December 21, 2020
Poliomyelitis is an acute infectious disease caused by a virus of the same name, characterized by damage to the central nervous system, primarily the cells of the anterior horns of the spinal cord, responsible for motor activity, the membranes of the brain and spinal cord
Poliomyelitis is an acute infectious disease caused by a virus of the same name, characterized by damage to the central nervous system, primarily the cells of the anterior horns of the spinal cord, which are responsible for motor activity, and the membranes of the brain and spinal cord. It is observed more often in children and leads to the development of paralysis.
Polio viruses have 3 serotypes. Type 1 most often causes paralysis and has been the most common cause of epidemics. Humans are the only natural host and the infection is extremely contagious through direct contact. Asymptomatic and minor infections (abortive poliomyelitis) are more common than nonparalytic or paralytic infections by a ratio of ≥ 60:1 and are the main source of spread.
Widespread vaccination has nearly eradicated the disease from the world. However, cases are still being reported in regions with incomplete immunization, such as sub-Saharan Africa and South Asia. At risk of contracting this infection: children under 7 years of age, pregnant women, people suffering from immunodeficiencies. The risk of infection is higher in the warm season: in summer or autumn, the virus is very tenacious, in a humid environment it can live up to 4 months.
How does infection occur and who is at risk?
The routes of infection with polio mainly come down to the penetration of the virus through the digestive tract - if water, food or hands have previously come into contact with contaminated substances. For example, feces of a sick person get into a pond, and then when swimming, the patient gets the virus along with the contaminated water. The causative agent of the disease is poliovirus.
You can become infected through water, food, dirty clothes, etc. At risk are:
- children under 7 years old. Poliomyelitis occurs much more often in children than in adults;
- Pregnant women;
- people with very weakened immune systems. This can be facilitated by various diseases, as well as disorders at the endocrine level, periods after operations, etc.;
- people suffering from immunodeficiencies.
The risk of infection is higher during the warm season: summer or autumn. The virus is very tenacious; in a humid environment it can live up to 4 months.
Victory of Soviet scientists
The fate of the live polio vaccine and its further role in global epidemiology was decided by Sabin’s meeting with the Soviet scientist Mikhail Chumakov. At that time, Mikhail Petrovich was in America - together with his wife and colleague, he was sent to the States to exchange experiences. Chumakov quickly seized on this theory, and after some time several thousand doses of polio vaccines were brought to the USSR.
The drug, which had not been fully tested, was tested on everyone - myself, relatives, colleagues. Understanding perfectly well the danger of such experiments, none of my relatives objected. Everyone knew that this was necessary to protect their children from a terrible disease.
Production of live Sabin vaccine has begun at the Polio Institute. However, the Ministry of Health did not approve of this idea - “if the drug was abandoned in America, why should we test and produce it”? Chumakov decided to take a risk and carried out a successful vaccination, after which the polio epidemic was ended in just a year and a half, and the vaccine was exported to more than 60 countries.
Symptoms of polio and course of the disease
The polio virus causes the following symptoms:
- signs of intoxication: nausea, vomiting, diarrhea, rash;
- cold-like disorders: cough, runny nose, sore throat, difficulty breathing and swallowing;
- fluctuations in blood pressure, fatigue, general poor health, headache;
- in rare cases - various types of paralysis that can lead to the death of the patient.
It is important to note that in 90% of cases, polio has no symptoms and does not affect the nervous system. And in 10% of cases there are very severe forms, involving inflammation of the membranes of the brain - with serious consequences, even fatal.
The incubation period of polio is quite short - it does not exceed 5 days. In this case, recovery in the case of a mild form occurs within 3 days. However, as we have already said, there are also complex forms - they are quite rare, but extremely dangerous. In this case, treatment may last for months, years, or may be completely useless.
Are you experiencing symptoms of polio?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Preparalytic stage
It is characterized by a rather acute onset, high body temperature, general malaise, headache, gastrointestinal disorders, rhinitis, pharyngitis. This clinical picture persists for 3 days, then the condition normalizes for 2-4 days. Afterwards there comes a sharp deterioration in the condition with the same symptoms, but more pronounced intensity. The following signs are included:
- pain in legs, arms, back;
- decreased reflexes;
- increased sensitivity;
- decreased muscle strength;
- convulsions;
- confusion;
- excessive sweating;
- spots on the skin;
- "goose pimples".
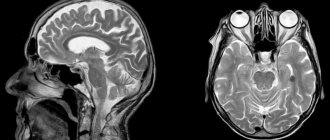
How is polio diagnosed?
If obvious symptoms of polio occur, the patient is admitted to an infectious diseases hospital, where an infectious disease specialist takes over the examination. To understand what the reason is, they carry out a number of manipulations, be sure to investigate:
- blood and urine tests;
- materials from the nasopharynx;
- feces;
- cerebrospinal fluid.
All this allows us to find out which pathogen caused the disease and make a correct diagnosis.
Classification
There are several forms of polio depending on the type of disease, its severity and course. By type, polio is typical (with damage to the central nervous system) and atypical (without damage to the central nervous system).
Typical forms of polio are non-paralytic and paralytic. The non-paralytic form is the meningeal form, which occurs as meningitis.
The paralytic form can come in several forms:
- spinal (damage to the spinal cord) - flaccid paralysis of the limbs, torso and neck;
- bulbar (damage to the cranial nerves) - disturbances in speech, breathing, swallowing and cardiac activity;
- pontine (damage to the brain stem) - complete or partial impairment of facial expressions;
- cerebral - proceeds as encephalitis;
- mixed - a combination of different variants of the paralytic form of polio.
