Hemianopia is a partial loss of vision due to congenital or acquired damage to the visual system. Hemianopsia is not an independent disease, but accompanies other diseases. Therefore, hemianopsia is treated by doctors of different specializations - oncologists, neurologists, therapists, endocrinologists, etc. Let's consider the causes of the pathology, methods of treatment and prevention.
General information
With hemianopsia, a person cannot see on one side of the eye—right or left. The visual picture partially falls out of sight, as if visibility was closed or blocked. Sometimes the disease is accompanied by hallucinations. This condition occurs when the visual structures of the brain, which controls all functions and systems of the body, are damaged. Therefore, pathology is classified as a neurological disease and does not belong to ophthalmology.
Hemianopsia occurs:
- congenital;
- acquired.
The acquired form most often develops in women after 30 years of age. Symptomatic treatment against the background of the underlying disease is indicated.
The congenital form develops against the background of lesions of the central nervous system:
- underdevelopment of the brain and cranium;
- exit of the meninges outside the cranium;
- increased intracranial pressure due to the influence of cerebrospinal fluid;
- dropsy of the brain.
In multiple sclerosis, the nerve membranes are affected, including the visual apparatus.
From a clinical point of view, two forms of pathology are distinguished:
- homonymous (symmetrical);
- heteronymous.
Homonymous hemianopsia is characterized by loss of the left/right part of the visual field in both eyes. Heteronymous pathology has 2 forms:
- bitemporal;
- binasal.
Bitemporal hemianopsia is characterized by loss of the temporal halves of the visual field in both eyes. The names of the pathology with the prefix “bi” indicate that blind areas of the visual field appear on both sides.
There is also a binasal form of hemianopsia, which appears due to the “empty sella” syndrome or chiasmatic arachnoiditis. Binasal pathology is loss of visual fields on the side of the nose. Such a clinical picture is rare; it accompanies oncology, hydrocephalus, inflammatory foci in the arachnoid membrane, and diseases of the central nervous system.
There are cases of partial damage to the visual system in one eye and complete blindness in the other.
Depending on the volume of the affected area, hemianopia occurs:
- full;
- partial;
- square;
- scotoma.
In case of complete hemianopsia, half of the visual field is affected, in case of partial hemianopsia, part of half of the visual field is affected. With a square one, only a quarter of the field; with a scotoma, a round-shaped spot appears in the visual field.
Visual neglect
Visual neglect (also called hemispatial neglect or unilateral spatial neglect) differs from hemianopsia in that it is an attentional deficit rather than a visual one. Unlike patients with hemianopsia, who cannot actually see, people with visual neglect do not have vision problems, but they do have an impaired ability to pay attention to and process the visual information they receive. While hemianopia can be alleviated by allowing patients to move their eyes around the visual scene (ensuring that the entire scene falls within their unimpaired visual field), neglect cannot be done. Neglect may also apply to auditory or tactile stimuli and may even result in the patient not noticing one side of their body.
Ellis and Young (1998) showed that neglect can also affect patients' mental maps, such that if they are asked to imagine themselves standing in a familiar place and name the buildings around them, they will not name the buildings on their affected side, but will be able to name them when asked to mentally turn in the opposite direction.
Some advanced treatment patients also have hemianopsia, but they often occur independently.
Causes
The acquired form of pathology develops when:
- occipital cortex;
- central parts of the visual pathways;
- visual tracts.
Damage to brain structures is caused by:
- acute cerebrovascular accidents;
- inflammatory processes of the meninges;
- volumetric intracranial formations - tumors;
- angiomatosis;
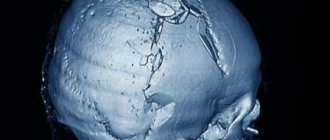
- traumatic brain injuries;
- iatrogenic factor;
- congenital pathology of the central nervous system.
- multiple sclerosis.
An acute disorder of cerebral blood supply is a stroke that can occur against the background of thrombosis of the vessels supplying the brain, arterial hypertension, atherosclerosis and other vascular pathologies. When blood circulation is impaired, the brain suffers from a lack of oxygen and glucose.
