Meningococcus is not only in Africa
This infection is widespread throughout the world. And in Africa there is even a so-called “meningitis” or “meningococcal belt”:
However, this disease does not only exist somewhere far away, on other continents; unfortunately, it is also close to us. Outbreaks of meningococcal infection are recorded every now and then in different regions of Russia.
For example, in Novosibirsk in 2021, 25 cases of the disease were registered in less than two weeks. And this is very characteristic of this infection: usually long periods of well-being (10-15 years) are interrupted by sharp increases in incidence, which have a focal outbreak nature.
The increase in incidence can be explained by the widespread carriage of meningococcal bacteria. As the number of susceptible individuals increases, the number of cases increases. And declines are ensured by an increase in the immune layer as a result of latent immunization as bacterial carriage spreads among the population of a given territory.
You need to understand that during recession years the infection does not disappear: 50% of diseases occur in children under 5 years of age; 20% - for children aged 6-14 years. As age increases, incidence rates decrease, but carriage rates increase. The age group of 15-20 years is also subject to a high degree of susceptibility, because its representatives - students, military personnel - communicate intensively in schools, dormitories, barracks, etc. First of all, those who come from remote areas get sick, i.e. not previously in contact with the pathogen.
Why are doctors sometimes unable to identify meningococcal infection in the early stages of the disease and provide timely assistance? The fact is that the first symptoms of the disease are similar to the onset of a regular acute respiratory viral infection, and later medicine turns out to be powerless against the lightning-fast course of the disease. Moreover, during periods of prosperity, cases of the disease are so rare that the alertness of even experienced doctors, not to mention young novice doctors, gradually decreases.
One of the features that can also be canceled is that meningococcal infection is characterized by a winter-spring seasonality with the maximum number of diseases in February – April.
There are many real stories about how this can happen, here is one of them (a video from our partners - Sanofi Pasteur):
Latest epidemics
It is estimated that 80-85% of all cases in the meningitis belt are caused by group A meningococcus, and epidemics occur every 7-14 years. The highest rates of the disease are found in the meningitis belt of sub-Saharan Africa, stretching from Senegal in the west to Ethiopia in the east.
During the 2009 epidemic season, a total of 88,199 suspected cases, of which 5,352 were fatal, were reported in 14 African countries conducting enhanced surveillance. This is the largest number of victims since the 1996 epidemic.
How does infection occur?
The causative agent of meningococcal infection is the bacterium Neisseria meningitides. There are 12 varieties of it, six of which lead to severe forms of the disease. The bacterium is covered with a special capsule, which makes it especially resistant to immune cells.
In most cases, carriage of meningococcus on the mucous membrane does not cause noticeable health problems. And only 10-15% of cases this leads to the development of inflammation.
The route of transmission is airborne. The bacterium enters a healthy body through the mucous membrane of the mouth and nasopharynx during close contact with a sick person or carrier.
ON A NOTE! According to WHO statistics, asymptomatic carriers of Neisseria meningitides are from 10 to 20% of the population.
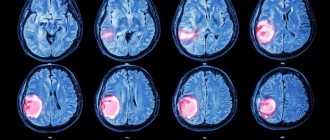
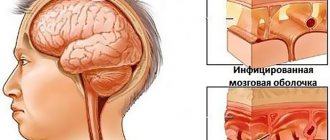
Through the mucous membrane, the pathogen enters the bloodstream and, quickly multiplying, spreads throughout the body, leading to sepsis (blood poisoning), inflammation of the internal organs, and the membranes of the brain. The first signs may appear after 24-48 hours. In general, the incubation (hidden) period can last from a day to 10 days.
ON A NOTE! The disease is classified as a “war” infection, since the increase in incidence is directly correlated with wars, as well as major disasters and accidents. Almost any situation that leads to stress, as well as significant crowding of people in poor living conditions, leads to the occurrence of meningococcal infection. It has been proven that if the number of meningococcal carriers in a team reaches 20% or more, then clinically pronounced forms of the disease appear.
