Babies, as a rule, often fall in the first year of life, when they are learning to walk or due to the neglect of adults, falling out of bed is very common. If this occurs, it is important to calmly assess the situation and pay close attention to signs of injury.
Although it may look scary, falling out of bed usually does not cause serious harm. However, injuries can occur, so parents should know the signs that indicate their child needs medical evaluation after a fall.
What is meant by the term “concussion” and what are its causes in children?
A concussion is a mild traumatic brain injury and is characterized by the absence of focal damage to the brain.
This pathology is diffuse, all changes occur at the cellular and subcellular level. Thus, identifying a concussion in an adult, and even more so in a child, is a very difficult task even with the use of modern diagnostic methods. Most often, boys suffer from this type of injury, and there is a seasonal fluctuation - the spring-summer period is especially rich in various craniocerebral “incidents”. There is also a tendency towards an increase in the number of concussions in children of preschool and primary school age. The peak incidence occurs between 8 and 12 years of age.
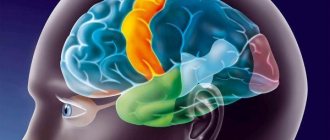
It is not only the direct traumatic agent that has a negative effect on the brain; in other words, neurons will be damaged both at the site of the impact and at a distance from it. At this moment, redistribution of cerebrospinal fluid occurs in the ventricular and subarachnoid spaces. As a result, a hydrodynamic shock occurs, diffusely damaging the cells. Another link in the pathogenesis of concussion is the displacement and rotation of the cerebral hemispheres relative to the rigidly fixed brain stem.
All this leads to disruption of the vascular tone of the cerebral arteries and veins, increased metabolism in cells (the so-called “metabolic fire”), changes in the permeability of the blood-brain barrier, liquorodynamic disorders, as well as dysfunction of the transmission of impulses from neuron to neuron.
Despite the fact that a concussion is a mild form of injury, pathological changes occurring in the brain, if not properly treated, can lead to disability.
The most common causes of concussion in children under one year of age
Most often, children between birth and one year old receive any injuries due to the fault of their parents. This may be a simple oversight and carelessness of young mothers and fathers who, without thinking about the consequences, leave their babies alone on the bed or changing table, in a stroller, in a high chair and walk away, even if only for a minute.
A child can also get a concussion due to excessively active motion sickness, aggressive behavior on the part of adults, or even simply being thrown up. This type of injury, in which there is no effect of the traumatic agent on the skull, is called “shaken baby” syndrome.
Causes of injury in a child aged one to three years
At this age, the child begins to explore the world around him, learns to walk and run. Therefore, among the causes of concussion, falling from height, hitting the head on various furniture, etc. come to the fore. At the same time, children do not have a sense of danger; they do not know how to land correctly with their arms forward.
Also, do not forget about the facts of violence from adults: a small (according to parents) slap in the face can lead to injury.
Concussion in preschool children
Concussions in preschool children also most often occur as a result of unsuccessful landings after a jump, road traffic accidents, hits to the head from sports equipment and merry-go-rounds on playgrounds. Often the cause of injury during this period is a fall from an open window.
Why are schoolchildren so vulnerable to injury?
Schoolchildren receive various types of injuries, including concussions, as a result of their carelessness. This happens due to falls from trees, garage roofs, and extreme sports. Fights contribute a lot to this.
Typical cases of traumatic brain injury in infants
- The baby lies on the changing table or on the sofa, the mother turns away for a few moments, and the baby falls on his butt.
- The baby is left unattended in a high chair. He pushes off the table with his feet and falls on his back along with the chair.
- The baby is trying to get up in the crib. Something on the floor interested him, and he hangs over the side and falls.
- The little one was left sitting in the stroller, not expecting that he would try to stand up in it and, not finding support, would fall down.
Is concussion in children classified according to severity?
Current standards of care do not classify concussions in children based on severity.
But in order to more accurately describe the patient’s condition to a colleague or relatives of the victim, among doctors there is the following gradation of injury:
- a mild degree of concussion is characterized by the absence of any type of amnesia, the child does not experience a disturbance of consciousness either at the time of injury or after it, and headache, nausea and other symptoms last no more than an hour;
- a moderate concussion occurs when children have anterograde amnesia and severe cerebral symptoms with preserved consciousness;
- A severe concussion in children is manifested by all the key symptoms inherent in this type of injury.