Inflammatory foci in the meninges are formed due to infection. This is possible with purulent otitis media, head trauma, as well as with inflammatory diseases of internal organs - the infection enters the brain through the bloodstream. For example, during an inflammatory process in the nasal sinuses, the chiasm located at the base of the brain may be affected. Inflammatory processes in the cerebral cortex can be influenced by purulent foci in the tissues of the lungs or bronchi.
Angiomatosis is a series of hereditary pathologies that affect the nervous system and skin. The disease is characterized by active proliferation of blood vessels and the formation of neoplasms - fibroids, plaques, etc.
An iatrogenic factor is unintentional damage to the visual apparatus during surgery on the central nervous system.
What is hemiplegia
Hemiplegia is a violation of the transmission of nerve impulses to the muscle fibers of any part of the body. In other words, the impulse coming from the cerebral cortex does not fully reach the motor neurons, which are located in the anterior horns of the spinal cord. It is for this reason that a person loses control over movements in the limbs or parts of the body. This condition is reversible. With proper treatment, recovery occurs very quickly.
If hemiplegia is temporary and undergoes treatment, then hemiparesis is a more serious condition. And it consists in severe damage to nerve fibers. Motor neurons are either completely destroyed under the influence of any irritants, or for some reason a physiological blockade occurs. In this case, treatment will no longer help. If the transmission of nerve impulses is disrupted, motor activity stops, and the muscles in this area atrophy. With hemiparesis, there is a right-sided or left-sided lesion.
In the case of hemiplegia, complete restoration of motor activity is possible, in contrast to hemiparesis. In the place where the medulla oblongata passes into the spinal cord, partial crossing of motor nerve fibers occurs, and various types of disorders occur here, but the symptoms of the lesion appear on the opposite side of the body. Such nuances are usually covered by a specialist.
Symptoms
Hemianopsia immediately begins with an acute form and accompanies a traumatic brain injury or stroke. Patients complain that entire areas of the visual image disappear from the field of vision or that large spots appear before the eyes - they prevent clear visualization.
Often the acute form of hemianopsia is accompanied by the following symptoms:
- dizziness;
- nausea, vomiting;
- violation of spatial orientation;
- increased blood pressure;
- violation of facial expressions;
- numbness of the limbs;
- speech disorder.
But sometimes the disease occurs without pronounced symptoms: the patient complains of constant headaches, which are accompanied by partial loss of visual fields; unmotivated weakness and general malaise appear. If such symptoms appear, you should immediately see an ophthalmologist or therapist.
Patients with hemianopsia find it difficult to cope with everyday responsibilities and perform normal work. Walking around the city is dangerous: they do not always see approaching vehicles, do not notice many objects on the road surface, and are poorly oriented in space.
When peripheral vision is lost, it is difficult for a person to navigate space, take care of himself, and perform daily work.
A healthy visual system provides a person with central and peripheral vision. With hemianopia, peripheral vision is absent, which leads to disorientation in space. The field of view is the totality of objects that a person sees simultaneously when fixing his gaze on one thing. When part of the visual field is lost, orientation in space is difficult or impossible.
What diseases does it develop in?
Homonymous hemianopsia can be either congenital or acquired. The following diseases can cause its occurrence:
- Ocular migraine. The development of hemianopsia is associated with impaired blood circulation in the area of the optic nerve. It is accompanied by such symptoms as extreme sensitivity of the eyes to light, nausea, increased hearing, and headaches. It occurs due to a significant expansion of the blood vessels in the brain. Blind areas due to this pathology appear in those places where blood flow is disrupted.
- Nephrotic syndrome.
- Hydrocephalus. As a result of this pathology, too much fluid accumulates in the brain. It also puts pressure on his tissues. For this reason, vision problems arise.
- Disorders of blood circulation in the brain, for example during a stroke.
- Epilepsy. Due to epileptic seizures, swelling of the brain occurs. It leads to visual impairment. Before an attack, the same symptoms may appear as before a migraine. The cause of the development of incomplete blindness can be either a hemorrhage that provokes epilepsy or the seizure itself.
- CNS disorders.
- Neoplasms in the brain. Due to their occurrence in the part of it that is responsible for vision, its tissues begin to be compressed. This process causes loss of vision.
