Panic attacks at night are sudden attacks of anxiety and fear (most often fear of death) that occur at night or during sleep and are accompanied by severe autonomic symptoms - palpitations, a feeling of shortness of breath, heavy sweating, dizziness. Regular panic attacks are called panic disorder.
The causes of panic attacks during sleep are still unknown. It is believed that they are based on a disruption of the functioning of biologically active substances (norepinephrine and gamma-aminobutyric acid). In 15% of cases, there is a hereditary predisposition when similar conditions occur in close relatives.
A psychotherapist diagnoses and treats panic attacks.
Provoking factors include:
- severe stress, conflicts, childhood experiences and psychological trauma
- abuse of strong coffee, alcohol
- excessive physical activity, mental stress
- hormonal metabolism disorders, injuries and previous infectious diseases of the brain
Less common are panic attacks with two or three symptoms, the so-called minor attacks. They are not accompanied by a feeling of fear and imitate other diseases - heart pathology, dysfunction of the endocrine glands (for example, the thyroid gland).
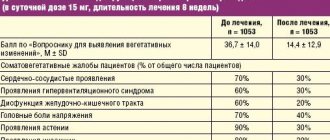
Such patients have been observed and treated for a long time by therapists, cardiologists and neurologists with a diagnosis of VSD or neurocirculatory dystonia. If treatment from other specialists helps poorly or has no effect at all, you need to consult a psychotherapist.
Panic attacks during sleep
Panic attacks differ from nightmares in the time they occur. Night dreams occur in the second half of the night during the REM sleep phase; a person often remembers what he dreamed. Nocturnal panic attacks are not associated with dreams and most often develop from twelve at night to four in the morning.
Panic attacks during sleep have serious negative consequences for a person's health and overall well-being. Attacks prevent the body from resting, disrupt falling asleep, and lead to lack of sleep and constant fatigue.
Important
Panic attacks at night are impossible to forget. A person begins to live in constant fear that this will happen again, and is afraid to go to bed.
Repeated attacks of anxiety and fear at night should alert you and cause you to contact a specialist. Over time, attacks occur more frequently and their duration increases. For example, if at the beginning of the disease there are 1-2 panic episodes every two to three months, then without treatment, attacks can develop daily.
Sleep disorders. Continuation
Fatal familial insomnia is characterized by insomnia, which is accompanied by a rise in blood pressure, tachycardia, hyperhidrosis and hyperkinesis (tremor, myoclonus). Sometimes psychotic disorders are added. The prognosis is unfavorable. The disorder is one of hereditary causes.
Delayed sleep-wake cycle syndrome is thought to occur when there is a combination of delayed sleep onset and equally slow awakening. In general, the norm of full daily sleep is reduced. Over time, increasing sleep deficit can have corresponding consequences.
Accelerated sleep-wake cycle syndrome is characterized by falling asleep too quickly and waking up too quickly from sleep, as well as impaired sleep quality. Patients report that they do not fall asleep as usual, but “fall into sleep,” and do not wake up from sleep, but “come to their senses,” waking up with the feeling that they have “awakened from unconsciousness.” There are no dreams. Sleep, according to patients’ descriptions, is “heavy”, “stupefying”, and does not lead to a feeling of rest or vigor. Waking patients can be difficult. Children may experience urinary and fecal incontinence. Some researchers believe that in such cases we are talking about too deep sleep - profundosomnia (Buyanov, 1985). The feeling of instantly falling asleep and equally rapid awakening may apparently indicate a loss of the sense of sleep, confined to the first phases of slow-wave sleep.
Sleep incontinence is characterized by the breakdown of normal sleep-wake cycles into smaller fragments lasting 1-2 hours or less, as well as an imbalance in the various phases of sleep. REM sleep appears to be the most affected. The disorder occurs in elderly and senile patients. Clinically, it manifests itself as a continuous alternation of short periods of sleep and wakefulness.