Treatment in hospital and at home
Usually, when a concussion is confirmed in a child, he is recommended to be hospitalized, regardless of the severity of the condition. In simple cases, hospital stay is limited to 3-4 days. In more difficult situations, the baby remains in the hospital for up to 1-2 weeks. Therapy involves monitoring the victim’s vital signs and well-being, preventing cerebral edema and the development of serious structural damage to the organ.
Treatment of concussion is based on taking the following groups of drugs:
- diuretics;
- medicines with potassium;
- sedatives;
- antihistamines;
- analgesics;
- antiemetics - according to indications.
At home, treatment of TBI continues according to the regimen drawn up by the doctor. It includes taking vitamins and nootropics. For 2 weeks after discharge from the hospital, the child is prescribed bed rest or maximum rest. The patient’s usual lifestyle changes in order to prevent physical and emotional overload. Active games, prolonged watching of TV, and uncontrolled use of gadgets are contraindicated for the victim. After a course of therapy, all symptoms of a concussion should completely disappear. If any alarming manifestations remind you of themselves, you must inform your doctor about this.
The most common symptoms of concussion in children
Symptoms of a concussion in school-aged children are virtually the same as those observed during an injury in adults. The child can clearly tell what happened to him and how he is feeling at the moment. It is much more difficult to notice and identify the first signs of a concussion in a child under three or four years of age, when the child cannot yet describe his sensations.
General cerebral symptoms as the first signs of concussion in children
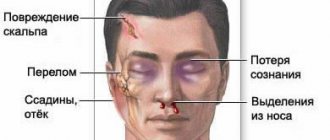
The most common symptoms of a concussion in a child are headache, vomiting, loss of consciousness and memory impairment. But it is not only mild traumatic brain injury that has such signs. Therefore, it is important to know the characteristics and features of each of them.
Headache
Headache caused by a concussion has a spreading, diffuse nature due to increased intracranial pressure. Sometimes there are complaints of dizziness, which does not depend on body position. Young children will experience irritability, rapid mood swings, tearfulness, sleep disturbance in the form of drowsiness during the day and insomnia at night. During this period, the child tries to avoid noise and bright light, which usually worsen the headache.
Nausea and vomiting
Another manifestation of liquor hypertension is nausea and vomiting, which do not depend on the fact of eating. Babies in the first months of life may experience sudden, repeated regurgitation. Such vomiting does not bring relief, and nausea can persist for up to several days.
Impaired consciousness
Almost always, a concussion is accompanied by a short-term loss of consciousness, which usually does not exceed ten minutes. In young children, this fact may go unnoticed; adults may think that the child simply became quiet for a couple of seconds. Restoration of consciousness may be marked by screaming or crying.
In school-age children, one of the criteria for a concussion is a memory disorder in the form of anterograde, retrograde or congrade amnesia. That is, events that occur after the injury, before it, or the incident itself that led to the concussion are forgotten, respectively.
Symptoms of a concussion that are detected during a detailed neurological examination
Parents can also identify the symptoms described above; the remaining specific signs of a concussion in children can only be determined by a qualified specialist when examining the neurological status of a small patient.
Autonomic dysfunction
A concussion also entails disruption of the autonomic nervous system. The following symptoms are observed:
- increased sweating, especially in the palms and soles;
- pallor, or even cyanosis, of the distal limbs;
- low-grade fever (increased body temperature ranging from 37.1 to 38C). Often this sign is asymmetrical: body temperature will differ in the left and right armpits;
- fluctuations in blood pressure and pulse, which are usually higher than normal for the child’s age;
- “play of capillaries” is a symptom indicating a violation of vascular tone. It manifests itself as a sharp change from pallor on the face to a bright blush.
Transient small focal symptoms
A concussion is also characterized by the presence of microfocal neurological symptoms, which are the result of minor hemorrhages and swelling of the brain substance. Damage to neurons in mild traumatic brain injury is minimal, so it is possible to observe these signs only within 3-4 hours from the moment of injury.
These include:
- anisoreflexia, that is, asymmetry of tendon and periosteal reflexes;
- horizontal small-amplitude nystagmus;
- oculomotor disorders in the form of limited lateral movement of the eyeballs, which is accompanied by pain and double vision;
- vestibular dysfunction, manifested by unsteadiness while walking and in the Romberg position;
- decreased muscle tone in one half of the body;
- violation of the corneal (corneal) reflex.