- Intoxication of the body. Due to severe poisoning with ethyl alcohol, medications or any products, the quality of vision may also deteriorate.
- Traumatic brain injuries. They often cause tumors in the brain. It also puts pressure on those tissues in it that are responsible for the functioning of the organ of vision. As a result, partial blindness develops.
Prevent the development of glaucoma - eye pressure drops.
Find out why Taufon eye drops are prescribed from the article.
Sources
- https://moy-oftalmolog.com/symptoms/blurred-vision/gemianopsiya.html
- https://zrenue.com/nejrooftalmologija/54-zabolevanija-hiazmy/416-binazalnaja-gemianopsija.html
- https://www.minclinic.ru/pns/zritelniy_put_rasstroystva.html
- https://GlazaLik.ru/bolezni-glaz/drugie-bolezni/gemianopsiya/
- https://GlazaTochka.ru/bolezni/gomonimnaya-gemianopsiya
- https://okulist.online/zabolevaniya/glaz/zritelnyj-nerv/gomonimnaya-gemianopsiya.html
- https://GlazaLik.ru/bolezni-glaz/drugie-bolezni/gemianopsiya-gomonimnaya/
- https://glaz.guru/zabolevaniya/gomonimnaya-i-geteronimnaya-levostoronnyaya-gemianopsiya.html
- https://ozrenieglaz.ru/bolezni/drugie/gemianopsiya
- https://ProZrenie.online/zabolevaniya/redkie/gomonimnaya-gemianopsiya-vidy-metody-lecheniya-profilaktika.html
Clinical manifestations
The clinical course is complicated by agnosia or hallucinations. A patient with agnosia cannot distinguish between familiar objects: he simply does not recognize them. With prosopagnosia, the patient does not recognize familiar faces. With “mental gaze paralysis,” patients see only one object: surrounding objects completely fall out of sight.
Hallucinations occur in patients who have had a stroke. They can be either formalized (the patient sees familiar images) or unformed (various lines, geometric shapes). Hallucinations always appear unexpectedly.
The lesion can affect different parts of the visual apparatus:
- optic nerve;
- optical chiasmus;
- cortical visual analyzer;
- cerebral cortex.
Optic nerve
Complete damage to the optic nerve leads to absolute blindness. With partial damage, individual “pieces” fall out of the field of vision - the person sees a “cropped” picture or blind sectors appear in the field of vision.
If the optic chiasm is affected, the person may develop complete blindness. But in practice, partial damage most often occurs, which manifests itself in the absence of peripheral vision. Patients feel like a “horse in blinders,” that is, they cannot see anything on the sides. They have central vision, which can be sharp, but lateral vision is completely absent. This pathology is called bitemporal hemianopia.
Sometimes visibility disappears not on the sides, but in the central part. In this case, patients cannot see their own nose and complain that a black spot has appeared in front of their eyes on the side of the nose. This pathology is called binasal hemianopia.
Cortical visual analyzer
Homonymous (of the same name) hemianopsia is the most common clinical picture when the visual analyzer is damaged. Same name means on the same side. For example, right hemianopsia is loss of the left half of the visual field in both eyes. Less common is lower or upper hemianopsia.
If the cortical projection area is partially damaged, then a partial loss of the visual field is observed: either the squares appear in the upper left or lower right.
Cortex
If the cerebral cortex is damaged, hallucinations may occur. For example, the patient sees shiny lines or dots in front of him. The figures move with the movement of the eyeball. This phenomenon is called photopsia.
When the cerebral cortex is damaged, agnosia (inability to recognize familiar objects) or prosopagnosia (non-discrimination, failure to recognize familiar faces) develops.
Complications
Pathological damage to the optic tract leads to optic nerve atrophy. If the underlying disease that led to hemianopsia is incurable, then the patient’s quality of vision will gradually decrease until complete blindness.
Some patients develop persistent depression due to ophthalmological pathologies; they prefer to spend time alone and withdraw from society. Ridicule of ridiculous movements and sloppiness causes them psychological discomfort and a desire to avoid it by any means. If left untreated, depression can lead to more serious mental health problems. Therefore, patients should be consulted by a psychologist or psychotherapist.
