28.06.2019
Stroke is an acute disorder of cerebral circulation due to blockage of blood vessels or their rupture. After a vascular accident, neurological symptoms develop within a few minutes or hours, which progress, sometimes leading to death. Recently, cases of stroke have become more frequent at young ages, up to 30 years.
Types of disease
Stroke is a pathology accompanied by impaired blood circulation in certain areas of the brain. The condition is accompanied by oxygen starvation and a severe deficiency of nutrients, which ultimately leads to the death of brain cells. As a result, there is a complete or partial loss of functions for which the affected area was responsible.
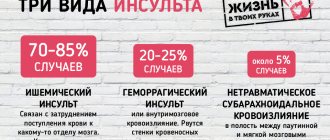
Depending on the underlying cause, there are two types of stroke:
- Ischemic (most common). It is a consequence of blockage of the lumens of cerebral vessels. The disease progresses slowly and is not accompanied by hemorrhage, but is accompanied by the death of brain cells.
- Hemorrhagic. Caused by hemorrhage in the brain tissue as a result of rupture of a local vessel. Due to the accumulation of blood and pressure exerted on a certain area of the brain, its functions are impaired.
Important! The cause of a stroke may be cerebrovascular disease.
Symptoms, signs and first aid
Anyone can have a stroke, which is why it is so important to know the primary symptoms of the condition. It is indicated by:
- weakness in the limbs;
- fainting conditions;
- numbness of half the face, distortion of features;
- Strong headache;
- speech impairment, misunderstanding;
- various visual impairments;
- complete or partial paresis;
- impaired coordination of movements up to its complete loss;
- impaired skin sensitivity;
- instability and tension of the pulse.
If we talk about what pressure is possible during a stroke, then its indicators can be both low and high. To make sure that the patient has had a stroke, he must be asked to perform several familiar actions. For example, smile broadly or say a few words. He will not succeed: the affected part of the face will remain motionless, and speech will be unclear, as if the person’s mouth is filled with porridge and he is trying to speak through it.
What to do if this happens? First of all, immediately call an ambulance. Lay the patient down so that the head is elevated in relation to the legs, unbutton the collar, and remove the woman’s bra. A person must breathe deeply. Trying to lower blood pressure on your own is strictly prohibited.
When to reduce
It is impossible to lower blood pressure after a stroke artificially, with the help of medications. Since this significantly reduces the body’s protective and regenerative abilities. Because of this, blood flow through the vessels to the affected cells is reduced, and this directly affects the recovery of the brain after a stroke. If you are at risk of having a stroke, you should definitely call a doctor and follow the doctor’s further instructions. Self-medication is strictly prohibited!
What blood pressure can trigger the development of a stroke?
At what blood pressure level can a stroke occur and can the condition develop at normal blood pressure? It is worth noting that most often a stroke occurs in hypertensive patients. The reasons are:
- Stably high blood pressure, which does not decrease even while taking medications;
- sharp jumps in indicators caused by a stressful situation or significant physical activity;
- refusal of treatment for hypertension and heart disease.
Doctors call the physiological level of blood pressure, at which all body systems operate in a natural mode, a level of 120/80 mm. rt. Art. When it increases to 180/120, we can talk about the development of a hypertensive crisis, which can quite easily turn into an apoplexy (stroke).
The danger in terms of the development of pathology is represented by too small a difference between the upper and lower blood pressure readings. If it is less than 40 units, then the likelihood of blockage of the vascular lumen increases significantly. Therefore, a blood pressure of 130/110 is more likely to trigger the development of a stroke than a blood pressure of 160/90.
Keeping Blood Pressure at a Healthy Level
To reduce the risk of stroke with hypertension, you need to give up medications that increase blood pressure (if you can refuse, be sure to consult your doctor first), also give up alcohol, smoking, and normalize your daily routine. And if you still manage to minimize the level of stress, then you are unlikely to face an increase in blood pressure. In general, the main thing is to maintain a healthy lifestyle, and then the risk of stroke drops sharply. The same applies to other people, not just hypertensive people.