The inversion of the sleep formula is manifested by sleep during the day and wakefulness at night. Such patients fall asleep in the morning and wake up in the evening, closer to night. This disorder is especially common in schizophrenia. Daytime stimuli seem to lose their former meaning for patients; they are closed in on themselves, they are guided exclusively by personal interests. Other patients, especially those suffering from depression, report that the worries of the day not only do not activate them, as it was before, but, on the contrary, suppress them and are perceived as overwhelming. Only on weekends and on vacation do they feel better.
At night, according to the stories of some patients, they seem to take a break from the oppression of responsibilities, gain access to what they personally like best, they do household chores with pleasure, read something with interest, write, willingly watch TV, listen and watch audio and video recordings. It is also possible that the inversion of the sleep formula is caused not only by autism, depression, but also by a violation of the circadian rhythm of activity. The disorder sometimes resembles the rhythm of life of patients with catatonia, who fall into a state of stupor during the daytime, and at night they seem to disinhibit and behave more actively and adequately. Sometimes an inversion of the formula occurs during the active period of the disease and then persists in remission, sometimes for many subsequent years.
Much more common is a shift in the sleep formula, when patients fall asleep late at night and wake up during the day, before noon or afternoon. The time of greatest activity occurs in some patients in the late evening and night hours. The main reason for the inversion and shift of the sleep formula is, apparently, a disruption of the “biological clock”, that is, a disruption of the daily circadian rhythm of activity.
A change in the sleep formula that is similar to the mentioned disorders and has become habitual is sometimes characteristic of creative people, apparently “night owls” by nature, who prefer to work at night, thereby distracting themselves from the immediate concerns of the day. This is how, for example, F.M. Dostoevsky and O'Henry worked. F.M. Dostoevsky, often staying up until the morning, drank a lot of iced tea. O'Henry also preferred to write at night. When asked about his creative method, he jokingly advised: “It’s very simple. In the evening, take clean paper, a pen and a bottle of whiskey. And by morning the story is ready.”
In addition, there are professions that require high work activity, mainly at night. Persons employed in such professions, on vacation and in retirement, may stay awake mainly at late times if they have not been able to adapt to the new rhythm of life for them. A sleep formula disorder may also be associated with reasons such as puberty crisis, menstruation, the onset of menopause, i.e., psychoendocrine disorders.
The increase in the sleep-wake cycle is believed to be due to the fact that the duration of this cycle, for unknown reasons, exceeds 24 hours. As a result, subject to the limitations of life circumstances, the individual does not get enough sleep, and the sleep deficit gradually increases towards the end of the week. On weekends, the patient should therefore get enough sleep if he feels the effects of sleep deprivation. The duration of the sleep-wake cycle is usually formed in early childhood.
Chronic sleep deprivation is characterized by limited sleep time due to lifestyle factors. A typical example of a violation is represented by people with operator professions, in particular managers, who, in the pursuit of success, are often forced to sleep much less time than the body requires. In addition to the phenomena of increasing asthenia, which inevitably accompany such a lifestyle, patients often experience persistent disturbances in sleep, attention, memory and performance that do not go away after vacation and rest, and are sometimes very difficult to treat.
Wolf's sleep externally manifests itself as chronic absolute insomnia. Rare cases of the disorder have been described when patients do not sleep for several years (up to 10 years or more). According to some reports, the disorder can occur as a result of a cerebral concussion. The EEG pattern is found to show that patients do sleep, but in very short and frequent episodes, which are not noticed by either the patients themselves or the people around them, but which are quite sufficient to maintain activity at a satisfactory level for a long time .