↑ Changes in field of view
changes in the field of view kinetic and static perimetry isopters with low visual acuity The essence of the Kestenbaum test of reflex closure of the palpebral fissure For hemianopsia to relative hemianopsia good lighting To identify scotoma in the red color of topical diagnosis Fig. 82.
Diagram of the location of nerve fibers in the chiasm.
1 - retina; 2 - optic nerve; 3 - chiasma; 4 - optical path; 5 - diagram of the cross section of the chiasm; 6 - pituitary gland; 7 - zone of passage and intersection of the papillomacular bundle. on some features of the cross. Main types of changes in the visual field
Rice.
83. Scheme of typical changes in visual fields depending on the level of localization of the pathological focus (according to Duke-Elder S.). 1 - unilateral amaurosis with monolateral damage to the optic nerve;
2—unilateral amaurosis and contralateral temporal hemianopsia with damage to the intracranial portion of the optic nerve near the chiasm; 3 - bitemporal hemianopsia with damage to the medial part of the chiasm; 4 — incongruent homonymous hemianopsia with damage to the optic tract; 5 - homonymous hemianopsia without preservation of the macular zone with damage to the posterior part of the optical tract or the anterior part of the optical radiation; 6 - incongruent superior homonymous quadrantopsia with damage to the anterior part of the optical radiation (temporal lobe); 7 - weakly expressed incongruent homonymous inferior quadrantopsia with damage to the internal part of the optical radiation (parietal lobe); 8 - incongruent homonymous hemianopsia without preservation of the macular zone with damage to the middle part of the optical radiation; 9 - congruent homonymous hemianopsia with preservation of the macular zone with damage to the posterior part of the optical radiation; 10 - congruent homonymous hemianopsic central scotoma with damage to the occipital lobe. hemianopic visual field defects of the intracranial portion of the optic nerve
Rice.
84. Bitemporal hemianopsia with damage to the chiasm in the medial part.
Rice.
85. Right-sided homonymous hemianopsia with damage to the left optic tract.
Hemianopsias are divided
Rice.
86. Incomplete homonymous congruent hemianopsia (lesion at the level of the posterior parts of the left optical radiation).
Rice.
87. Incomplete homonymous incongruent left-sided hemianopsia (lesion at the level of the anterior parts of the right optical radiation).
secondary post-congestive atrophy of the optic nerve Unilateral concentric narrowing difficulty of differential diagnosis in combination with scotomas quadrant unilateral defects
Rice.
88. Unilateral inferotemporal quadrantopsia in a patient with a tumor of the right optic nerve.
absolute or relative scotomas Unilateral central or paracentral scotomas Homonymous hemianopicheal central scotomas chiasm defects cause damage to fibers Symmetrical bitemporal quadrantopsia
Rice.
89. Hemianopic bitemporal visual field defects due to compression of the chiasm from above.
asymmetric growth pattern Homonymous hemianopic in the form of quadrantopsia Tumors of the temporal lobe
Pathology of the organ of vision in general diseases | Komarov F.I., Nesterov A.P., Margolis M.G., Brovkina A.F.
Important Causes and differences of brain asymmetries, their impact on human life
Diagnostics
Diagnosis of any visual pathology begins with an ophthalmological examination - viziometry, autoreflectometry, examination of the pupil and measurement of intraocular pressure.
To establish hemianopia, you need to perform a topical diagnosis:
- perimetry;
- campimetry.
- Ultrasound Dopplerography;
- MRI;
- computed tomography;
- CT angiography.
Using perimetry, “blind” areas of the visual field are identified. This is the key diagnosis in this case. With homonymous pathology, symmetrical areas are formed: at the temporal part on one side and at the bridge of the nose on the other. That is, the right lobes or the left.
If perimetry cannot be performed due to the patient’s age or other reasons, other diagnostics are used. For example, the doctor holds a stick or towel in his hands and asks the patient to find the middle. With hemianopsia, the patient will divide only part of the stick in half, since he does not see the entire object. Also, the patient does not see the movement of the doctor’s fingers on the affected side of the eye.
With bitemporal pathology, there is a violation of the temporal halves of the visual field for both eyes. With binasal pathology, the central halves (near the nose) fall out.