Acceptable indicators and pressure deviations after impact
What blood pressure should a patient have after a stroke? Everything will depend on the type of pathology.
Ischemic form
During the first few hours after the formation of the condition, almost all patients experience high blood pressure. This is a protective reaction of the brain aimed at stabilizing the work of the myocardium. That is why a specialist should select antihypertensive drugs, taking into account the current condition of the patient.
Incorrectly selected medications can reduce blood pressure too much. The worst outcome in this case may be the death of a person. In addition, recovery after a stroke will be longer and more difficult.
Indications for emergency reduction of blood pressure are:
- increase to 180/220–100/120 mm. rt. st;
- the need to administer an antithrombotic agent;
- development of systemic circulatory failure;
- diagnosing aneurysm/arteriovenous malformation of cerebral vessels;
- disorders of the kidneys.
During the first 48–72 hours after an ischemic stroke has occurred, blood pressure can be reduced by no more than 15% relative to the existing one. At this time, increased blood pressure is normal.
Important! In patients who do not have a history of hypertensive pathology, blood pressure should not fall below 165/95 mm. rt. Art. In the presence of the disease, the minimum level is determined by 185/105 mm. rt. Art.
It is very important to protect the patient from factors that can provoke a sharp increase in blood pressure. These include nervous tension, severe pain, and fluid retention.
Hemorrhagic form
This type of stroke occurs against the background of a significant increase in blood pressure, so antihypertensive therapy should be started as early as possible. Taking medications helps:
- reducing the volume of the hematoma, stopping its spread;
- decrease in intracranial pressure;
- blocking the development of swelling of brain tissue.
The critical level of blood pressure, upon reaching and overcoming which it is necessary to take measures to reduce, is considered to be 140/90 mm. rt. Art. But the decline should be gradual. During the day, it can be lowered only by 20% relative to the current one.
Heart attack and stroke: signs, emergency care, prevention
Myocardial infarction is a disease in which, due to blockage of the coronary artery, the full blood supply to an area of the heart muscle (myocardium) suddenly and abruptly stops, which leads to a severe lack of oxygen (ischemia), nutrients and death of myocardial cells. This area can no longer take part in heart contractions, so the heart cannot provide blood flow to the body. All organs and tissues begin to experience oxygen starvation, which leads to disruption of their function. The main cause of heart attack is elevated levels of cholesterol and certain lipids in the blood.
Typical manifestations of myocardial infarction are a feeling of severe pressure or pain behind the sternum, or slightly to the left or right of it. The pain is most often squeezing, pressing, tearing (feeling of a stake in the chest), sometimes burning. Irradiation of pain to the left shoulder girdle, shoulder, arm, less often to the neck and lower jaw, sometimes to the right half of the shoulder girdle is typical. Occasionally, the pain is localized in the epigastric region. Unlike angina, pain during myocardial infarction lasts more than half an hour, usually several hours. Nitroglycerin taken brings only minor and short-term relief. Severe weakness and cold sweat are often noted. Often in the acute stage of myocardial infarction, patients experience nausea, vomiting, hiccups, and bloating, which are of a reflex nature. In some cases, myocardial infarction is practically asymptomatic.
During the period of pain, the patient's face has a suffering appearance, the skin is usually pale, sometimes with a cyanotic tint. Breathing is rapid. Blood pressure may rise when pain occurs, but soon drops to an unusually low level for the patient. The pulse is frequent, heart sounds are weakened. In most patients, various cardiac arrhythmias can be detected.
If you or someone else suddenly has the above characteristic signs of a heart attack, even with weak or moderate intensity, which last more than 5 minutes, do not hesitate, immediately call an ambulance team. Do not wait more than 10 minutes - in such a situation it is life-threatening.
The recovery period after a myocardial infarction lasts 4-6 weeks. It occurs differently in different patients. Most often, during this period, patients remain able to work, but they sometimes experience angina attacks. In rare cases, the course of the post-infarction period is interrupted by the onset of a second infarction.
