats per minute or more, respiratory rate - 64 per minute, blood oxygen saturation - 66%), and, despite timely hospitalization and active treatment in the intensive care unit, a fatal outcome was observed. The authors note that this patient was not vaccinated against influenza [24].
It is known that upper respiratory tract infections can aggravate symptoms and in some cases provoke the development of myasthenic crisis [25]. However, myasthenia gravis is a type of immunopathological condition with neurological manifestations where influenza vaccination should be carried out with great caution. Experts from the British Association of Neurologists believe that in patients with myasthenia gravis, any vaccination should be considered only for health reasons. It should also be taken into account that when carrying out immunosuppressive therapy, the effectiveness of vaccination may be reduced. Live vaccines are absolutely contraindicated in the presence of myasthenia gravis; the administration of attenuated vaccine preparations is associated with an increased risk of exacerbation of the disease. But patients requiring immunosuppressive therapy can still receive the necessary vaccine prophylaxis if necessary. Vaccination against influenza, as well as pneumococcus, Haemophilus influenzae and Varicella zoster, may be considered, according to the regional vaccination schedule. If possible, in myasthenia gravis, vaccination (with blood tests to assess immune response) should be planned before starting immunosuppressive therapy [26].
Flu and multiple sclerosis
Patients with multiple sclerosis (MS), due to physical limitations and receipt of immunomodulatory therapy, are at increased risk of infectious diseases and associated decline in neurological function. Indeed, after influenza, an increase in the frequency of exacerbations in MS patients is recorded, which is associated with the effect of inflammatory mediators and activation of the demyelinating process [27]. Both short-term deterioration in function and permanent consequences are possible - the latter are likely the result of irreversible demyelination. Viral infections have been shown to be associated with the clinical activity of MS; therefore, infectious diseases such as influenza can cause relapses and acute deterioration of neurological functions [28]. MS patients with influenza require hospitalization more often than people in the general population [29]. Meanwhile, influenza vaccination can prevent this unfavorable scenario [30]. Therefore, in some countries, the proportion of people with MS who get vaccinated against influenza is higher than among the general population. This allows us to reduce the frequency of exacerbations of MS and hospitalizations associated with influenza, which was confirmed by data from a retrospective study from 2008-2014. including 6755 patients with MS [31].
In addition to true exacerbations that influenza can stimulate, Uchtoff's symptom is known - a transient short-term deterioration of neurological functions in patients with MS in response to an increase in body temperature. The exact mechanism of this phenomenon remains unclear. It is likely due to a combination of structural and physiological changes in CNS axons during demyelination. The condition is benign; it is distinguished from a true exacerbation of MS by the absence of negative dynamics on MRI of the brain, the positive effect of hypothermia, and the duration of no more than 24 hours [32].
Influenza and cerebral vascular pathology
There are no indications in the literature to assess the risk of developing recurrent cerebrovascular accidents during influenza, although these data are of great interest in practical terms. Since meningoencephalitis is not a common and typical extrapulmonary manifestation of influenza, it is likely that the risk of worsening cerebral vascular disease is expected to be lower than with herpes infection. In addition, unlike herpes group viruses, vaccine prophylaxis is available for influenza, which, according to some data, reduces the risk of recurrent stroke. Thus, when admitted to hospital for stroke or transient ischemic attack, only 6% of patients regularly vaccinated against influenza indicate the presence of previous cerebral vascular events, while among a population comparable in age and place of residence this figure was about 19% [ 33]. A case-control study conducted in Germany showed that patients admitted to hospital for ischemic or hemorrhagic stroke or transient ischemic attack were significantly less likely to indicate a history of influenza vaccination both during the last vaccination campaign and in previous seasons. compared with healthy volunteers of the same sex and age and living in the same area [33].
Discussion: focus on vaccinations
The US Centers for Disease Control and Prevention (CDC) recommends regular influenza vaccination as the first and most important step in preventing this infection and the possible severe complications it can cause in patients with chronic neurological disorders [ 34]. The United States Advisory Committee on Immunization Practices (ACIP) officially recognizes NS as a risk factor for severe influenza and recommends vaccination [35]. In general, in clinical practice this recommendation can be followed, but with some reservations.