Somnambulism (sleepwalking, sleepwalking) usually manifests itself as single episodes during the night and short-term episodes of incomplete awakening from sleep. This disorder is the opposite of sleep paralysis. The difference is that in states of sleep paralysis, the psychic self appears to be awake, while the somatic self remains asleep. With sleepwalking, the opposite picture is observed. The frequency of sleep paralysis and somnambulism is comparable. The term “somnambulism” is not entirely accurate, since in addition to sleepwalking, patients often perform other, sometimes very complex, automated actions. The name "sleepwalking" comes from the fact that some patients actually sleepwalk during the full moon. The state of consciousness of patients during sleepwalking is usually regarded as twilight stupor, very close to what is observed in states of ambulatory automatism in patients with epilepsy.
The disorder first appears around the age of 5–6 years. More common in males. Approximately 15% of children experience it as a single episode. In some patients, the disorder lasts until adolescence, then disappears. In a number of patients it is observed in adulthood, and sometimes appears for the first time at this age. It is rare in old and senile age. Episodes of sleepwalking occur in the 3rd–4th phase of slow-wave sleep, usually in the first third of the night. Their duration usually does not exceed 30 minutes.
In typical cases, sleepwalkers get out of bed at approximately the same time. Often this is preceded by exciting impressions. Patients' activity usually comes down to walking around the house, after which they return to bed independently or with someone's help and continue to sleep. They walk silently, noiselessly, aimlessly, with their eyes open, so that they avoid obstacles in their path without any problems. Often the same, stereotypical actions are performed, but more often these actions are diversified. The patients' gaze is directed as if to infinity.
They do not react to the speech of others, do not maintain eye contact, and do not recognize loved ones or acquaintances. The patient's face does not express anything, emotional manifestations are delayed. The next morning, when patients wake up, they do not remember walking in their sleep and for the most part feel normal. Nor do they report that they had any dream immediately before or during sleepwalking. In abortive cases of somnambulism, the actions are reduced to the fact that patients sit up or jump out of bed, they can get up and urinate or recover.
It is not so rare that the actions of patients during sleepwalking are quite complex. So, they can get dressed, wash their face and hands, brush their teeth, pack some things for the trip, open the door and go outside. Some patients move pieces of furniture from place to place, hide behind curtains or in other hidden places in the house, look at themselves in the mirror, light the stove, turn on a gas or electric stove, put a kettle or pan on it, look out of the window into the street and for some time They seem to be watching something, reading a newspaper or a book, trying to write something. There are patients who, when going outside, climb poles and trees, walk along the edge of a balcony, cornice, roof, which they could not do during the day even if they wanted to.
There are rare cases of sleepwalking during which patients can perform sexual intercourse and then not remember anything about it. Occasionally other cases are identified. So, one of the patients rolled up a carpet like a log and carried it on his shoulder around the apartment. Several times he hid certain things in his sleep in such a way that during the day he could hardly find or remove them. Another patient with ritual compulsions during the day reproduced them during sleepwalking. He sniffed repeatedly, clenched and unclenched his hands, turned the light on and off, brought a spoon to his mouth several times in a row and immediately pulled it away, etc.
It happens that patients during sleepwalking commit acts of self-harm and suicide attempts. One of the patients, a young man, self-harmed several times with a knife in the elbow area. Another hammered a nail into the wall, tied a rope to it, made a noose, stuck his head through it and tightened it around his neck, at which time he came to his senses. The third patient, getting out of bed in his sleep, closed the damper in the stove and returned back to bed. He woke up lying at the door open to the street, when he greedily inhaled fresh air. Another patient woke up from suffocation to find his hand squeezing his own throat.
Some patients demonstrate mobility skills: riding a bicycle, motorcycle, or even driving a car. Relatively rarely, patients run in their sleep, sometimes along a single trajectory. There are cases of a combination of somnambulism and sleep talking. So, the patient went out into the street in a dream, made a large circle and at the same time swore loudly. It happens that patients answer questions from others or talk as if with an imaginary interlocutor.
In addition to varying degrees of complexity of actions during sleep, all cases of somnambulism can apparently be divided into two types. In the first of them, actions of a closed cycle are observed. Patients at the beginning of the episode get out of bed, do something, and then return to bed on their own. In the second case, patients seem to forget to go back, waking up on their own somewhere in the course of their automated actions. Both can occur in the same patient.
