Sympatho-adrenal crisis is one of the manifestations of panic disorder. Repeated panic attacks significantly complicate the life of a person experiencing such conditions. And, although they are not a direct threat to life, the consequences for the social and psychological spheres of the patient’s life can be very significant.
For a long time, until the end of the twentieth century, the main attention in medicine was paid to phobias and generalized anxiety disorder. At a time when pathologies such as stress, panic and obsessive-compulsive disorders of the nervous system were little studied. Accordingly, the treatment of these conditions did not bring the desired effect.
But over the last quarter of a century, the situation has changed - as a result of research, it has become clear that such conditions are much more common than previously thought. The reasons behind their occurrence have been discovered, and new treatment methods have been developed (EMDR therapy, short-term strategic and cognitive behavioral therapy, Ericksonian hypnosis). Therefore, his results have improved significantly.
Classification of vegetative-vascular crises
The duration and course of paroxysms (attacks) are individual - each has its own. The longer they last and the more often they occur, the more severe the disease.
Seizures are characterized by manifestations of certain physical sensations (symptoms) - pain of various localizations, fluctuations in body temperature, dizziness, a state of dysfunction of internal organs, and others. This is due to disruption of the functioning of parts of the autonomic nervous system (ANS).
In accordance with this, crises are divided into:
- By severity;
- According to clinical and pathogenetic indicators (according to clinical manifestations and parts of the nervous system, the disruption of which caused the pathology).
Division of panic attacks by severity
- Mild degree - attacks last no more than 15 minutes, are expressed by a small number of symptoms, have vegetative shifts within normal fluctuations.
- Moderate severity - duration from 15 minutes to an hour, pronounced changes in the vegetative nature, the presence of various symptoms: a feeling of anxiety, fear. After the attack, severe asthenia is observed (severe weakness, lack of concentration, muscle pain, irritability, headache, dyspepsia, dizziness). It can last up to one and a half days.
- Severe degree - lasts more than an hour, is accompanied by significantly pronounced autonomic disorders, a large number of symptoms, including tonic convulsions, chill-like hyperkinesis (feeling of internal trembling, unexpected chills, accompanied by the appearance of so-called “goose bumps” and internal tension), a feeling of fear. Asthenia develops quickly and can last up to 3–4 days.
Clinical and pathogenetic classification of crises in VSD
- Sympathetic-adrenal crisis (develops as a consequence of the predominance of one of the parts of the nervous system over the other, namely the sympathetic over the parasympathetic).
The pathology is characterized by manifestations of panic anxiety, chills, lack of air, numbness of the limbs, lips and tongue, tachycardia (rapid heartbeat), a feeling of pain in the heart, tinnitus, and blurred vision.
During the examination, the doctor notes: piloerection (the appearance of “goose bumps”), trembling (tremor) of the lips, hands and eyelids, a slight rise in body temperature, as well as a slight increase in blood pressure.
The attack may stop unexpectedly, accompanied by copious urination (the urine is light and has a low relative density). Often, the withdrawal period can last for several hours or even days, accompanied by severe symptoms of asthenia.
Sympatho-adrenal crisis should not be confused with the term adrenal crisis. The latter manifests itself in Addison's disease (as a manifestation of acute insufficiency of the adrenal cortex), its symptoms will be discussed further.
- Parasympathetic (vago-insular). It develops as a consequence of disturbances in the activity of the parasympathetic nervous system.
During a vagoinsular crisis, the following are recorded: profuse salivation, pain in the abdomen, nausea, drowsiness, dizziness, fear of death caused by cardiac arrest or suffocation, a feeling of weakness and weakness, hunger, increased pain sensitivity of different parts of the body.
On examination, the following are noted: pallor of the face (occasionally redness), decreased blood pressure, wet and cold palms, flatulence (bloating), increased intestinal motility, bradycardia, hyperkinesis or pseudoparalysis of the limbs, decreased tendon reflexes and decreased daily urination.
- Mixed vegetative-vascular crisis.
It is characterized by the simultaneous (rather than sequential) manifestation of symptoms characteristic of excitation of the sympathetic and parasympathetic departments, the inclusion of symptoms characteristic of other types of attacks and their repeated alternation.
- Fainting-tetanic (hysteria-like) crisis.
In fact, it is one of the varieties of a hysterical attack.
The clinical picture is characterized by increased blood pressure, demonstrative behavior, tachycardia, increased sweating, signs of convulsive readiness, trembling, local tonic convulsions, and sometimes even generalized tetany (convulsions).