General information
Meningococcal disease is potentially fatal and should always be treated as a medical emergency. Causes meningococcal meningitis - this is a bacterial form of meningitis - and is a serious purulent infection of the membranes surrounding the brain and spinal cord.
Meningitis is caused by a number of different bacteria. One such bacteria that can cause epidemics is Neisseria meningitidis. Twelve serogroups of N. meningitidis have been identified, six of which (A, D, C, W135 and X) can cause epidemics.
The bacterium is transmitted from person to person through droplets of secretions from the respiratory tract or throat of the carrier. Close and prolonged contact, such as kissing, sneezing, coughing toward another person, or living in close proximity to an infected person (for example, in a shared bedroom or sharing utensils), helps spread the disease. Bacteria can be carried in the throat, and sometimes, for reasons that are not entirely clear, by overwhelming the body's defenses, the infection spreads through the bloodstream to the brain.
Despite remaining gaps in our knowledge, it is estimated that 10–20% of the population are carriers of N. meningitidis at any given time. However, in epidemic situations the number of carriers may be higher. In an epidemiological sense, carriers are the most dangerous, since there are 1200-1800 carriers per one sick person.
How does meningococcal infection manifest?
Symptoms depend on the form of infection; When carried, the bacterium can only be detected using laboratory analysis, since there are no external signs. In other cases, symptoms may be as follows:
- acute nasopharyngitis – headache, runny nose or nasal congestion, weakness, increased body temperature;
- meningitis - a sharp increase in temperature, severe pain in the head, vomiting, pulling the legs towards the stomach, the inability to lower the neck and others characteristic of this disease;
- blood poisoning - a sharp increase in temperature, headache, confusion, muscle aches, rashes of varying sizes (most often on the lower part of the body);
- meningoenephalitis - symptoms similar to meningitis, various rashes on the skin and/or mucous membranes
A story from life! Muscovite Yana Savchenko’s 5-year-old daughter died of meningitis in January 2021. Mom and daughter were returning home by train. The girl’s temperature quickly rose to 41˚, her throat turned red, and her body took on the “coping dog” pose (with her legs pressed to her stomach). Upon arrival in Moscow, the child was immediately taken to the infectious diseases hospital, but after some time she died. Everything happened within 24 hours.
There is a test for mengococcal rash. You need to press the side of the glass against the rash-covered skin. It is important that you see the rash through the walls of the glass. If the rash is not visible when pressed, it is not meningococcal.
ATTENTION! Due to the high risk of serious complications and even death, at the slightest suspicion of meningococcal infection, you should immediately consult a doctor! Diagnosis is carried out by laboratory examination!
Features of treatment
The initial diagnosis of meningococcal meningitis can be made by clinical examination followed by a spinal puncture to isolate the pathogen from the puncture. Meningococcal disease is potentially fatal and should always be treated as a medical emergency. The patient must be admitted to the hospital, but is not required to be isolated.
Appropriate antibiotic treatment should be started as early as possible, ideally immediately after a lumbar puncture if such a puncture can be performed immediately. If treatment is started before a spinal tap is performed, growing bacteria from the cerebrospinal fluid and confirming the diagnosis may be difficult.
The infection can be treated with a range of antibiotics, including penicillin, ampicillin, chloramphenicol and ceftriaxone. In epidemic settings in areas of Africa with limited health infrastructure and resources, the preferred drugs are chloramphenicol oil solution or ceftriaxone, a single dose of which is effective in treating meningococcal meningitis.
What complications may there be?
As mentioned above, if meningococcal infection is detected late, there is a high probability of death. However, even if treatment was prescribed on time, often the disease does not go away harmlessly. The consequences can lead to a variety of complications, ranging from hearing loss, vision and speech disorders, to amputation of limbs, paralysis, epilepsy and hydrocephalus. And here is another video (video by our partners - Sanofi Pasteur) with a girl who, at the age of 5, suffered a meningococcal infection and was left deaf for the rest of her life:
Can a child survive?
With the development of infectious-toxic shock, mortality is high: up to 80%, even with timely initiation of therapy. The cause of death is microcirculation disorders, dysfunction of the cardiovascular, respiratory and urinary systems.