The results of large-scale international studies, in particular the INTERHEART study, showed that the following factors have a decisive influence on the risk of developing myocardial infarction: dyslipidemia, smoking, hypertension, abdominal obesity, psychosocial factors (stress, social isolation, depression), diabetes mellitus, reduce the risk : eating enough vegetables and fruits, regular physical activity.
Emergency self-help and mutual assistance measures in case of a heart attack (myocardial infarction).
In our country, up to 80% of deaths occur outside of medical organizations - at home, at work, in the country, in public and other places. Most of them occur suddenly or by the mechanism of sudden death. However, with knowledge of simple first aid techniques on the part of people surrounding a person who finds himself in such a critical condition, as well as everyone’s knowledge of first self-help measures, can in most cases save the patient’s life.
Characteristic signs (symptoms) of a heart attack (myocardial infarction)
• sudden (paroxysmal) pressing, squeezing, burning, aching pain in the chest (behind the sternum) lasting more than 5 minutes;
• similar pains are often observed in the left shoulder (forearm), left shoulder blade, left half of the neck and lower jaw, both shoulders, both arms, the lower part of the sternum along with the upper abdomen;
• lack of air, shortness of breath, severe weakness, cold sweat, nausea often occur together and sometimes follow or precede discomfort/pain in the chest
• often these manifestations of the disease develop against the background of physical or psycho-emotional stress, but more often with some interval after them.
Algorithm of urgent actions:
• Call an emergency medical team.
• Sit (preferably in a chair with armrests) or lie in bed with the head of the bed raised, take 0.25 g of acetylsalicylic acid (aspirin) (chew the tablet, swallow) and 0.5 mg of nitroglycerin (put the tablet/capsule under the tongue, first bite the capsule , do not swallow); free your neck and provide fresh air (open the vents or windows).
• If after 5-7 min. After taking acetylsalicylic acid (aspirin) and nitroglycerin, pain persists, you need to take nitroglycerin a second time.
• If pain persists 10 minutes after taking the second dose of nitroglycerin, it is necessary to take nitroglycerin a third time.
• If after the first or subsequent doses of nitroglycerin there is severe weakness, sweating, shortness of breath, you need to lie down, raise your legs (on a bolster, etc.), drink 1 glass of water and then, as with a severe headache, do not take nitroglycerin.
• If the patient has previously taken cholesterol-lowering medications, give the patient his usual daily dose and take the drug with you to the hospital.
Attention! A patient with a heart attack is strictly forbidden to get up, walk, smoke or eat until the doctor’s special permission;
You should not take aspirin (acetylsalicylic acid) if you are intolerant to it (allergic reactions), as well as with obvious or worsening peptic ulcers of the stomach and duodenum;
Nitroglycerin should not be taken if there is severe weakness, sweating, or if there is severe headache, dizziness, or acute impairment of vision, speech, or coordination of movements.
Prevention of myocardial infarction.
As for the prevention of atherosclerosis, everyone who has become familiar with the factors contributing to its occurrence knows what to do. The one who sharply reduces the consumption of animal fats and develops a rational attitude to nutrition will do the right thing. You should eat low-fat cottage cheese and low-fat kefir. More fiber-rich vegetables should be included in the menu - raw and sauerkraut, beets, carrots (at least 500 g per day). Fiber helps remove excess cholesterol from the body. When the first cases of increased pressure are detected, for which you need to regularly, at least once every one to two months, measure blood pressure and, by contacting a doctor, take the necessary measures, it is quite possible to stop the development of hypertension (blood pressure should not be higher than 140/90 mm Hg. Art.). If elevated cholesterol levels are determined, then by resorting to dietary and drug treatment, the progression of atherosclerosis can be delayed (the maximum permissible level of cholesterol in the blood is 5 mmol/l). The most important preventive measure is to stop smoking. Harmful substances in cigarette smoke contribute to the development and progression of atherosclerosis, cause fluctuations in blood pressure, thicken the blood and provoke thrombosis. The danger is posed by so-called passive smoking, so it is important not only to quit smoking, but also not to be in areas where smoking is allowed and in the company of smokers. Smoking significantly reduces the effect of physical training, so the desire to achieve the maximum effect from exercise and lead an active lifestyle is another reason to stop smoking.