- Vestibulopathic attack.
Severe changes in blood pressure, severe ataxia, dizziness, nausea, and vomiting occur.
- Pseudo-adysonic crisis.
It can be classified as one of the subtypes of vagal-insular crisis, but with a predominance in the clinical picture of symptoms similar to the manifestation of an adysonic (adrenal) crisis. These include: low blood pressure, nausea, adynamia, weakness, abdominal pain, gastrointestinal upset.
- Migraine-like (cluster) vegetative-vascular crisis.
Associated with the manifestation of an acute disorder of the tone of various vessels of the spinal cord.
Characterized by very sharp, attack-like cephalgia (headaches), possibly a slight increase in blood pressure.
Vegetovascular dystonia with panic attacks
A panic attack is an episodic manifestation of anxiety that begins suddenly for no apparent reason in patients suffering from VSD. The attacks last from a minute and can last an hour. Sometimes panic attacks occur periodically several times a week, or may not make themselves felt for a long time.
A panic attack during VSD is manifested by extremely pronounced anxiety (panic). It is accompanied by fear of death, self-control, loss of consciousness, fear of going crazy and pronounced vegetative symptoms:
- Increased sweating;
- Accelerated heartbeat;
- Chest pain;
- Nausea;
- Feeling hot or chilly;
- Dizziness;
- Discomfort in the abdomen;
- Trembling hands.
The symptoms of a panic attack can vary from person to person. The attack begins suddenly and lasts from several minutes to several hours. Panic attacks can be associated with a certain situation, environment, place, and arise spontaneously, regardless of external circumstances. The key difference between isolated panic attacks in VSD and panic disorder is the absence of the formation of fear of anticipation of a new panic attack and protective behavior - avoiding situations and places in which a panic attack has already occurred.
Physiology and main causes of VSD attacks
According to research in the field of psychotherapy, almost 2.5% of all people on the planet suffer from panic disorder. And in highly developed countries, for example, in America, more than 50% of patients undergo annual treatment from a psychotherapist. Panic attacks are often combined with agoraphobia (fear of being in public places). In this case, the cause of agoraphobia is considered to be a panic attack.
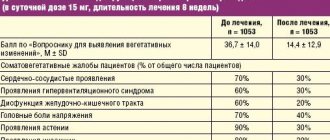
For a clearer picture of the population’s susceptibility to panic disorders, the following table can be given:
| Distribution for 1 year, % | Ratio by gender (women to men) | Age at onset of illness (years) | Spread to immediate family | |
| Panic attacks | 2,3 | 5:2 | 15-35 | High |
Among psychotherapists, the following theories of the development of panic disorder are most popular:
- Biological theory.
- Cognitive.
Biological theory
It began to take shape in the 60s of the last century. When it was discovered that patients suffering from this disease are helped not by strong sleeping pills (benzodiazepines), but by drugs used to eliminate the symptoms of depressive disorder (antidepressants).
Based on the knowledge that antidepressants cause changes in the activity of norepinephrine and serotonin (mediators that facilitate the transmission of signals between neurons in the brain), it was assumed that panic crises could be caused by the abnormal activity of these substances.
It was possible to prove that patients have inconsistent activity of this mediator. An experiment was conducted in which the locus coeruleus (an area of the brain involved in the regulation of emotions, containing a large number of neurons that use norepinephrine) was electrically stimulated in monkeys. At the same time, they recorded reactions that were very reminiscent of panic.
Another experiment was conducted in which a patient was induced to panic by injecting him with a substance that affected the activity of norepinephrine.
Her flaws
However, it was not possible to determine what the real cause of the pathology was. What kind of activity contributes to this: increased or decreased, or is it another type of disturbance associated with norepinephrine. In addition, it was possible to determine that it is not the only mediator involved in the development of the disease.
It has not been possible to determine why people are susceptible to this biological anomaly. An option with a genetic predisposition was considered. But then, the susceptibility to attacks should increase with the degree of relatedness. But research results do not show such a clear trend.
The results of treatment with antidepressants show improvement in 80% of cases, 40% of patients experience significant improvement or complete recovery. In this case, the improvement lasts up to 4 years or more. But, in many situations, the use of medications alone is not enough. The most effective is its simultaneous combination with the help of a qualified psychotherapist.