With prompt and competent treatment for meningococcemia, the prognosis for recovery is favorable; a child can survive even with fulminant meningococcemia, but this largely depends on the virulence of the infection, as well as immunity.
Possible consequences that may remain after meningococcemia:
- asthenic syndrome (weakness of the body, rapid fatigue, periodic headaches);
- paresis and paralysis;
- epilepsy (a zone is formed in the brain in which pathological excitation is observed in response to minor influences);
- hypertensive syndrome (increased intracranial pressure);
- decreased intelligence, memory, hearing acuity.
Who is at risk and how to prevent infection
Prevention of meningococcal infection can be nonspecific, it includes the following measures:
- isolation of identified carriers and sick people;
- preventing a recovered person from joining the team for 10 days after discharge;
- monitoring persons who have been in contact with sick people;
- teaching children basic hygiene rules;
- avoiding crowded places;
- increasing immunity by all available methods.
However, the most effective specific prevention is vaccination.
Meningococcal infection can affect anyone. The only exceptions are those who have been vaccinated.
However, doctors identify categories of people for whom the pathogen poses a particular danger. So, who should definitely get vaccinated against meningococcal infection:
- conscripts into the army (funds are allocated from the budgets of the regions sending guys to serve);
- travelers, especially to 26 meningitis belt countries: Benin, Burkina Faso, Burundi, Democratic Republic of the Congo, Gambia, Ghana, Guinea, Guinea-Bissau, Cameroon, Kenya, Ivory Coast, Mali, Mauritania, Niger, Nigeria , Rwanda, Senegal, Sudan, Tanzania, Togo, Uganda, Central African Republic, Chad, Eritrea, Ethiopia, South Sudan;
- pilgrims (since May 2001, vaccination with a quadrivalent (A+C+W135+Y) vaccine is mandatory for the Hajj to Saudi Arabia);
- persons with risk of contacts in outbreaks, i.e. according to epidemiological indications;
- children and teenagers before joining new groups (kindergarten, camp, school, boarding school, etc.) - paid for at the expense of CARING parents;
- medical workers.
Effectiveness of vaccination
Vaccination is carried out once, the effectiveness is about 90%, immunity is formed on average within 5 days and lasts 3-5 years.
In December 2010, a new meningococcal group A conjugate vaccine was introduced throughout Burkina Faso and parts of Mali and Niger, where a total of 20 million people aged 1–29 years were vaccinated. Subsequently, in 2011, these countries reported the lowest ever number of confirmed cases of meningitis A during the epidemic season.
By the end of 2013, two years after the introduction of the MenAfriVac vaccine developed by WHO and PNTZ, 150 million people in African countries affected by meningitis A had been vaccinated. It is hoped that all 25 countries in the African meningitis belt will introduce this vaccine by 2021. With broad coverage of the target group aged 1–29 years, meningococcal A epidemics are expected to be eliminated in this region of Africa.
Vaccines against meningococcal disease
The effectiveness of vaccination against meningococcal infection is almost 90%. The frequency, the need for re-vaccination, as well as age restrictions depend on the characteristics of the vaccine. Today, among the drugs you can find Mencevax ACWY, Menactra, Bexero, domestic ones - meningococcal A, A+C.
In a number of countries, vaccination against meningococcus is mandatory and is recommended by WHO. In Russia, vaccination against this infection is not yet included in the National Vaccination Calendar; budget funds are allocated only for conscripts and to eliminate outbreaks. Therefore, children, who are at the highest risk, today can be protected by vaccination only if their parents take care of it. Whether to build immunity from meningococcus in your child in advance or to believe that trouble will pass by is something that everyone decides individually. But, given the frequent cases of fulminant infection, the high risk of developing serious complications and even death, it is worth thinking about this issue in advance. Indeed, in most cases, parents who were faced with this terrible disaster either did not know about the existence of vaccination, or believed that their child was unlikely to encounter this infection, or postponed vaccination until better times...
"ASKO-MED" invites everyone to be vaccinated against meningococcal infection; the "MENAKTRA" vaccine is available. You can make an appointment for vaccination by phone: 8 800 555 84 09.