The material presented above gives an idea that in some categories of neurologist’s patients, the recommendation of influenza vaccination can be considered unconditional. These are, for example, patients with vascular pathology of the brain. In a randomized controlled trial of 439 patients, the composite cardiovascular outcome measure MACE (death or hospitalization for acute coronary syndrome, heart failure, or stroke) was significantly lower in participants who received influenza vaccination [36]. An unambiguous recommendation to undergo vaccination also applies to patients with NS disorders developing as a result of diabetes. The American Diabetes Association (ADA), CDC, and ACIP recommend that people with diabetes receive seasonal influenza vaccination, and the World Health Organization (WHO) recommends that people with diabetes receive additional immunization against H1N1 influenza vaccine with a single dose to minimize morbidity and mortality associated with this pathogen in this category of patients [37, 38].
Influenza vaccination is also recommended for children with epilepsy due to a significantly increased risk of increased seizure activity due to viral infections that provoke an increase in body temperature [39]. Research shows that this recommendation is not followed. For example, in Australia, approximately 20% of children with cerebral palsy do not comply with the routine vaccination schedule, which is more than 2 times higher than the percentage of “violations” in the general population (about 8%). The most frequently neglected vaccinations are against measles, mumps and rubella, followed by polio and DTP (diphtheria, tetanus and whooping cough) [40]. On average, only every second child with chronic NS pathology is vaccinated against influenza [41].
One of the actively discussed issues is the advisability of influenza vaccine prophylaxis in patients with MS due to fears of developing an exacerbation of MS [42]. The risk of relapse following influenza vaccination (seasonal and pandemic) has been examined in several studies, which have found no association between influenza vaccination and an increased risk of developing MS in adults [43, 44]. Administration of live attenuated vaccine is not recommended for patients with MS [45]. Glucocorticoids, teriflunomide, interferon beta, rituximab and natalizumab do not impair the immune response after influenza vaccination [46–49]. But for safety reasons, after pulse therapy it is recommended to delay vaccination for at least 2 weeks. The use of mitoxantrone, fingolimod, and azathioprine may impair the immunogenicity and effectiveness of the influenza vaccine [50-52]. Patients receiving mitoxantrone/cyclophosphamide should be vaccinated between courses of the drug. For immunosuppressive therapy, it is recommended to determine the antibody titer 4 weeks after vaccination. If the antibody titer does not increase, it is recommended to consider repeated administration of the vaccine product [45].
In myopathies, the position regarding influenza vaccination depends on the specific nosology. Thus, for Salih myopathy, annual influenza vaccination and other immunizations associated with respiratory infections are recommended [53]. In case of myasthenia gravis, the administration of any vaccine preparations is carried out with great caution; live vaccines are contraindicated, as discussed in detail above.
Conclusion
Thus, knowledge of current recommendations and the position of leading professional societies on the issue of vaccination of neurological patients against influenza is a real necessity for a clinician working with this group of patients. But according to an online survey conducted by the World Federation of Neurology, the level of training in this area leaves much to be desired. The majority (82.7%) of the 184 neurologists surveyed said they recommend influenza vaccination for patients with myasthenia gravis, but less than half of respondents (42.7%) recommend it for GBS [54]. This is a paradoxical example when world practice contradicts the recommendations directly set out by the CDC. This indicates a lack of awareness among neurologists regarding influenza vaccine prevention and determines the need to include this section in medical education programs.
CONFLICT OF INTEREST. The authors of the article have confirmed that there is no conflict of interest to disclose.
CONFLICT OF INTERESTS. Not declared.
Literature/References
- Radzišauskiene D., Vitkauskaite M., Zvinyte K., Mameniškiene R. Neurological complications of pandemic A(H1N1)2009pdm, postpandemic A(H1N1)v, and seasonal influenza A // Brain Behav. 2021; 11(1):e01916. DOI: 10.1002/brb3.1916.