Cognitive theory (from the Latin “cognitio” - knowledge)
It appeared not very long ago and has already become popular. It is based on the assertion that people susceptible to the psychological anomaly in question are highly sensitive to certain sensations in their body (tight breathing, intense anger, excitement) and they misperceive them, interpreting them as signs of a disease. Without even making an attempt to understand the true cause of their feelings, they overwhelm themselves more and more, only contributing to the development of neurosis. And assumptions that such a condition may recur only accelerate the onset of repeated panic attacks.
Why can a person develop such neuroses?
- Poorly developed ability to deal with stress.
- Lack of social support.
- Possible psychological problems in childhood (lack of control, inadequate reaction of parents to the child’s psychological problems).
- Hereditary chronic diseases.
In accordance with the cognitive theory, people with an increased level of anxiety sensitivity, which is determined by a doctor conducting special (biological) tests, are more susceptible to vegetative-vascular crises. This is a special procedure used to induce a panic attack in patients by fulfilling certain requirements, directly under the supervision of a psychotherapist.
It has been scientifically proven that cognitive therapy is significantly more effective than drug treatment for the treatment of panic attacks. And, although many practitioners have tried to combine the two, it is not yet well understood whether this is more effective than using cognitive therapy alone.
Migraine-like crisis
Migraine-like crisis - paroxysmal sharp headaches, nausea, vomiting, increased blood pressure, dizziness.
Emergency care for a migraine-like crisis
- Inject intramuscularly in one syringe:
- 50% solution of metamizole sodium (analgin) 0.1 ml/year
- 2.5% solution of promethazine (pipolfen) 0.01 ml/kg
- 2% papaverine solution 0.1 ml/year of life.
- Inject intramuscularly or intravenously 1% solution of furosemide (Lasix) 0.1-0.2 ml/kg.
- Inject intramuscularly 0.5% solution of metoclopramide (cerucal) 0.01 ml/kg.
- For severe bronchospasm - intravenously 2.4% slow aminophylline 0.1 ml/kg.
Factors contributing to the development of vegetative crises
VSD with panic attacks very often develops from an asymptomatic or mild course. Therefore, the presence of any of the above factors is a reason to pay more attention to your health:
- The presence of malfunctions in the functioning of the endocrine glands (endocrine system).
- Concussions, birth injuries, disorders of the central nervous system.
- The development of osteochondrosis, the occurrence of tumors and infectious foci, as a consequence of the development of disorders of the ANS (autonomic nervous system).
- Physiological hormonal changes in the body (occurs during puberty in adolescents, pregnancy, menopause). This point requires paying attention to the table of population susceptibility to panic disorders, namely, to the section “Age at onset of illness.”
However, the presence of a background condition of the disease cannot be the only reason for the development of a crisis. This requires additional factors that act as a catalyst. Such catalysts can be: mental and physical fatigue, stress, previous surgery, exposure to medications, severe forms of infectious diseases.
Vagotonic crisis
Vagotonic (parasympathetic or vagoinsular) crisis - manifested by complaints of weakness, sweating, vomiting, headache, abdominal pain, drooling. Characterized by hypothermia, low blood pressure, bradycardia, increased peristalsis, flatulence, oliguria, and a tendency to faint. More typical for younger children.
Emergency care for vagotonic crisis
- Put the child to bed, warm him, provide access to fresh air.
- Ingestion of Eleutherococcus tincture 1 drop/year of life.
- Inject subcutaneously 10% caffeine solution 0.1 ml/year of life.
- In case of severe bradycardia or intractable crisis, administer intramuscularly 0.1% atropine solution 0.1 ml/year of life.
Symptoms
The symptoms accompanying a sympatho-adrenal crisis are directly related to the release of too much adrenaline that occurs during it.
- Panic anxiety, complaints of fear of death, inexplicable melancholy.
- Regarding the heart: fading and interruptions, pain, rapid heartbeat.
- Feeling short of air.
- Throbbing headache.
- Chills, trembling.
- Visual impairment.
- Noise in ears.
- Numbness of lips, tongue, limbs.
- Hallucinations, disorientation.
Sympathetic-adrenal crisis refers to the hypertensive type of VSD and is accompanied by a sudden increase in blood pressure, up to levels of 140 mmHg. Its name (sympatho-adrenal) is similar to the name of the crisis that occurs in Addison's disease - adrenal crisis, the symptoms of which are similar to the manifestations of a pseudo-adrenal attack, which must be taken into account when making a diagnosis. For comparison, below is a list of symptoms of adrenal crisis:
- On the part of the heart - a feeling of interruptions in work, rhythm disturbances.
