Such a disease as epileptic seizures has been familiar to humanity since ancient times. This disease stood alongside leprosy, since it was little studied and practically could not be treated. But today, the science of neurophysiology has developed so much that it allows epilepsy to be diagnosed and successfully treated in the early stages.
Signs of epilepsy in a child
Epilepsy is a chronic neurological disease that can be caused by genetic predisposition or external factors.
The disease manifests itself approximately equally in both adults and children. However, in the latter it is more difficult to diagnose, because the child’s behavior is often more dynamic, which is associated with the normal physical activity of the growing organism. The main signs of childhood epilepsy:
1. Seizures . Can last from 10 seconds to 20 minutes. Characterized by tension in all muscle groups and trembling. In this case, there is a short-term cessation of breathing at the very beginning of the attack. The bladder often empties spontaneously. Upon completion of the attack, the child usually immediately falls asleep;
2. Absence seizures are seizures without convulsions. In such situations, the child becomes as if protected from the world. There is a blank look in the eyes. He does not respond to movements, light, or sounds. It is almost impossible to attract the baby's attention during such an attack, which lasts up to half a minute. Sometimes the eyelids tremble or the head falls back.
3. Attacks of atony . They are characterized by a sharp deterioration in the performance of the central nervous system, as a result of which consciousness is lost and all muscles relax. A standard attack is identical to fainting. Therefore, if the regular loss of a creature by a baby without good reason becomes commonplace, you should consult a doctor;
4. Spasms are involuntary muscle tension. They usually occur in children immediately after sleep. They are manifested by bringing the arms to the chest, bending the torso and head forward, straining and straightening the legs.
Alpha Rhythm
Neurologist-epileptologist, Ph.D. Kirillovskikh O. N.
Currently, frontal lobe epilepsy ranks second among symptomatic forms of epilepsy after temporal lobe epilepsy. The frontal regions of the human brain occupy first place in terms of area and variety of functions performed, which explains the variety of clinical manifestations in symptomatic frontal lobe epilepsy. The causes of symptomatic frontal lobe epilepsy are varied. It is the frontal regions of the brain that are most vulnerable to various traumatic brain injuries, which determines the most common frontal localization of epileptic foci in post-traumatic epilepsy in children and adults. In the frontal regions of the brain, various vascular aneurysms, cavernomas and malformations are most often localized - benign tumors that can cause the development of symptomatic frontal epilepsy . Various dysontogenetic (congenital) malformations of the brain, such as lisencephaly, pachygyria, microgyria, focal cortical dysplasia, are also most often localized in the frontal and frontotemporal regions of the brain.
Symptomatic frontal forms of epilepsy are divided into 3 main groups depending on the localization and functional load of those parts of the frontal cortex that are the source of epileptic activity (V. A. Karlov, 2010). These are epileptic seizures , the source of which is the following parts of the frontal cortex (Figure 1):
Fig 1. Topical diagnosis of the cerebral cortex.
- Motor cortex
- Premotor cortex
- Prefrontal cortex
The longest and most well-studied is the so-called Jacksonian epilepsy (JE), described by the outstanding Scottish neurologist John Jackson in 1870.
The epileptic focus in Jacksonian epilepsy is located in the projection motor cortex - a region of the frontal lobe of the brain located on the border with the parietal and temporal lobes, where the cortical centers of voluntary movements for all human muscle groups are localized. The clinical picture of this type of epilepsy consists of local convulsions that occur in certain parts of the limbs, then spreading to the entire half of the body (Jacksonian march), followed by loss of consciousness and a generalized convulsive seizure . According to Jackson's classic description, there are 3 directions of seizure propagation:
- Convulsions, occurring in the hand (I, II, fingers, forearm), cover the entire hand, moving to the facial muscles, then the lower limb.
- Cramps begin in the muscles of the face or tongue, then affect the arm or leg. Moreover, if the seizure is right-sided, then speech disturbances are noted.
- Cramps from the lower limb spread to the entire leg, then the arm and face.
If several seizures follow in a row, they usually leave behind weakness in the limbs, which is called Todd's epileptic paralysis. Jacksonian seizures are a common manifestation of cerebral diseases such as tumors and arteriovenous aneurysms, consequences of traumatic brain injuries and infectious lesions of the nervous system, therefore, in the event of such seizures, a more detailed examination of the patient is necessary, primarily MRI of the brain with contrast and examination of cerebral vessels. EEG is highly informative for Jacksonian epilepsy of any etiology; the frequency of false-negative results on waking EEG does not exceed 20%. EEG video monitoring in most cases provides a video recording of a seizure. Treatment of DE is often very difficult, although benign forms of the disease can also occur. In the case of pharmacoresistant forms of DE, a neurologist-epileptologist treats the patient in close collaboration with neurosurgeons and MRI diagnostic specialists to select the optimal treatment tactics.