In order to timely identify initial disturbances in the activity of the cardiovascular system and, if necessary, prescribe optimal drug treatment that can prevent the development of myocardial infarction, experts strongly advise regular medical examinations or preventive medical examinations at the clinic at the place of residence.
Finally, it is important to remember that only a doctor prescribes treatment for a heart attack, and the patient and his relatives strictly follow the instructions. Self-medication of a heart attack, no matter how easy it may be, is unacceptable!
Stroke: causes, symptoms, prevention.
In the modern world, people suffer from such a disease as “stroke” more often than from “myocardial infarction”. Residents of large cities are most susceptible to this disease, where life is full of stress and anxiety, and there is also an unfavorable environmental situation. Stroke accounts for approximately 6 million deaths per year worldwide and is second only to coronary heart disease as a cause of death.
A stroke is a terrible blow, which often divides not only the life of the patient, but also the life of his family into two parts: “Before” and “After”. Everything can change overnight: an active, active person can become a helpless disabled person in need of constant outside help, caring for which places a heavy burden on his loved ones, creating considerable socio-economic difficulties for society. What kind of life are people forced to lead after suffering a severe stroke? This is a real genuine tragedy and tears invisible to the world, since for many of them even leaving the apartment is an insoluble problem, and it is not so rare that the disease is bedridden, making the patient completely dependent on others.
A stroke is an acute disorder of cerebral circulation, leading to damage to the brain substance and disruption of its functions. There are two types of this disease: ischemic stroke and hemorrhagic stroke. Ischemic stroke occurs when the lumen of a vessel is blocked by a thrombus or embolus. The cause of a hemorrhagic stroke is a rupture of the vessel wall and blood entering the brain.
Many risk factors for stroke are common to other cardiovascular diseases. They are divided into two large groups: internal - high blood pressure, age, family history (stroke, myocardial infarction, hypertension in close relatives), high blood cholesterol, obesity; external – emotional stress, sedentary lifestyle, bad habits, environmental features. In addition, stroke has risk factors unique to it: initial manifestations of insufficient blood supply to the brain, dyscirculatory encephalopathy, transient cerebrovascular accidents, and previous strokes.
The onset of a stroke can vary. Hemorrhagic stroke occurs suddenly. Subsequently, patients can even indicate at what hour and even minute they began to experience symptoms of the disease: severe headache, vomiting, dizziness, weakness, malaise. There may be a deterioration in a person’s orientation in the surrounding space, difficulty speaking, loss of consciousness, and the development of paralysis. With ischemic stroke, the onset may be slow. Often patients note increasing sensations of weakness in one half of the body, a gradual deterioration in speech, swallowing, facial distortion, and unsteady gait.
When the first such signs appear, the most correct thing is to immediately call an ambulance and hospitalize the patient in the neurological department. If a person’s stroke has developed acutely, with loss of consciousness and signs of paralysis, before the ambulance arrives, the patient must be turned on his side and a pillow placed under his head (if this happened at home); rolled up clothes or a bag (if this happened outside the home). To make breathing easier, unfasten your collar and, holding your head with your hands, constantly wipe away the foam with a handkerchief so that it does not get into your respiratory tract. To prevent the patient from biting his tongue, a comb or stick wrapped in a scarf can be inserted between the teeth. You cannot hold your arms and legs with force, trying to unclench your cramped fingers, much less lean on the patient with your whole body. This may make the seizure worse. The patient's arms and legs should only be held lightly so that he does not injure himself and others. And no ammonia! It may cause respiratory arrest. You cannot move a patient during an attack. If the patient’s pulse cannot be felt, the heart has stopped, and breathing has stopped, an indirect cardiac massage and mouth-to-mouth artificial respiration must be performed. Everything else is the task of the ambulance team.