Such symptoms may hide a more severe traumatic brain injury, which is a threat to the child’s life. Therefore, at the slightest suspicion of a disease, immediately seek medical help.
Why can't you shake a baby?
Due to the large size of the skull (up to 15% of the total body weight) and undeveloped muscles of the baby, high head mobility occurs. When shaking, the child's head swings from side to side and the brain hits the skull. With strong shaking, the spinal cord can separate from the brain at the level of the brain stem, and the vessels begin to burst. The damage from such shaking of a baby is much greater than from a blow from a fall from a small height.
Consequences of shaking a baby:
- Brain hemorrhages;
- Brain swelling;
- Retinal hemorrhages
Symptoms caused by shaking:
- breathing disorder,
- disturbance of consciousness,
- vomiting and lack of appetite,
- convulsions,
- increased drowsiness or irritability;
- pale skin,
- change in the child's behavior;
- bulging and pulsation of the large fontanel;
- stopping breathing during sleep (apnea).
Remember: any shaking of the baby is a manifestation of violence against the child!
CDS is a medical emergency because injuries sustained by a child during abuse can result in severe brain damage or death. The problem is that not all parents report that their child was treated this way. As a rule, if a child with severe consequences after shaking survives, then he will have persistent neurological disorders for the rest of his life.
SDS is not always a consequence of abuse of a child; this also happens in the case of excessively strong swinging of the child, throwing the baby and in other everyday situations, but such situations are extremely rare, so SDS is considered primarily from the point of view of violence against the child.
Are there complications after a concussion in children?
Although a concussion is not accompanied by focal brain damage, the microstructural damage that occurs often does not go away without leaving a trace. After a mild traumatic brain injury, post-concussion syndrome may be observed for 3-3.5 months, accompanied by headache, intellectual-mnestic disorders, dizziness, emotional lability and dyssomnia. After this time, complaints usually disappear.
Repeated concussions lead to the development of post-traumatic encephalopathy, which is already a persistent consequence of injury.
Its main symptoms are:
- headache , the intensity of which is greatest after sleep. Often such children have meteodependence;
- increased intracranial pressure, accompanied by liquor-hypertensive paroxysms;
- post-traumatic epilepsy , which usually manifests itself in partial seizures with secondary generalization;
- post-traumatic parkinsonism , which occurs against the background of prolonged hypoxia of the subcortical structures of the brain;
- vestibular disorders (unsteadiness when walking, dizziness);
- autonomic disorders;
- intellectual-mnestic dysfunction (decreased memory, deterioration of concentration, viscosity of thinking). In young children it manifests itself as a delay in neuropsychic development, in schoolchildren - poor assimilation of educational material, etc.;
- psychoemotional disorders , which include some personality change. A child who was previously calm and assiduous becomes irritable, whiny, and may experience depression;
- scattered cerebral microsymptoms (anisoreflexia, asymmetry of muscle tone, etc.).
In order to minimize the likelihood of developing the consequences of a concussion, it is necessary to contact a neurologist at the first signs of pathology to receive adequate treatment.
Consequences of TBI
Research on traumatic brain injury shows that even mild trauma can cause undesirable consequences.
Under the influence of trauma (the moment of mechanical damage to the brain substance) and its consequences, the functions of various parts of the brain are disrupted, and, consequently, the work of the organs and systems subordinate to them (endocrine, digestive systems, etc.). Blood flow may be impaired, including the outflow of venous blood from the cranial cavity. The regulation of vascular tone suffers - they can narrow inadequately, leading to increased blood pressure. All this worsens the course of metabolic processes in the brain, as a result of which brain cells can be replaced by cystic cavities, that is, holes filled with fluid form in their place, and in the place where these cysts are, certain brain functions are lost. For example, the frontal lobes are responsible for intelligence, which means that the presence of cysts in this place reduces it. In addition, it is known that the brain normally has spaces inside and outside filled with cerebral (cerebrospinal) fluid. After injury, it can accumulate excessively in them - and consequently, intracranial pressure increases. The fluid under pressure compresses the substance of the brain, causing its slow atrophy5 (this phenomenon can also occur during the formation of cysts).
The triggering of pathological mechanisms of injury depends on its severity: the more severe it is, the more pronounced the disorders, the worse the outcomes, and the longer the recovery period.
5Atrophy (from the Greek atrophia; a - absence of a sign or quality, trophe - nutrition) - a decrease in the mass and volume of an organ or tissue as a result of a nutritional disorder, accompanied by a weakening or cessation of their functions.