Non-paralytic poliomyelitis can occur in two forms:
- inapparent form - carriage of the virus without any symptoms;
- abortive (or visceral) form - nonspecific general symptoms characteristic of most viral diseases (fever, intoxication, headache and others).
Poliomyelitis can be mild, moderate or severe in severity. The criteria for the degree of the disease are intoxication and the severity of motor disorders.
The course of the disease can be smooth (asymptomatic or symptoms characteristic only of polio) and non-smooth. In the latter case, these may be complications, exacerbations of chronic infections, or the emergence of new infections due to polio.
Paralysis of the right leg after suffering from polio. Photo: PHIL CDC
How the disease is treated in Moscow
Treatment of polio is carried out in an infectious diseases hospital and involves an integrated approach, including:
- strict bed rest. The patient should remain calm, in a favorable environment;
- protection of paralyzed muscles. For this purpose, special splints can be applied;
- physiotherapy. This includes physical therapy, swimming in the pool under the supervision of a trainer, and massage. This also includes electrical stimulation, paraffin applications, UHF therapy and much more. The procedures are aimed at stabilizing the nervous system, helping paralyzed muscles;
- Ventilation Clinical guidelines for polio also suggest major life-sustaining interventions. The use of a mechanical ventilation device is indicated for patients whose paralysis has affected the respiratory system, and therefore threatens respiratory arrest;
- use of special medications.
It is very important that a polio patient be closely monitored, especially when the disease is progressing or not showing significant improvement.
Paralytic stage
This is the stage when the patient suddenly suffers from paralysis (within a couple of hours). This stage lasts from 2-3 to 10-14 days. Patients during this period often die from severe respiratory and circulatory disorders. It has the following symptoms:
- flaccid paralysis;
- defecation disorders;
- decreased muscle tone;
- limitation or complete absence of active movements in the limbs and body;
- damage mainly to the muscles of the arms and legs, but the muscles of the neck and torso may also be affected;
- spontaneous muscle pain syndrome;
- damage to the medulla oblongata;
- urinary disorders;
- damage and paralysis of the diaphragm and respiratory muscles.
During the recovery period of polio, which lasts up to 1 year, tendon reflexes are gradually activated and movements in individual muscle groups are restored. The mosaic nature of the lesion and uneven recovery causes the development of atrophy and muscle contractures, growth retardation of the affected limb, the formation of osteoporosis and bone tissue atrophy.
The residual period, or the period of residual effects, is characterized by the presence of persistent paresis and paralysis, accompanied by muscle atrophy and trophic disorders, the development of contractures and deformation in the affected limbs and parts of the body.
Prevention of polio
The main preventive measure is vaccination of children, which is carried out at an early age and then again. There is a special vaccination calendar, on the basis of which pediatricians recommend undergoing this procedure. When vaccinated correctly, lifelong immunity and resistance to poliovirus are developed.
If we talk about the prevention of polio at the household level, it means:
- refusal to swim in dirty bodies of water that are not suitable for this;
- compliance with personal hygiene rules;
- refusal of potentially dangerous products. In this sense, raw milk is undesirable - a pathogen is often found in it;
- Quarantine measures if a child with a disease is detected in a children's group. At the same time, all objects and things are processed and disinfected.
Now polio is quite rare - this is due to centralized vaccination, thanks to which children from an early age develop immunity to the polio virus, and therefore calmly tolerate contact with it.
Forecast for life
Mild forms of poliomyelitis (occurring without damage to the central nervous system and meningeal) pass without a trace. Severe paralytic forms can lead to permanent disability and death.
Thanks to many years of targeted vaccine prevention of polio, the structure of the disease is dominated by mild inapparent and abortive forms of infection; paralytic forms occur only in unvaccinated individuals.
Questions and answers on the topic of polio
Is it necessary to get the OPV vaccine?
Parents have the opportunity to refuse such vaccination - they can write a written refusal and not undergo this procedure. However, doctors warn against such a decision: remember that if 10% of children get sick, the consequences will be irreversible, and for some children such a refusal will cost their lives. Currently, OPV vaccination is the only way to be 100% protected against the polio pathogen.
How is the polio vaccine given?
The vaccination is done twice, starting from the age of three months. The injection is given intramuscularly and contains the virus killed by formaldehyde.
How effective is vaccination against this disease?
Since the active fight against polio (1988), thanks to vaccination, it has been possible to reduce the number of cases from 350 thousand people per year to 359 cases (in 2014). These data speak for themselves: after receiving the vaccine, the disease becomes harmless and no longer threatens the person.
Vaccines
There are two types of vaccines to prevent polio—live oral polio vaccine (OPV) and inactivated polio vaccine (IPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life. All available evidence indicates that OPV is not teratogenic and is safe for pregnant women and HIV-infected individuals. However, rare serious adverse events associated with OPV may include vaccine-associated paralytic polio (VAPP) among vaccinated individuals and their contacts, and the emergence of vaccine-derived polioviruses (VDPV). The incidence of VAPP is estimated to be 2–4 cases per million births per year in countries using OPV. The introduction of at least one dose of IPV before OPV vaccination leads to the elimination of VAPP. Let us remind you that in the National Calendar of Preventive Vaccinations of the Russian Federation, the first two (!) vaccinations against polio are given with inactivated polio vaccine!
IPV is considered a highly safe vaccine whether given alone or in combination with other vaccines. There is no evidence of a cause-and-effect relationship with adverse events other than mild local erythema (0.5-1%), tissue induration (3-11%), and tenderness (14-29%).
More about vaccines