Using computer campimetry, disturbances in color perception and color perception in a specific area of the visual field are determined.
MRI and CT can determine the etiology of the disease, which will help select the desired treatment algorithm. Using computer diagnostics, it is possible to determine the localization of tumors, areas of brain damage during a stroke, and the extent of traumatic injuries.
CT angiography visualizes the vascular network, using this diagnosis to determine the degree of damage to blood vessels.
Doppler ultrasound is a non-invasive examination method to determine the speed of blood flow.
Control studies
It is important to differentiate this disease from such pathologies as decreased perception of certain colors, that is, hemichromatopsia, and deterioration of vision in certain areas - hemihypoxia. These diseases may precede the onset of hemianopsia or develop independently.
To establish the exact number of visual fields that are lost, perimetry is performed.
Additionally, control tests are prescribed, which can only be carried out by doctors with normal vision. To do this, the patient and the doctor stand opposite each other at a distance of 10 centimeters. Their eyes must be at the same level. Both examination participants cover one eye with a bandage or hand. The patient must look carefully into the doctor's open eye.
The doctor begins to move the finger from the periphery to the central region alternately in all directions. When the doctor's finger appears in the patient's field of vision, he must report it. If the doctor himself does not suffer from pathology, and his indicators coincide with the parameters of the person being examined, then the patient has normal vision. Identifying this disease in this way will not be difficult.
Treatment
Without eliminating the underlying disease that caused the pathology of the visual analyzer, it is impossible to get rid of hemianopsia. Healing from a somatic disease will lead to full or partial restoration of visual fields. Treatment is carried out either by a neurosurgeon or a neurologist.
Treatment of encephalitis, stroke, and traumatic brain injury is carried out in a hospital. Some acute clinical conditions require emergency surgery. The development of a tumor process in the brain requires treatment at an oncology center: the patient is prescribed radiation therapy or chemotherapy.
If a genetic form of pathology is identified, consultation with a geneticist is required. It is impossible to cure a genetic pathology, so patients are prescribed symptomatic treatment. You will have to take medications and treatment for the rest of your life.
Congenital pathology can be eliminated with surgery or drug treatment. The result will depend on the degree of tissue damage, anatomical abnormalities, and concomitant diseases.
What does the ophthalmologist do in this case? He prescribes symptomatic treatment that relieves pain and partially restores visual function. For example, a doctor may prescribe medications that improve blood microcirculation in the tissues of the visual organ. To strengthen the immune system, immunomodulators and vitamin complexes are prescribed. Physiotherapy stimulates the functions of the optic nerve.
Patients are asked to wear special glasses that complement the missing visual picture.
If the underlying condition is not treated, the optic nerve may become damaged. Optic nerve atrophy leads to vision loss and complete blindness. It is important to consult a doctor in a timely manner and undergo medical examination if necessary.
Symptoms of hemiplegia
Hemiplegia is characterized by a violation of the conduction of nerve impulses from the brain to muscle fibers due to damage to the nerve fibers of the pyramidal tract. Based on this, the main and main clinical sign of this condition will be the absence of motor activity of any part of the body, depending on the location of the pathological focus: on the opposite side, cross or the same.
Forms of the disease:
- Tetraplegia. 4 limbs are involved in the pathological process.
- Monoplegia. Motor activity is impaired in 1 limb.
- Diplegia. Symmetrical parts of the body are affected.
- Hemiplegia. Impaired motor activity of any one part of the body, for example, the right arm, part of the torso, leg.
Associated symptoms of the disease are:
- Hypertonicity of the muscle tissue of the affected part of the body.
- Pathological reflexes of the limbs.
- Strengthening reflexes: tendon and periosteal.
- Decreased joint reflexes.
A person who suffers from a nerve patency disorder may experience: disturbances in speech and facial expressions on the affected side.
Prevention
It is impossible to prevent the development of pathology. However, the patient can improve the quality of vision if he follows the recommendations of doctors:
- when reading books, you should not turn your head to the sides;
- when reading books, keep your head straight, and try to cover as much of the text as possible with your eyes;
- you need to read the text not horizontally, but vertically;
- When reading, the book should be held at an angle of 90 degrees.