For mild traumatic brain injury, the prognosis is usually favorable, provided that the recommended regimen and treatment are followed. After recovery, phenomena of asthenia are possible - the child quickly gets tired, becomes inattentive, and irritable. At the same time, the baby is more inhibited, which can lead to repeated injuries. These phenomena can affect the child’s intellectual development in the future.
In case of moderate TBI, the phenomena of asthenia may be accompanied by increased intracranial pressure, frequent headaches, and loss of coordination.
With severe TBI, the prognosis can be unfavorable - mortality in these cases reaches 15-30%. After recovery, a wide variety of consequences are possible: from varying degrees of motor impairment, severe convulsive attacks to severe mental disorders and consciousness, which leads to disability.
With open TBI, purulent-inflammatory complications often occur (for example, meningitis - inflammation of the membranes of the brain, etc.), which can also lead to death.
There is still no clear answer to the question of how long it takes for the body to fully recover, even after a mild TBI. It was believed that after such an injury, recovery occurs within a few days, a maximum of 2-3 weeks. But studies have shown that 1-3 months after a concussion, at least half of the children show certain deviations from the norm, which sometimes persist for a longer time. The speed of recovery depends primarily on the severity of the injury, the age and previous health of the child.
Among various injuries to the body, head injuries account for 30-50% of all injuries in children. And every year this figure increases by 2%.
Advertising
First aid tactics for suspected concussion in a child
If you notice symptoms of a concussion in a child, it is very important to provide first aid correctly so as not to harm him with your actions. After all, the wrong tactics of adult behavior in this situation can lead to a worsening of the victim’s condition.
So, to reduce the risk of further damage to brain cells, you need to:
- Place the child on a horizontal surface. If there is a suspicion of spinal damage, then the patient should not be moved under any circumstances;
- Do not give children medications on your own, as some of them change the clinical picture of the disease and make diagnosis difficult. The most you can do is apply a bandage if the soft tissue of the head is damaged and apply ice for a short time;
- monitor the child’s condition : you need to remember whether there was a loss of consciousness, how long it lasted, whether there were convulsions or vomiting. By sharing this information with your doctor, you will make it easier to make the correct diagnosis.
If you suspect a concussion in a child, immediately call an ambulance; do not wait for the victim’s condition to worsen.
Who is to blame and what to do?
Such situations most often arise when the mother or other people caring for the child do not rest and burnout occurs. For one reason or another, a child may cry for a long time, and the mother, in response to this crying, begins to do things that she could not even think about: shake the baby or even throw her.
The child may be lucky, and he will only receive bruises, abrasions and slight fear, or he may not be lucky at all, and then the baby will develop SDS.
When a child exhibits symptoms that are atypical for his usual condition, which we wrote about above, the parents go to the hospital. In the best case, within a day the child will be given a correct diagnosis and prescribed treatment. In 91% of cases, symptoms characteristic of SDS develop immediately after shaking, and in 70% of cases it turns out that the child has been shaken many times.
It often happens that parents do not go to the hospital immediately for a number of reasons:
- the parents did not understand what the child’s condition was due to shaking and did not say anything about it
- the parents realized that it was due to shaking and did not say anything about it to avoid liability
- there was little or no external damage
And the loss of time during SDS is tantamount to death.
It is very important and difficult in this situation to understand and prove that the injuries are a consequence of abuse of the child, and not domestic injuries that the child received while learning to walk and constantly falling. At the same time, there is always a risk of blaming an innocent person and destroying the family or not understanding who is really harming the child.
Diagnostic measures
Diagnosing concussion in children is quite a difficult task even for an experienced neurologist. Since, unlike more severe traumatic brain injury, this pathology is not characterized by structural changes in brain tissue that are detected using available research methods. It is also very difficult to collect complaints and a reliable history of the disease in a child.
Neurological status examination
During the initial examination, a pediatric neurologist collects complaints, life history and illnesses. Young children are not able to provide this information, so everything that happened to the baby should be remembered well and then reported to the doctor by those who were near the child at the time of the injury.
The specialist will be interested in the following questions:
- Under what circumstances did the injury occur?
- Was there a loss of consciousness, limpness, or a sharp cry in the child?
- Did you vomit or convulse after hitting your head?
- Have there been any traumatic brain injuries, etc., before this incident?