Rare forms of meningococcemia
Damage to the paranasal sinuses
Inflammation of the paranasal sinuses occurs with meningococcal nasopharyngitis and with a generalized form of infection.
Urethral lesion
Meningococcal nasopharyngitis can cause specific urethritis in homosexuals during orogenital contact.
Meningococcal iridocyclitis and uveitis
With meningococcal sepsis, the choroid of the eyes can be affected (uveitis). The lesion is often bilateral. Vitreous opacification is noted. It detaches from the retina. In places of peeling, rough adhesions form. Visual acuity decreases. Sometimes secondary glaucoma and cataracts develop.
With inflammation of the ciliary body and iris (iridocyclitis), severe pain appears already on the first day, visual acuity sharply decreases, even leading to blindness. The iris protrudes forward and takes on a rusty tint. Intraocular pressure decreases.
Involvement of all tissues of the eyeball in the inflammatory process (panophthalmitis) can result in complete blindness.
Rice. 15. Meningococcal uveitis (left) and iridocyclitis (right).
The nature of the inflammatory process in meningitis
Based on the analysis and appearance of the cerebrospinal fluid, as well as the patient’s condition, it is possible to determine the nature of the inflammatory process and quickly take therapeutic measures.
Purulent
A severe form of meningitis caused by bacteria is characterized by the accumulation of purulent exudate. As a result, the outflow of cerebrospinal fluid is disrupted, pronounced signs of intoxication are observed, and consciousness is often disturbed. It is necessary to prescribe a high dose of antibiotic, otherwise the mortality rate is very high - up to 95%.
Serous
It is a sign of viral meningitis. It proceeds favorably and often ends in complete recovery. It has a relatively short-term course: in the first 2-3 days from the onset of symptoms, an acute clinical picture is observed, and with timely treatment, improvement occurs already on days 5-6.
First aid
Since a hemorrhagic rash occurs when blood capillaries rupture, the first action upon detection should be to limit the child’s mobility and maintain bed rest until the doctor arrives.
Important! If a rash and symptoms similar to meningitis appear, you should immediately call an ambulance and take the patient to the hospital.
Only a doctor, after a general examination and examination of tests, can make a diagnosis and prescribe treatment. Meningitis is not only a severe illness for the patient himself, but also dangerous for others .
What kind of disease is this?
ATTENTION : Meningitis is a dangerous infectious disease that is transmitted by airborne droplets or through household items. Most often, the disease is diagnosed in preschool children.
Quite often, the pathological process begins with symptoms of nasopharyngitis, and only then vomiting, rash, and headache are added. The rash with meningitis on the first day of illness is very similar to the rash with measles.
Watch a video about the symptoms of meningitis:
Support and follow-up
The consequences of meningitis can have a huge negative impact on a person's life, their family and the local community, both financially and emotionally. Sometimes complications such as deafness, learning difficulties or behavioral disorders are not recognized by parents, carers or health professionals and therefore go untreated.
The consequences of meningitis often require long-term treatment. The permanent psychosocial impact of disability resulting from meningitis may create a need for medical care, educational assistance, and social and human rights support. Despite the high burden of meningitis on patients, their families and communities, access to services and support for these conditions is often insufficient, especially in low- and middle-income countries. Persons with disabilities due to meningitis and their families should be encouraged to seek services and advice from local and national disability societies and other disability-focused organizations where they can receive vital advice on their rights, economic opportunities and social life, so that people who have become disabled due to meningitis can live a full life.
Epidemiological surveillance
Epidemiological surveillance, from case detection to investigation and laboratory confirmation, is essential for successful control of meningococcal meningitis. Main objectives of surveillance:
- detection and confirmation of disease outbreaks;
- monitoring incidence trends, including the distribution and evolution of serogroups and serotypes;
- assessing the burden of disease;
- monitoring of pathogen resistance to antibiotics;
- monitoring the circulation, distribution and evolution of individual strains;
- assessing the effectiveness of strategies to control meningitis, in particular vaccine prevention programs.