Stroke prevention is based on the basic principles of a healthy lifestyle.
· Know and control your blood pressure - it should not be more than 140/90 mmHg.
· Do not start smoking or stop smoking as soon as possible.
· Add as little salt as possible to your food and avoid canned and processed foods that contain it in excess.
· Control your blood cholesterol levels – the maximum allowable level is 5 mmol/l.
· Follow the basic principles of a healthy diet - eat more vegetables and fruits (at least 500 g per day), avoid added sugar and saturated animal fat.
· Don't drink alcohol. The risk of stroke is highest in the first hours after drinking alcohol.
· Exercise regularly. Even moderate physical activity (walking outdoors for 30 minutes a day) reduces the risk of developing cardiovascular diseases, including stroke.
Preventative medical examinations and consultations that you can undergo:
— in a clinic at your place of residence, where you can undergo medical examination or in-depth preventive examination;
— at the Health Center (in Krasnodar at Tramvaynaya str., 5), where your blood pressure will be measured, your blood glucose and cholesterol levels will be determined, and your body mass index will be calculated. Knowing your risk for developing heart disease can help you develop a specific action plan to improve your heart health.
Low and high blood pressure
During the first 24 hours after the impact, maintaining high blood pressure is an acceptable norm. The danger is high blood pressure that persists for a week after a stroke. The symptom indicates incorrect treatment. In this case, the patient becomes incapacitated and develops neurological disorders.
Such negative consequences for the patient’s health are due to the continuing increase in cerebral edema, which results in wedging of the brain stem into the occipital part. It is possible that breathing processes may be disrupted until a critical condition develops, as well as heart failure and cardiac arrest.
Complications of hypertensive crisis
If the pressure, despite the therapy, still jumps, then the consequences may be as follows:
- re-strike;
- expansion of the ischemic focus;
- development of encephalopathy;
- hemorrhage in the skull.
Why does a patient have low blood pressure after a stroke and why is this condition considered negative by doctors? A rapid decrease in blood pressure occurs against the background of the following pathological conditions:
- development of a major stroke;
- brain stem damage;
- the formation of cardiogenic shock against the background of a heart attack;
- heart rhythm disturbance;
- dehydration;
- blockage of the pulmonary arteries;
- blood poisoning;
- aneurysm.
Low blood pressure values during the rehabilitation period indicate progression of the pathology. The prognosis in this case is extremely unfavorable, this applies to both recovery and human life. A decrease in blood pressure can occur against the background of regular use of hypertensive drugs that were prescribed to the patient even before the stroke developed.
But if the reason for this is not drug treatment, then this is a signal that the body is unable to independently regulate blood pressure as a result of impaired cerebral blood circulation. Medical statistics show that severe hypotension during the first few days after a stroke causes the death of the patient.
What are stroke warning signs?
The next step, and this is by no means a ringing bell, but a real ringing of the bell, is the development of a transient ischemic attack (TIA) or transient cerebrovascular accidents.
Clinically, the pathology is manifested by dizziness and headaches. They can occur suddenly, or they can precede for several days the main symptom of the disease, which is
The following symptoms are also characteristic:
- short-term weakness in the arm and leg on one side of the body,
- short-term loss of vision or speech,
- sudden transient global amnesia - loss of short-term memory for events preceding and accompanying TIA, lasting up to a day. At the same time, long-term memory (usually for events a week ago before the attack and beyond) is preserved.
30−50% of people who have suffered a short-term cerebrovascular accident within five years develop a stroke, so they require a comprehensive examination and follow-up by a neurologist.
Causes of blood pressure surges
A sharp fluctuation in blood pressure after a stroke occurs when the organs and systems of the body are unable to perform their functions. Most often it is the brain that is affected. Against the background of unstable blood pressure, both cardiac and peripheral circulation worsens, and the destruction of the walls of blood vessels also occurs. The patient develops an acute form of atherosclerosis. The development of recurrent strokes cannot be ruled out.