- Vlajinac H., Dzoljic E., Maksimovic J., Marinkovic J., Sipetic S., Kostic V. Infections as a risk factor for Parkinson's disease: A case?control study // International Journal of Neuroscience, 2013; 123: 329-332. 10.3109/00207454.2012.760560.
- Taubenberger JK The origin and virulence of the 1918 “Spanish” influenza virus // Proc Am Philos Soc. 2006; 150: 86-112.
- Park CH, Ishinaka M, Takada A, Kida H, Kimura T, Ochiai K, et al. The invasion routes of neurovirulent A Hong Kong 483/97 (H5N1) influenza virus into the central nervous system after respiratory infection in mice // Arch. Virol. 2002; 147: 1425-1436. 10.1007/s00705-001-0750-x.
- Bohmwald K., Gálvez NMS, Ríos M., Kalergis AM Neurologic Alterations Due to Respiratory Virus Infections // Front Cell Neurosci. 2018; 12: 386. Published 2021 Oct 26. DOI: 10.3389/fncel.2018.00386.
- Hosseini S., Wilk E., Michaelsen-Preusse K., Gerhauser I., Baumgärtner W., Geffers R., et al. Long-term neuroinflammation induced by influenza A virus infection and the impact on hippocampal neuron morphology and function // J. Neurosci. 2018; 38: 3060-3080. 10.1523/JNEUROSCI.1740-17.2018.
- Toovey S. Influenza-associated central nervous system dysfunction: A literature review // Travel Med Infect Dis. 2008; 6: 114-124.
- Hauge SH, Bakken IJ, de Blasio BF, Håberg SE Risk conditions in children hospitalized with influenza in Norway, 2017-2019 // BMC Infect Dis. 2020; 20 (1): 769. Published 2021 Oct 19. DOI: 10.1186/s12879-020-05486-6.
- Keren R., Zaoutis TE, Bridges CB, Herrera G., Watson BM, Wheeler AB, et al. Neurological and neuromuscular disease as a risk factor for respiratory failure in children hospitalized with influenza infection // Jama. 2005; 294(17):2188-2194. DOI: 10.1001/jama.294.17.2188.
- Wieching A., Benser J., Kohlhauser-Vollmuth C., Weissbrich B., Streng A., Liese JG Clinical characteristics of pediatric hospitalizations associated with the 2009 pandemic influenza A (H1N1) in Northern Bavaria, Germany // BMC Res Notes. 2012; 5: 304. Published 2012 Jun 18. DOI: 10.1186/1756-0500-5-304.
- Marpole R., Blackmore AM, Gibson N., Cooper MS, Langdon K., Wilson AC. Evaluation and Management of Respiratory Illness in Children With Cerebral Palsy // Front Pediatr. 2020; 8: 333. Published 2021 Jun 24. DOI: 10.3389/fped.2020.00333.
- Weng TC, Chiu HR, Chen SY, Shih FY, King CC, Fang CC National retrospective cohort study to identify age-specific fatality risks of comorbidities among hospitalized patients with influenza-like illness in Taiwan // BMJ Open. 2019; 9(6):e025276. Published 2021 Jun 24. DOI: 10.1136/bmjopen-2018-025276.
- Hayase Y., Tobita K. Influenza virus and neurological diseases // Psychiatry Clin Neurosci. 1997; 51 (4): 181-184. DOI: 10.1111/j.1440-1819.1997.tb02580.x. PMID: 9316161.
- Yamana M., Kuwahara M., Fukumoto Y., Yoshikawa K., Takada K., Kusunoki S. Guillain-Barré syndrome and related diseases after influenza virus infection // Neurol Neuroimmunol Neuroinflamm. 2019; 21:e575.
- Hughes RA, Hadden RD, Gregson NA, Smith KJ Pathogenesis of Guillain-Barré syndrome // J Neuroimmunol. 1999; 100: 74-97.
- Hara M., Morita A., Ichihara K., et al. Miller Fisher syndrome associated with influenza A infection // Intern Med. 2012; 51: 2621-2623.