Epileptic seizures, the source of which is the premotor cortex (Fig. 1), more often manifest themselves in the form of the so-called. adversive and/or postural seizures. An adverse epileptic seizure is a type of focal epileptic seizure that involves muscle groups that produce a combined rotation of the head and upper half of the body away from the epileptic focus. Typically, turning involves tonic movements of the trunk and opposite limbs to maintain balance, which leads to a so-called postural seizure, that is, a seizure in which the patient assumes a certain characteristic posture. One of the typical poses is the “fencing pose” with the arm contralateral to the focus tonically bent and raised upward with the head and eyes turned towards it (Fig. 2).
Rice. 2. “Fencer’s pose” in a child with postural adjuvant seizures with symptomatic frontal lobe epilepsy.
In addition, epileptic seizures of the premotor area include simple partial seizures with isolated disturbances of speech function - speech arrest.
The most diverse, numerous and difficult to diagnose group are epileptic seizures originating from the prefrontal cortex (Fig. 1). The following types of seizures are typical:
- With negative motor manifestations - hypomotor seizures - freezing, freezing (pseudo-absences and true absences), as well as falling.
- Hypermotor seizures - “pedaling”, “boxing”, chaotic movements of the body, rolling, crawling.
- Generalized convulsive, often serial or status.
Seizures in frontal lobe epilepsy have their own distinctive features.
Characteristic:
- Short term.
- Minimal or complete absence of postictal confusion.
- Fast secondary generalization.
- Pronounced motor manifestations, complex automatisms and gestures.
- Frequent falls of the patient during bilateral discharges.
Diagnosis of frontal lobe prefrontal epileptic seizures often presents significant difficulties. When the attacks are hypomotor (with minimal motor manifestations), occurring in the form of sudden falls without convulsions, differential diagnosis is carried out with various types of fainting. A common finding during neuroimaging during hypomotor seizures are post-traumatic or tumor foci in the mediobasal regions of the frontal lobe, as well as foci of focal cortical dysplasia (Fig. 3). EEG video monitoring of daytime (nighttime) sleep in most cases allows us to identify a focus of epileptiform activity, which is evidence of the epileptic nature of the attack.
Fig 3. Focal cortical dysplasia of the left frontal region.
Diagnosing hypermotor seizures is even more challenging. The structure of hypermotor seizures in frontal epilepsy may include screaming, pedaling movements of the legs, violent, chaotic movements of the body, sometimes rolling or crawling. The presence of such unusual manifestations of a seizure requires differential diagnosis with psychogenic (conversion, pseudoepileptic) seizures. The only reliable method of differential diagnosis is EEG video monitoring of sleep , and in most cases there is a need for EEG video monitoring of night sleep. Synchronous video recording of the electroencephalogram and the paroxysmal event itself makes it possible to register epileptiform activity preceding the attack, as well as specific changes in the EEG that occur after the attack. The EEG picture of an attack, as a rule, is distorted by movement artifacts due to the hypermotor nature of the attack. Decoding the EEG when recording a paroxysmal event in frontal epilepsy requires highly qualified and extensive experience of a neurologist-epileptologist, since EEG manifestations in frontal epilepsy are often minimally expressed, for example, in the form of desynchronization (flattening) of the main rhythm. (Figure 3A, 3B)
Rice. 3A. Patient S.A., 5 years old. Focal cortical dysplasia. Symptomatic focal frontal lobe epilepsy. Video-EEG monitoring during sleep recorded a focal motor attack with hyperkinetic automatisms. Ictal EEG (seizure onset) - the appearance of rhythmic alpha and theta activity bifrontally, but with a clear predominance in the left frontal and anterior vertex areas.
Rice. 3B. The same patient. Ictal EEG (continuation of a focal motor attack with hyperkinetic automatisms) - diffuse flattening of bioelectrical activity with the appearance of a large number of motor artifacts over time (with the appearance of hyperkinetic automatisms).
Thus, symptomatic frontal lobe epilepsy represents a large and heterogeneous group of different epileptic syndromes, presenting significant difficulties for diagnosis and treatment. Successful treatment of this complex form of epilepsy requires an integrated approach - modern diagnostic methods, including EEG video monitoring of night sleep and MRI study according to the epileptological protocol (link to the article on the possibilities of MRI in the diagnosis of epilepsy), as well as constant monitoring by a neurologist-epileptologist. When diagnosing focal changes of an organic nature, it is necessary to consider the possibility and advisability of neurosurgical treatment.
Childhood epilepsy - sources of the disease
Is epilepsy treated in children? Yes, rapid identification of risk factors makes it possible to stop attacks in the early stages.
Risk factors:
- brain tumors;
- past illnesses - encephalitis or meningitis;
- disturbances in the functioning of the liver and kidneys;
- imbalance of mineral metabolism in the body.