To expand the visual range, special ophthalmological programs developed by leading doctors are used.
In order not to provoke the development of pathology, you need to protect your head from blows and injuries. It is unacceptable to overstrain the visual organs so as not to injure the optic nerve and blood vessels. Avoid smoking tobacco and staying in environmentally unclean areas. Sometimes intoxication of the body leads to eye pathology, so follow safety precautions when working with chemicals.
Preventative examinations once a year are important for every person after 30 years of age. Left-sided or right-sided hemianopia most often develops in women aged 30-50 years. Pathology at the initial stage can only be noticed at a doctor’s appointment, so do not neglect regular professional examinations. This disease may not show itself in any way, but subsequently vision will begin to decline sharply. Along with decreased vision, the quality of life will deteriorate, even to the point of disability.
Consequences and complications
Restoring motor activity of a limb or part of the body depends on the degree of damage to the nerve structures, as well as on the root cause of the disease and treatment methods. With a timely diagnosis and treatment initiated, provided that the pathology is temporary, motor activity returns in full. But for a complete recovery, long-term rehabilitation will be required, visits to special centers and courses, where specialists will select methods of influencing the nervous system that are suitable for the patient.
In some cases, the disease is irreversible and the return of physical activity is impossible. In this case, hemiplegia turns into hemiparesis, and the patient becomes disabled.
Hemiplegia is a disease that needs to be fought. In addition, new methods of exposure and treatment methods for brain diseases are now being developed. New drugs are being developed that are more effective. With the correct diagnosis of the main diagnosis, as well as with competent therapy, the motor activity of the affected part of the body or limb can be returned to its previous state and one can continue to live at the usual pace of life.
Most birthmarks are harmless to a child, including single purplish red spots (called "angel's kiss"), but up to a quarter of children with this mark have Sturge-Weber syndrome. Many patients with Sturge-Weber syndrome are quite successful in life. At the same time, Sturge-Weber syndrome may be accompanied by neurological disorders in the form of hemiparesis, hemianopsia, mental retardation, ADHD, and symptomatic epilepsy.
What is Sturge-Weber syndrome?
Sturge-Weber syndrome (encephalotrigeminal angiomatosis) is a sporadic neurocutaneous disease (phakomatosis) with the occurrence of angiomas (benign vascular tumors) of the pia mater and facial skin, usually in the area of innervation of the ophthalmic and maxillary branches of the trigeminal nerve (although angiomas can also be on the human body, usually on the upper torso). Damage to the skin and pia mater can be unilateral (about 85% of cases) or bilateral (about 15% of cases).
Portrait of the Infanta Margherita Teresa [frontalcortex.com/?page=qod&topic=pediatric…]
Psychoneurological complications
- Movement disorders (hemiparesis)
- Visual impairment (hemianopsia, cataracts, glaucoma, retinal detachment)
- Mental retardation
- Attention deficit hyperactivity disorder (ADHD)
- Symptomatic epilepsy
Disease code
in the database of human hereditary diseases MIM ID 185300 (STURGE-WEBER SYNDROME; SWS, English).
How common is Sturge-Weber syndrome?
This is a fairly rare disease (1 in 50,000), which is equally common in both boys and girls.
The number of people with Sturge-Weber syndrome in general in the world and in our country in particular is unknown. The incidence of this disease varies over a fairly wide range - from 1 in 40,000 to 1 in 400,000 people in the population.
What is the cause of the development of Sturge-Weber syndrome?
The development of Sturge-Weber syndrome is caused by a disruption of normal embryonic development at 6-9 weeks of gestational development of the fetus, that is, during the first 2 months of gestation. Angiomas are formed from the remnants of the choroid plexus, which remains in the area of the head of the neural tube.
A number of experts associate the cause of the development of this disease with a gene mutation on chromosome 4q.
Sturge-Weber syndrome is characterized by so-called somatic genetic mosaicism, in which some human tissue cells have a causative genetic mutation, while others do not, that is, they are healthy. Depending on which cells are more numerous (with or without mutation), the severity of the disease and the rate of progression vary in different patients.
Thus, in 2002, it was shown that the mutation (paracentric inversion on chromosome 4q) occurs in approximately 40% of the cells in the meninges and in more than 50% of the cells in the area of the wine-colored “flaming nevus” on the skin of the face or scalp.