- Peleg AY, Weerarathna T., McCarthy JS, Davis TM Common infections in diabetes: Pathogenesis, management and relationship to glycemic control // Diabetes Metab Res Rev. 2007; 23:3-13.
- Miller AC, Subranian RA, Safi F., Sinert R., Zehtabchi S., Elamin EM Influenza A 2009 (H1N1) virus in admitted and critically ill patients // J Intensive Care Med. 2011; 27: 25-31.
- Luís Ribeiro, Ana Monteiro, João Martins. Hyperacute relapse of Lewis-Sumner syndrome during influenza A (H1N1) virus infection // BMC Neurol. 2020; 20: 427. Published online 2021 Nov 24. DOI: 10.1186/s12883-020-02008-4.
- Gibson SB, Majersik JJ, Smith AG, Bromberg MB Three cases of acute myositis in adults following influenza-like illness during the H1N1 pandemic // Journal of neurosciences in rural practice. 2013; 4: 51-54.
- Servidei S., Miranda AF, Gamboa ET Infectivity of influenza B virus in cultured human muscle // Acta Neuropathol. 1987; 73: 67-76.
- Bartley JM, Pan SJ, Keilich SR, et al. Aging augments the impact of influenza respiratory tract infection on mobility impairments, muscle-localized inflammation, and muscle atrophy // Aging (Albany NY). 2016; 8 (4): 620-635. DOI: 10.18632/aging.100882.
- Borgatta B., Perez M., Rello J., Vidaur L., Lorente L., Socias L., Pozo JC, Pozo J., Garnacho-Montero J., Rello J. Elevation of creatine kinase is associated with worse outcomes in 2009 pH1N1 influenza A infection // Intensive Care Med. 2012; 38: 1152-1161.
- Li T., Qi N., Gao X., Yu H. Rescue of four pediatric patients with severe influenza A (H3N2) in Weifang, China // J Int Med Res. 2018; 46 (11): 4800-4805. DOI: 10.1177/0300060518792795.
- Kalita J., Kohat AK, Misra UK Predictors of outcome of myasthenic crisis // Neurol Sci. 2014; 35: 1109-1114.
- Sussman J., Farrugia M.E., Maddison P., et al. Myasthenia gravis: Association of British Neurologists' management guidelines // Practical Neurology. 2015; 15: 199-206.
- Buljevac D., Flach HZ, Hop WC, et al. Prospective study on the relationship between infections and multiple sclerosis exacerbations // Brain. 2002; 125 (Pt 5): 952-960. DOI: 10.1093/brain/awf098.
- Williamson EM, Berger JR Infection risk in patients on multiple sclerosis therapeutics // CNS Drugs. 2015; 29 (3): 229-244. DOI: 10.1007/s40263-015-0226-2.
- Marrie RA, Elliott L, Marriott J, et al. Dramatically changing rates and reasons for hospitalization in multiple sclerosis // Neurology. 2014; 83 (10): 929-937. DOI: 10.1212/WNL.0000000000000753.
- Mailand MT, Frederiksen JL Vaccines and multiple sclerosis: a systematic review // J Neurol. 2021. DOI: 10.1007/s00415-016-8263-4.
- Ghaderi S., Berg-Hansen P., Bakken IJ, Magnus P., Trogstad L., Håberg SE Hospitalization following influenza infection and pandemic vaccination in multiple sclerosis patients: a population-based registry study from Norway // Eur J Epidemiol. 2020; 35 (4): 355-362. DOI: 10.1007/s10654-019-00595-2.
- Panginikkod S., Rayi A., Rocha Cabrero F., Rukmangadachar LA. Uhthoff Phenomenon. 2021 Oct 23. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. PMID: 29261916.
- Grau AJ, Fischer B., Barth C., Ling P., Lichy C., Buggle F. Influenza vaccination is associated with a reduced risk of stroke // Stroke. 2005; 36 (7): 1501-1506.