Symptomatic manifestations of epilepsy in children are more difficult to diagnose than in adults. It is generally accepted that this disease is always accompanied by seizures, but in the case of a child this is not always the case. For example, if your child suffers from frequent headaches or nightmares, this is a reason to go to the doctor and get diagnosed. The disease is diagnosed by undergoing magnetic resonance imaging (MRI).
Epileptic seizure: main differences from ordinary fainting.
- The reaction of the pupils - they stop constricting when interacting with directional light.
- Spontaneous uncontrollable seizures.
- Duration of the attack. If paroxysmal seizures last more than 5 minutes in a child and are repeated many times, and the break between them is less than an hour, this is a very alarming symptom. In this case, you should immediately seek medical help.
Types of disease
The following types of epilepsy are observed in patients of different age groups.
- Juvenile myoclonic epilepsy. Mostly occurs in teenagers. The attacks occur after waking up and are sometimes not accompanied by convulsions.
- Progressive myoclonic epilepsy. It is difficult to treat and can develop into a more complex and dangerous form of the disease throughout life.
- Symptomatic epilepsy. Older people suffer. The first signs of the disease may appear up to 30 years of age. The causes are head injuries and diseases of the nervous system. Due to the varied manifestations of the disease, it is difficult to diagnose as the symptoms can be misleading and the patient may be misdiagnosed even after a thorough examination.
- Temporal lobe epilepsy. Affects the temporal lobes of the brain. A common symptom is a state of “déjà vu.” This form of epilepsy also causes anxiety disorders, uncontrollable outbursts of anger and other emotional states.
- Frontal epilepsy. Symptoms vary and depend on which parts of the brain are affected. Affects the motor functions of the human body. The manifestations of this disease often do not cause concern. The patient may move his eyes and tongue rapidly, and stagnate. From the outside it may seem that a person is simply experiencing nervous excitement. At the same time, a person cannot organize his thoughts, experiences many emotions at the same time and cannot calm down or concentrate on one thing.
- Parietal epilepsy. It is quite rare. The symptom is visual disturbances or eye sensitivity to flashes of light. The eyes may move uncontrollably or jerk from side to side, and the eyelids may tremble. Severe headaches often occur during or after an attack.
- Absence epilepsy. Symptoms of this disease are characterized by short-term fainting or loss of consciousness. With rare exceptions, absence epilepsy is manifested by a loss of concentration; a person cannot focus, breaks off a sentence mid-sentence and cannot build a logical chain to convey his idea. His movements are unclear, his hands can move uncontrollably, inexplicable sensations arise in his fingers, so the patient wants to stretch his hands.
- Myoclonic epilepsy. Manifests itself with sudden spontaneous movements of the arms and legs. The symptoms of this disease are often ignored and confused with the completely normal hypnogogic myoclonus that everyone experiences when falling asleep.
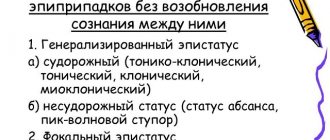
In addition to the classification of epilepsy, individual forms of epileptic seizures are also distinguished.
Treatment of epilepsy in children
The first step to overcoming the disease is diagnosis in the office of a neurologist. If one of the presented signs begins to appear, you should immediately go to a good clinic. An experienced doctor will identify the problem (probably requiring tests to make an accurate diagnosis), and select a strategy to solve it.
Effective medications are used to treat epilepsy. Every third child recovers as a result of drug treatment alone. The use of hardware technologies makes it possible to permanently cure more than 75% of babies.
Treatment at the Yusupov Hospital
To alleviate the condition of patients suffering from epilepsy, the specialists at the neurology clinic at the Yusupov Hospital have several methods at their disposal. Properly selected treatment and strict adherence by the epileptic to medical recommendations can achieve stable remission for a long time.
Drug treatment helps to reduce electrical activity in the lobe of the brain where the disease, previously identified through EEG (electroencephalography), is localized. Treatment of patients at the Yusupov Hospital is carried out using the most modern medications that have a pronounced therapeutic effect and have minimal side effects. During drug treatment at the Yusupov Hospital, patients are constantly monitored by doctors who monitor the course of the disease.
Prevention of epileptic seizures
There are preventive recommendations that, if followed, can prevent epileptic seizures, especially if you already have a history of them:
- you should protect yourself from getting traumatic brain injuries;
- stop smoking, drinking alcohol and drugs;
- try not to stay in stuffy, unventilated rooms for a long time;
- avoid hypothermia;
- give preference to a healthy lifestyle and sports;
- avoid stressful situations;
- do not overwork;
- observe the work and rest schedule.
Epilepsy is a rather severe and difficult-to-treat pathology. Thanks to the prescription of modern anticonvulsants, doctors at the neurology clinic of the Yusupov Hospital are able to significantly improve the quality of life of their patients and prevent the development of new epileptic seizures in them.
An appointment with a neurologist at the Yusupov Hospital can be made by phone or on the clinic’s website. You can also ask questions regarding the conditions of hospitalization in a hospital and the estimated cost of the services provided.