Attempts by others to awaken somnambulists lead to different results. Apparently, in most cases they can still be woken up, and this does not entail any sad consequences. Some of these patients the next morning can remember some impressions from what happened during sleepwalking. These are probably painful episodes during which the disturbance of consciousness was not particularly deep. Most likely, somnambulists of this kind are neurotic. Usually they walk in their sleep due to the fact that the day before they had to experience some exciting events.
By the way, there is an ingenious folk test for identifying such patients. It was customary to spread a wet rag next to the bed or at the threshold at night, and stepping on it with bare feet would wake up the sleepwalker. In some cases, attempts to wake the patient are unsuccessful. Perhaps this indicates a deeper clouding of consciousness. If the patient suffers from epilepsy, and sleepwalking is the equivalent of an epileptic seizure, then an attempt to awaken the patient may lead to secondary generalization of the seizure. The possibility of epileptic somnambulism may also be indicated by the stereotypical nature of actions during sleepwalking, more or less regular repetition of episodes of sleepwalking, and deterioration of well-being in the morning. The epileptic nature of sleepwalking is confirmed, according to various authors, no more often than 0.5–1% of all cases of the disorder.
Sleepwalking also occurs in patients with schizophrenia, depression, and many other painful forms, thereby indicating the fact of a nonspecific sleep disorder. Finally, there are cases of constitutional sleepwalking, that is, characteristic of patients with psychopathy and neuropathy. It is necessary to distinguish between sleepwalking itself and hysterical stupefaction that occurs during spontaneous or forced awakening from sleep. The most striking distinguishing feature of hysterical somnambulism is the expressiveness of the patients' actions, expression and emotions.
Sleep talk occurs quite often in patients with various painful forms and in different age groups. Patients talk at any time of the night, sometimes several times; they do this especially often when falling asleep, in the first half of the night and in the morning. Episodes of sleep talk are usually short-lived and last only a few seconds, although in a small proportion of cases they can last much longer. Often, instead of conversation, only vocalization is observed when patients moan, scream, moo, laugh, hum something, sob, or call out to someone.
In some cases, sleep talking comes down to short and unintelligible muttering. Some patients speak loudly and articulately about something personal, if those present manage to understand anything at all, and this conversation may also include invective, commands, orders, requests. There are patients who seem to be conducting a dialogue with someone, they seem to be asking someone or answering someone’s questions. Relatively few patients can respond to the speech of people present, for example, answer questions more or less meaningfully.
Typically, patients do not remember anything about the fact of sleep talking, although some of them know about it because they continue to talk when they wake up. In very rare cases, it is possible to establish that patients dreamed about something during dream talk. Here are some reports from the patients themselves: “I started talking in my sleep. My wife says that I speak so loudly that she wakes up. I speak clearly. I swear, swear, and also wave my arms and move my legs, as if walking... I begin to fall asleep, my eyes are still open, I look at my wife and, as she says, I’m talking all sorts of nonsense. Sometimes it’s like I’m communicating with someone at work.
I talk for a few minutes, then close my eyes and fall asleep. The next morning I myself don’t remember anything about it... They say that I often began to talk in my sleep. I sit up in bed and spout all kinds of nonsense, it’s impossible to understand. I speak much faster than usual. Sometimes, if they wake me up, I continue talking for a while. I remember that myself, I just forget what I said.” In relatively rare cases, sleep talking is a speech seizure of epilepsy. Sometimes sleep talking is accompanied by hypnic hallucinations, disturbances in self-perception, and intense fear. The patient reports: “Once when I was a child, I fell asleep with my eyes open. I saw some stones, a carpet, something else falling on me. I'm being crushed and I feel like I'm dying. At this time, as they told me, I screamed for help, to save me.”