- Grohskopf LA, Sokolow LZ, Broder KR, Olsen SJ, Karron RA, Jernigan DB, et al. Prevention and control of seasonal influenza with vaccines // MMWR Recomm Rep. 2016; 65:1-54.
- Centers for Disease Control and Prevention. Prevention and control of seasonal influenza with vaccines. Recommendations of the Advisory Committee on Immunization Practices-United States, 2013-2014 // MMWR Recomm Rep. 2013; 62: 1-43.
- Phrommintikul A., Kuanprasert S., Wongcharoen W., Kanjanavanit R., Chaiwarith R., Sukonthasarn A. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome // Eur Heart J. 2011; 32 (14): 1730-1735.
- American Diabetes Association (ADA) Standards of medical care in diabetes-2011 // Diabetes Care. 2011; 33:S11-61.
- Centers for Disease Control and Prevention (CDC) The Pink Book: Chapters Epidemiology and Prevention of Vaccine Preventable Diseases. 12th Edition. 2011.
- Chiu SS, Tse CY, Lau YL, Peiris M. Influenza a infection is an important cause of febrile seizures // Pediatrics. 2001; 108(4):E63. DOI: 10.1542/peds.108.4.e63.
- Greenwood VJ, Crawford NW, Walstab JE, Reddihough DS Immunization coverage in children with cerebral palsy compared with the general population // J Paediatr Child Health. 2013; 49: 137-41. 10.1111/jpc.12097.
- Smith M., Peacock G., Uyeki TM, Moore C. Influenza vaccination in children with neurological or neurodevelopmental disorders // Vaccine. 2015; 33 (20): 2322-2327. DOI: 10.1016/j.vaccine.2015.03.050.
- McNicholas N., Chataway J. Relapse risk in patients with multiple sclerosis after H1N1 vaccination, with or without seasonal influenza vaccination // J Neurol. 2011; 258(8):1545-1547.
- Auriel E., Gadoth A., Regev K., Karni A. Seasonal and H1N1v influenza vaccines in MS: safety and compliance // J Neurol Sci. 2012; 314 (1-2): 102-103.
- Mailand MT, Frederiksen JL Vaccines and multiple sclerosis: a systematic review // J Neurol. 2021. DOI: 10.1007/s00415-016-8263-4.
- Baghbanian SM Influenza vaccination in patients with multiple sclerosis is possible with some considerations // Iran J Neurol. 2016; 15 (2): 109-110.
- Schwid SR, Decker MD, Lopez-Bresnahan M. Immune response to influenza vaccine is maintained in patients with multiple sclerosis receiving interferon beta-1a // Neurology. 2005; 65 (12): 1964-1966.
- Vagberg M., Kumlin U., Svenningsson A. Humoral immune response to influenza vaccine in natalizumab-treated MS patients // Neurol Res. 2012; 34 (7): 730-733.
- Bar-Or A., Freedman MS, Kremenchutzky M., Menguy-Vacheron F., Bauer D., Jodl S., et al. Teriflunomide effect on immune response to influenza vaccine in patients with multiple sclerosis // Neurology. 2013; 81 (6): 552-558.
- Van Assen S, Holvast A, Benne CA, Posthumus MD, van Leeuwen MA, Voskuyl AE, et al. Humoral responses after influenza vaccination are severely reduced in patients with rheumatoid arthritis treated with rituximab // Arthritis Rheum. 2010; 62 (1): 75-81.
- Olberg HK, Cox RJ, Nostbakken JK, Aarseth JH, Vedeler CA, Myhr KM Immunotherapies influence the influenza vaccination response in multiple sclerosis patients: an explorative study // Mult Scler. 2014; 20 (8): 1074-1080.
- Kappos L., Mehling M., Arroyo R., Izquierdo G., Selmaj K., Curovic-Perisic V., et al. Randomized trial of vaccination in fingolimod-treated patients with multiple sclerosis // Neurology. 2015; 84 (9): 872-879.
- Abu-Shakra M., Press J., Varsano N., Levy V., Mendelson E., Sukenik S., et al. Specific antibody response after influenza immunization in systemic lupus erythematosus // J Rheumatol. 2002; 29 (12): 2555-2557.