In other families, patients with Sturge-Weber syndrome had a different mutation, trisomy 10, which was found in cells in the area of the “flaming nevus” and was absent in normal skin cells.
In a number of clinical cases, Sturge-Weber syndrome is associated with another phakomatosis - Klippel-Trenaunay-Weber syndrome.
What is the risk of inheriting Sturge-Weber syndrome?
The risk of inheriting this disease is low. Sporadic gene mutations (so-called de novo mutations) predominate in certain groups of cells of the meninges, brain vessels, and skin.
What are the clinical manifestations of Sturge-Weber syndrome?
This disease can manifest itself in the form of isolated skin lesions, combined lesions of the skin and the central nervous system (brain), as well as the organ of vision (eyes).
What causes brain damage?
With this disease, a pathologically expanded network of vessels is noted, most often located in the zone of innervation of the trigeminal (trigeminal) nerve. It should be remembered that the trigeminal nerve innervates not only the face, but also the meninges. Therefore, a similar expansion of the vascular network is possible on the meninges on the same side where the spot on the face is located. When the pathologically expanded vascular network of the meninges is congested (for example, with an increase in body temperature, including those caused by vaccinations, overheating in the open sun or in a bath), irritation of the cerebral cortex (gray matter) is possible, which causes the development of epileptic seizures.
The neurological manifestations of Sturge-Weber syndrome vary depending on the location of pia mater angiomas, which are most often found in the parietal and occipital lobes.
Hydrocephalus (at birth and in infants) or intracranial hypertension (in children and adults) develops in Sturge-Weber syndrome due to impaired outflow due to intracerebral angiomas, both calcified and non-calcified.
Given the nature of brain damage, which varies widely among different patients with Sturge-Weber syndrome, the risk of developing symptomatic focal epilepsy is high (70-75%).
Mental retardation is not a mandatory symptom of Sturge-Weber syndrome, but is a consequence of repeated cerebrovascular accidents, if they do occur, and late diagnosed and drug-resistant symptomatic epilepsy, if one has developed. Therefore, patients should be registered with a neurogeneticist and a neurologist-epileptologist so that the child’s development continues in accordance with age in the future.
It is important to remember that the prescription of vascular drugs, which are often unjustifiably prescribed to children in the first years of life in local children's clinics, is not indicated for Sturge-Weber syndrome.
What eye pathology is possible with Sturge-Weber syndrome?
Sturge-Weber syndrome is often accompanied by the development of glaucoma at any age. Hemangiomas of the eyeball can over time lead to degeneration of the retinal epithelium, cystic degeneration, retinal detachment and loss of vision, so a child, teenager or adult suffering from this disease needs regular follow-up with an ophthalmologist.
Fundus of a patient with a port-wine stain on the face (Sturge-Weber syndrome)
, complicated by occlusion of the central retinal vein, diffuse choroidal retinal hemangioma, glaucoma [Hoyt, William Fletcher, 1926; Neuro-Ophthalmology Virtual Education Library: NOVEL]
What diagnostic methods are indicated for Sturge-Weber syndrome?
Examination methods for this disease include:
- angiography of cerebral arteries, veins and sinuses (MR angiography and SCT angiography are the most optimal because they are non-invasive techniques and can be used in both children and adults); characteristic signs of Sturge-Weber syndrome: incompetence of the superficial cortical veins, empty dural sinuses, pathological tortuosity of the veins;
- spinal puncture with subsequent collection of cerebrospinal fluid for examination (characteristic increase in protein),
- computed tomography (CT) of the brain (preferably multi-slice spiral computed tomography - MSCT); characteristic signs of Sturge-Weber syndrome: intracerebral calcifications, “tram rails” symptom, cortical atrophy, abnormal expansion of the venous network of the choroidal plexuses of the lateral ventricles;
- magnetic resonance imaging - MRI of the brain (preferably MRI with gadolinium contrast); characteristic signs: expansion of the choroidal plexuses, occlusion of the venous sinuses, cortical atrophy, demyelination of the brain of dystrophic origin;
- single photon emission computed tomography (SPECT); characteristic signs: areas of hyperperfusion of the brain substance (in the early stages of the development of the disease), areas of hypoperfusion of the brain (in the later stages of the development of the disease);
- positron emission tomography (PET); characteristic signs: areas of brain hypometabolism;
- video-EEG monitoring (VEM); characteristic signs: decreased power of bioelectrical activity of the brain, polyfocal epileptiform activity, represented mainly by paroxysms of high-amplitude theta and delta waves.