The main danger lies not in the increase or decrease in pressure, but in its constant fluctuation
The leading causes of sudden changes in blood pressure that occur after a stroke are:
- disturbances in the functioning of the central nervous system;
- low mobility of the vasomotor center;
- high blood sugar levels;
- hormonal imbalance;
- changes in the electrolyte composition of the blood.
Important! With a hemorrhagic stroke, the risk of developing a second stroke is high. This usually happens on the fifth or sixth day after the first blow.
How does cardioembolic stroke develop?
The ischemic ones themselves - in contrast to the main cause that caused the blockage of the artery - are divided into atherosclerotic and cardioembolic. Atherosclerotic - the most common: a plaque located in the carotid, vertebral or one of the intracerebral arteries ruptures, its fragments rush to the brain, and then blood clots try to “patch” the site of the formed defect, but in fact they only worsen the situation.
It’s a different story when a blood clot came from the heart cavity. Why did he appear there? Most often, against the background of the development of arrhythmia, for example, atrial fibrillation, when the atria begin to contract not measuredly, but chaotically, like a butter churn, churning stagnant blood. Sometimes, when a post-infarction aneurysm develops in the heart after a heart attack, a large blood clot can form unnoticed in its cavity. Infectious damage to the valves - infective endocarditis is also often complicated by the separation of weakly fixed microbial vegetations from the valve and the development of cardioembolic stroke.
Stroke in hypotensive patients
The development of a stroke is also possible with low blood pressure (in people suffering from hypotension). The formation of pathology is due to the body’s inability to independently eliminate the impending blow. A stroke in hypotensive patients can be triggered by features of a person’s lifestyle, stressful situations, disturbances in the functioning of internal organs and systems as a whole, and the use of antihypertensive medications.
The cause of stroke development against the background of hypotension can be:
- a sharp increase in blood pressure - occurs as a result of severe stress, overwork, as a side effect of the drug;
- rupture of an aneurysm - can be triggered by lifting weights, staying in a prolonged inclined position in hot rooms or under the open sun - a violation of the integrity of the vessel occurs as a result of overstrain;
- bleeding disorder - in this case, the likelihood of blood clots and blockage of blood vessels in the brain increases.
In the chronic form of hypotension, the likelihood of developing an ischemic stroke increases significantly with age. In the presence of cardiovascular pathologies, the risk of hemodynamic stroke increases. This is a subtype of the ischemic form, caused by circulatory decompensation. Its cause may be:
- atrioventricular block;
- myocardial infarction;
- weak sinus syndrome;
- atrial fibrillation.
Parkinson's disease is often accompanied by hypotensive crises, which, in turn, can cause the development of hemodynamic stroke. In hypotensive patients, signs indicating the formation of a hemorrhagic form of stroke are almost completely absent.
The condition is characterized by a slow onset and a long period of persistence of symptoms of brain damage with low blood pressure. The patient does not experience loss of consciousness or headaches. But almost all the precursors are typical for ischemic stroke. Most often, symptoms occur at night or in the morning.
Why does a stroke occur?
To make it clearer, let’s immediately divide all strokes into two fundamentally different types: ischemic and hemorrhagic. The first is associated with a violation of blood flow to a certain area of the brain; according to the mechanism of development, it resembles myocardial infarction. The second develops as a result of hemorrhage in the brain, most often due to the rupture of an aneurysm (local dilation of the vessel with thinning of the wall) of one of the cerebral arteries. This pathology is often congenital, and aneurysms can also form during life as a complication of hypertension. Hemorrhagic strokes are less common and are more severe than ischemic strokes.
First aid
If you or your relatives suspect symptoms characteristic of a hypertensive crisis or stroke, the first thing to do is call an ambulance. The algorithm of actions will be as follows:
- Call emergency medical services.
- Place the victim in a horizontal position with the head end raised;
- Unfasten tight clothing to allow oxygen to enter;
- Open the window and ventilate the room, covering the patient;
- Try to calm down or reassure the victim;
- Try to move less;
- If there are blood pressure medications nearby, take them.