- Hackman P., Savarese M., Carmignac V., et al. Salih Myopathy. 2012 Jan 12 . In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2021.
- Electronic resource https://wfneurology.org/2019-08-18-aan-neurology-today Date of access 02/08/2021 https://wfneurology.org/2019-08-18-aan-neurology-today Data obrashcheniya 08.02 .2021.]
E. G. Demyanovskaya*, **,1, Candidate of Medical Sciences A. S. Vasilyev**, Candidate of Medical Sciences
* GBUZ IKB No. 1 DZM, Moscow, Russia ** FGBU DPO TSMA UDP RF, Moscow, Russia
1Contact information
Features of the course of influenza in some categories of neurological patients / E. G. Demyanovskaya, A. S. Vasiliev For citation: Demyanovskaya E. G., Vasiliev A. S. Features of the course of influenza in some categories of neurological patients // Attending Physician. 2021; 3 (24): 56-60. DOI: 10.51793/OS.2021.24.3.011 Tags: neurological diseases, seizure readiness, flu vaccine prevention
VSD in faces
This page contains excerpts from patient histories, covering the main complaints with which people turn to us for help. This is done with the goal of showing how different and “complex” the symptoms of vegetative-vascular dystonia can be. And how closely it is sometimes “fused” with disturbances in the functioning of organs and systems. How it “disguises” itself as “heart”, “pulmonary”, “stomach”, “gynecological” and even “psychiatric” problems that people have to live with for years...
To learn more
1.General information
A persistent increase in body temperature above the standard established by nature of 36.6 ° C (in the armpit) should not be ignored. Any prolonged or chronic change in homeostasis (constancy of the internal conditions of the body) is an emergency for which compelling reasons must be found. Even if the temperature rises slightly, within one degree (up to the so-called subfebrile values), and remains at this level for a long time, this is already a symptom, that is, by definition, a sign of pathology, and it is important to establish in a timely manner, - which one.
Sometimes this can be very difficult.
It should be noted that the historically familiar method of measuring body temperature in the armpit is not a standard and is due only to the convenience of using a mercury thermometer, including for diagnosing the condition of children. The temperature of different parts of the human body is not the same: for example, in the mouth, ear, anus it is several tenths of a degree higher, i.e. low-grade fever for these zones is the norm, and the norm is even more stable than the temperature range of 36.5 - 36.7 in the armpits - therefore, in many cases it is advisable to measure the temperature rectally.
It is also known that the norm is not absolute, universal for all people: depending on the individual characteristics of metabolism, it can vary slightly. However, the general principle remains unchanged: an abnormally high body temperature for a given organism means acceleration of all biochemical reactions, increased heat transfer, and exceeding the limit of energy consumption and oxygen consumption. Biological “machines” are designed very economically, operate with high efficiency and do not have the ability to waste resources. Consequently, by increasing temperature the body is forced to react to something.
A must read! Help with treatment and hospitalization!
2. Reasons
There are a great many reasons for an increase in temperature, many of which are purely situational, but in this case, low-grade fever is always transient in nature and passes more or less quickly. These are, for example, temperature fluctuations during the day (slightly higher in the evening), in response to intense physical activity, overheating, a stressful situation, or (in women) the ovulation phase of the cycle.
An increase in temperature is one of the most common, almost always occurring reactions to an infection, no matter what pathogen it is caused by; Accordingly, persistent low-grade fever often turns out to be a symptom of a chronic infectious-inflammatory process, with which the immune system has entered into a kind of “clinch” without a clear “winner.”
The causes can also be HIV/AIDS, oncological processes, endocrine disorders (usually thyroid pathology), autoimmune diseases, asthenic conditions after an illness, anemia, viral hepatitis, chronic inflammation of the structures of the nasopharynx, kidneys, reproductive system, etc.; eroding and ulcerating diseases of the gastrointestinal tract, parasitosis, cardiovascular pathology, taking certain medications.
Visit our Therapy page