Sleep intoxication (pathological drowsiness, drowsy delirium) occurs both during spontaneous and forced awakening from a state of deep, probably paradoxical, sleep. Described by Goodden in 1905. In typical cases, it manifests itself as twilight stupefaction with productive symptoms: illusions, hallucinations, delusions, intense affects of fear and anger, disturbances in orientation in place, time, space, situation and in one’s own personality, as well as inadequate, often aggressive behavior. Lasts within half an hour, rarely longer.
Occurs in the first half of the night, but can also occur in the morning. It is important to note that the disorder is not associated with alcohol consumption the day before. If the latter fact occurred, then the violation may be regarded as sleep intoxication. If there was an acute stressful situation the day before, the condition is regarded as affective intoxication by sleep. In some cases, the disorder is associated with nightmares, when patients for some time after waking up are under the impression of what they saw in a dream - this, in fact, is dream intoxication with sleep.
In the development of sleepy delirium, a constitutional predisposition appears to play some role. In the family history there are indications of disorders of the “epileptic circle”: somnambulism, fainting, migraine, states of dysphoria, dipsomania, other impulsive drives, psychopathic features of the epileptoid type. In general, we can say that this disorder occurs in a wide variety of disease states.
Let us present a number of observations of the state of sleep intoxication, arranged in order of increasing severity of its symptoms: “I wake up and for a while I can’t understand where my legs are, where my head is, in which direction the doors are located... I wake up and for a long time I can’t figure out whether it’s morning, afternoon or evening. I feel like I'm late for work. When I come to my senses, I understand that I had already come from work and went to bed for a nap... It happens that waking up from sleep is delayed. I’m lying and wondering where I am, if I’ve moved somewhere. I study the situation for a long time, remembering whether I did something wrong. This goes on for about 10-15 minutes.
Then I come to my senses and sometimes remember that before that I dreamed of something... Six months before this illness, I had a very bad dream with terrible details: knives, blood, corpses, killing my grandmother, and then sawing her in half. It seemed that everything was happening as in reality. I jumped out of bed, screaming, crying. It seemed to me that I was in some dark room, alone, surrounded by either people or some kind of ghosts. I didn’t notice how my brother came into my room and turned on the light. Apparently, he was telling me something, reassuring me. I don’t remember how much time passed before I came to my senses. Probably 10–20 minutes, I can’t say for sure. Only later did I realize that I was having a nightmare, but I was shaking for a long time, as if in a fever, before I calmed down.”
Here is a case of sleep intoxication in an officer who returned from a combat mission a month ago. Before this, he had more than once had difficult dreams with scenes of battles, with injuries and deaths of his comrades. As his wife said, the husband woke up in the middle of the night, jumped out of bed, quickly got dressed, tore a hunting rifle from the wall, and looked for ammunition for it. At the same time, he loudly gave commands to hide in cover, crawled from one window to another, briefly looked out into the street, and took aim. He didn’t pay attention to his wife’s address to him and didn’t seem to notice her. After 15–20 minutes I came to my senses, but did not calm down immediately. When his wife asked what was wrong with him, he answered that nothing had happened, everything was fine. Last evening, the patient met with his comrades, they all celebrated the date of death of a mutual friend and drank.
There are cases when patients in a sleepy intoxication commit crimes. All of the above observations show that there are different gradations of the severity of the state of sleep intoxication: from short-term loss of orientation and sleepwalking to a deep disorder in the form of twilight stupefaction.
Night terrors manifest themselves as short-term psychotic episodes occurring spontaneously during sleep with hallucinations, delusions, confusion, extremely intense fear, as well as psychomotor agitation followed by congenital amnesia. They can occur in schizophrenia, and sometimes act as a manifestation of latent or manifest epilepsy.