- Hyperhidrosis (excessive sweating).
- Sudden decrease in blood pressure, chills, cold extremities.
- Sudden severe weakness.
- Gastrointestinal disturbances, vomiting, nausea, dyspepsia.
- Severe pain in the abdominal area.
- Oliguria (decreased urine output).
- Hallucinations, fainting, speech problems.
- Development of a coma.
But unlike an adrenal crisis, which is associated with acute adrenal insufficiency and sometimes leads to the death of the patient, a sympatho-adrenal crisis does not pose a direct threat to human life. And after the attack ends, its symptoms disappear.
In addition to the already mentioned hypertensive type of VSD, a hypotensive type may also occur. As the name suggests, its main feature is to lower blood pressure.
Next, we will consider the symptoms that are most characteristic of vegetative-vascular dystonia and manifest themselves, including during attacks.
Symptoms characteristic of VSD
Cephalgia (headache) with autonomic disorders occurs in 53–88% of cases and may differ in location. The impetus for its occurrence can be changes in weather and magnetic field, overwork, premenstrual syndrome, alcohol.
Vasodepressor syncope is a consequence of periodically manifested vasodilation (constriction) of peripheral vessels, resulting in a decrease in the return of venous blood to the heart muscle and the development of brain hypoxia. It can be triggered by acute pain, strong emotions, or increased ambient temperature.
Vestibulopathies are recorded in almost 27% of patients, manifesting themselves in the form of temporary visual impairment, pulsating tinnitus, non-systemic dizziness, and in 5% of cases they can even reach the level of vestibular crisis.
Abdominal vascular dystonia - manifested by paroxysmal pain in the abdominal area, increased gas formation, nausea, constipation or diarrhea.
Peripheral angiodystonic disorders are rare (up to 5.2%), characterized by paroxysmal (attack-like) pain, asymmetry of blood pressure, coldness, paleness or blue discoloration of the extremities. Disorders can be a consequence of both atonic and spastic reactions of the arteries of the lower extremities.
The most characteristic symptom accompanying all types of attacks is manifestations of fear, anxiety or panic. Which gradually fade away, along with the extinction of the attack.
The severity of symptoms in VSD directly depends on the circulatory disorder in the brain. The most complete picture of a decrease or increase in cerebral vascular tone is provided by rheoencephalography (REG). It is characteristic that REG changes persist even with long-term (many years) observation.
Preventive actions
There is no specific prevention that will help prevent the formation of the disease. Although there are recommendations on how to help the body quickly overcome attacks. To do this you will need:
- maintaining a healthy lifestyle, giving up alcohol;
- in the moments between attacks, you can take folk remedies that have a sedative effect (valerian, peony, motherwort in the form of tincture);
- Periodically visit a psychiatrist to develop stress resistance.
If you wish, you can overcome an attack of vegetative crisis. However, this will require strict adherence to your doctor's advice. Timely therapy is a serious prerequisite for eliminating the problem.
To undergo diagnostics and prescribe a course of treatment, contact our medical (formerly NDC) on Gakkelevskaya 33. Click the “SIGN UP” button, get advice from our specialists and come to us. We will help you cope with the disease.
Diagnostic features
To make a correct diagnosis during vegetative-vascular crises, it is necessary to act by excluding clinical phantoms, such as:
- Hypoglycemic coma.
- An attack of bronchial asthma.
- Cardiogenic shock.
- Addisonian crisis.
- Acute abdominal pathology.
- Hypertensive (including pheochrocytoma) crisis.
- Tetany.
Therefore, when identifying clinical signs, it is necessary to monitor blood pressure, conduct an ECG, urine test (catecholamines), clinical blood test, biochemical blood test (basic acid, urea, glucose, electrolytes), express glycemic analysis. If necessary, additional studies are carried out (introscopic, hormonal and others).
In psychoneurology, vegetative-vascular crisis and panic attack are considered synonymous. According to the American DSM-IV system, the diagnosis of a panic attack is considered established when at least 4 panic attacks occur within 4 weeks and there is a fear of repeated manifestations.
You can independently distinguish the manifestation of an attack of VSD from the above diseases on the basis of:
- Again, the analyzes carried out earlier.
- Manifestations of feelings of fear, anxiety, disappearing after the end of the attack.
- Manifestations of symptoms of heart disease that disappear after an attack and do not appear outside of it (the attack), including during physical activity.
- A certain frequency of manifestation (from 4 or more per month), with a characteristic, individual clinical picture.