If the doctor manages to collect a reliable history, this will greatly facilitate the diagnosis and allow the correct treatment to be prescribed.
X-ray of the skull
X-ray of the skull, or craniography, is a mandatory examination method for head trauma in children. The presence of cracks or fractures in the bones of the skull excludes a concussion.
Ultrasound
Infants, thanks to an open fontanel, can undergo a neurosonographic study, which will exclude contusion lesions in the brain tissue, the presence of hematomas in the cranial cavity, as well as increased intracranial pressure. Older children undergo echoencephaloscopy, which indirectly assesses the state of the brain using the M-echo response. With a concussion, the brain does not become displaced, which indicates the absence of a more severe traumatic brain injury.
EEG
An electroencephalogram is a method of recording the electrical potentials of the brain. During a concussion, a change in the α-rhythm is revealed, namely its unevenness, and zonal differences disappear. Complexes of sharp waves can also be detected. The use of provoking tests (hyperventilation, etc.) can cause paroxysmal slow-wave activity.
CT or MRI
When carrying out neuroimaging diagnostic methods (CT or MRI), focal changes in brain tissue or expansion of the ventricular system and subarachnoid space are not detected. An indirect criterion for a concussion can be signs of swelling of the brain or its membranes detected on MRI.
Consultation with an ophthalmologist
The complex of mandatory diagnostic measures for concussion in children includes consultation with an ophthalmologist.
When examining the condition of the fundus, a pink optic disc with fairly clear boundaries is observed; vascular tone most often remains unchanged. Occasionally, slight venous congestion is detected. It must be remembered that the diagnosis of any traumatic brain injury should be carried out by a qualified specialist, since the health of your child depends on it.
Treatment tactics for TBI
After the examination and clarification of the diagnosis, treatment tactics are determined. Drug treatment is prescribed (therapy aimed at eliminating cerebral edema, lowering intracranial pressure, correcting metabolism and blood flow in the brain, etc.). Surgical treatment is used (and necessary) primarily to eliminate compression of the brain. It is prescribed to children with depressed fractures of the skull bones and intracranial hemorrhages.
Parents need to realize that only a comprehensive, adequate examination of the child allows for correct and timely treatment of brain injury, achieving recovery and avoiding disability.
Treatment of concussion in children. Main groups of drugs
Concussions in children require treatment only in a hospital setting, since imaginary well-being may turn out to be a “bright spot” during which the formation of an intracranial hematoma occurs.
One of the key points in the treatment of a concussion in a child is to ensure a therapeutic and protective daily routine. It consists of bed rest, the absence of psycho-emotional stress, it is necessary to exclude watching TV and using phones, tablets, etc. The course of treatment is usually 5-14 days.
For mild traumatic brain injury, the use of the following groups of drugs is indicated:
- dehydration agents (10% sodium chloride solution, Lasix, furosemide, hypothiazide);
- vascular agents (cavinton, trental, pentoxifylline, nicotinic acid, aminophylline);
- B vitamins (combilipen, compligamma B, milgamma);
- desensitizing agents (suprastin, tavegil, diprazine, diphenhydramine);
- neurometabolites (cortexin, actovegin, cerebrolysin);
- neuroprotectors (Ceraxon, Pharmaxon, Gliatilin, Gleacer, Cerepro);
- nootropics (picamilon, piracetam, lucetam, thiocetam);
- sedatives (glycine, tincture of valerian, motherwort, peony).
In the recovery period after a concussion, it is advisable to use physiotherapeutic procedures (electric sleep, magnetic therapy), as well as reflexology (acupuncture), which will reduce the risk of developing complications of injury.
What to do first if a child falls
We strongly advise parents whose children have suffered a head injury: even if, in your opinion, nothing bothers the baby, he fell from a small height, stopped crying, etc., immediately seek help from the following doctors: a pediatric neurologist, a traumatologist, a neurosurgeon. To do this, you need to call an ambulance at home and you and your child will be taken to a specialized hospital. Or, go to the emergency surgery department of any large children's hospital yourself, where the child will be consulted by the specified specialists. If they do not confirm the pathology, you can safely return home.
Failure to consult a doctor is dangerous due to late diagnosis of the injury, worsening of the child’s condition, and the possibility of coma. All this requires treatment in intensive care, and in some cases, surgical intervention. Delayed consultation with a doctor increases the risk of death and complications, lengthens the recovery period and worsens its outcome, to the point that the child may become disabled.