Sleep disturbances are often associated with other disorders. Let us mention the following:
- Bruxism is uncontrolled grinding of teeth during sleep. It is more often observed in the second phase of MDH sleep; impressions of this are not retained in memory. May cause damage to teeth. After waking up, some patients feel pain in the jaw area;
- epileptic seizures, so-called nocturnal epilepsy. Seizures usually occur in the first half of the night. There are no memories of seizures. There are patients who have seizures for a long time only in their sleep, so they know about their illness only from the words of others;
- myoclonus when falling asleep - lightning-fast shudders of the whole body at the very beginning of sleep. Patients often wake up and some of them remember what happened to them. Others experience dreams during the myoclonic jerk, for example with the feeling that they are “flying into an abyss”;
- noctural myoclonus - tonic contractions in some muscle groups in one leg or both legs while falling asleep. Patients remember how, when falling asleep, the leg “pulls”, at the same time they feel a “crawling sensation” in the calves of the legs, and sometimes pain. Sometimes there is a desire to move your leg. This disorder is a particular manifestation of restless legs syndrome. The final diagnosis can be made taking into account electromyography from the tibia and other muscles of the legs. Myoclonus can apparently also occur in the arm muscles, as well as in the masticatory muscles. Thus, waking up from unpleasant sensations in the hands or in the jaw area, patients discover, for example, clenched fists or clenching of the jaw so that for some time they cannot open their mouth;
- rocking the head back and forth when falling asleep or while sleeping. There may be body swaying. It has been established that the disorder occurs in phases 1–2 of MDH sleep, but occasionally appears during REM sleep;
- hereditary paralysis is characterized by a sudden loss of voluntary movement at the onset of sleep or upon awakening. This probably refers to the state of sleep paralysis;
- Vascular hemicrania is manifested by migraine attacks during sleep. May be combined with similar attacks while awake;
- impaired swallowing during sleep can lead to the accumulation of saliva in the oral cavity, and then aspiration of saliva into the respiratory tract, coughing, choking, awakening from sleep;
- sleep asthma is manifested by attacks of bronchospasm and suffocation during sleep;
- cardiovascular symptoms that appear during sleep are associated with increased heart rhythm disturbances, insufficient blood supply to the myocardium, as well as changes in blood pressure. The mentioned disorders can be both a consequence of sleep pathology and a cause of sleep disturbance, occurring at different stages of sleep;
- gastroesophageal reflux is characterized by the appearance during sleep of burning substernal pain, pain and a feeling of tightness in the sternum and/or a feeling of sourness in the mouth. Cough and mild respiratory distress may also occur;
- hemolysis or paroxysmal hemoglobinuria occurs in patients with chronic hemolytic anemia. During sleep, hemolysis and hemoglobinuria increase. Morning urine has a red-brown color;
- when falling asleep, during sleep and when waking up from sleep, other disturbances often occur: disturbances of sensory synthesis, phenomena of depersonalization and mental anesthesia, deceptions of perception, etc.
Treatment of sleep disorders is based on the painful form and the specific disease state in which they occur.
In particular, artificial sleep deprivation (for example, insomnia torture) is fraught with serious consequences. In most cases, patients refer to insomnia as insufficiency or inadequacy of sleep to varying degrees.
Back to contents
Treatment of nocturnal panic attacks
What to do to get rid of panic attacks in your sleep? Panic attacks are treated with a combination of psychotherapy and medications. Treatment has two main directions:
- Learn to stop attacks.
- Don't allow them to repeat.
You can stop an attack - that is, quickly stop it and get rid of symptoms - with medication or non-drug. At the request of the patient, the doctor can prescribe an anti-anxiety drug (anxiolytic), which in a few minutes brings the nervous system into a relaxed state.
The patient needs to learn non-drug relaxation techniques during individual psychotherapy sessions. These are thought control, self-hypnosis and proper breathing. Modern relaxation techniques include biofeedback therapy.
To get rid of panic attacks at night forever, you need to understand their causes. This may require several therapy sessions, and the patient must be willing to make efforts, change, listen carefully to the therapist and strictly follow his recommendations. In this case, the prognosis will be favorable.