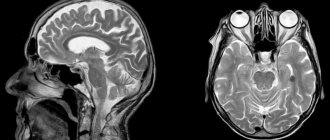
MRI of the brain with contrast in a patient with Sturge-Weber syndrome:
pial leptomeningeal venous angiomatosis, hemiatrophy of the cerebral hemisphere on the side of venous malformations. Clinically, the patient has a port-wine stain on the face in the area of innervation of the trigeminal nerve (on the side of the identified MRI changes) and epileptic seizures
Routine MRI (power less than 1.5 Tesla, slice thickness more than 1 mm) of the brain to diagnose Sturge-Weber syndrome may not be very informative (especially in small areas of the lesion), since the study must be performed by a neuroradiologist with special training in the characteristics of thin ( with a thickness of 1 mm) scanning the surface of the brain. At the same time, the magnetic resonance imaging scanner itself must be quite powerful - at least 1.5 Tesla.
Clinical examination of patients with Sturge-Weber syndrome
People with Sturge-Weber syndrome should be seen by a multidisciplinary team of physicians trained in the diagnosis and treatment of hereditary neurocutaneous syndromes, which include:
- dermatologist,
- neurologist,
- neurosurgeon,
- neuropsychologist (psychologist),
- ophthalmologist,
- vascular surgeon.
If your child or you have recently been diagnosed with Sturge-Weber syndrome, you probably have many questions about what complications can develop as a result of this disease, and what effective medical examination and treatment entails.
In this case, we recommend that you familiarize yourself with the Useful articles prepared by the staff of the Neurological Center for Epileptology, Neurogenetics and Brain Research at the University Clinic of the Krasnoyarsk State Medical University. Prof. V.F. Voino-Yasenetsky, who have practical experience in managing patients with this pathology.
In addition, you can contact the specialists of our center for a face-to-face consultation.
1Author:
Natalya Alekseevna Shneider, MD, PhD, Professor, Head of the Neurological Center for Epileptology, Neurogenetics and Brain Research at the University Clinic, Head of the Department of Medical Genetics and Clinical Neurophysiology at the Institute of Postgraduate Education of Krasnoyarsk State Medical University named after. Prof. V.F. Voino-Yasenetsky
1Sources:
– Schneider N.A., Shapovalova E.A. Epidemiology of phakomatoses // Bulletin of the Clinical Hospital No. 51. – 2011. – Volume IV, No. 2-3.- P.46-54. – Schneider N.A., Shapovalova E.A., Chesheiko E.Yu., Molgachev A.A., Khamraeva E.Kh. Clinical observation of late diagnosis of brain damage in a 35-year-old woman with Sturge-Weber syndrome // Bulletin of the Clinical Hospital No. 51. – 2011. – Volume IV, No. 2-3.- P. 108-112. – Ryan’s Story // Boston Children’s Hospital https:/…/az/Site2944/mainpageS2944P6.html
Useful links:
- The Sturge-Weber Foundation www.sturge-weber.org
- Sturge-Weber Syndrome Community swscommunity.org
- Hunter's Dream for a Cure Foundation www.huntersdream.org
- Kennedy Krieger Institute www.kennedykrieger.org
- Johns Hopkins Medicine www.hopkinsmedicine.org
- The Johns Hopkins University Dermatology Image Atlas dermatlas.med.jhmi.edu/derm
- Vascular Birthmarks Foundation www.birthmark.org
- Johns Hopkins Department of Neurology/Neurosurgery www.neuro.jhmi.edu
- NINDS Sturge-Weber Syndrome Information Page www.ninds.nih.gov/disorders/sturge_weber/sturge_weber.htm
- STURGE WEBER Foundation UK www.sturgeweber.org.uk
- Sturge-Weber Syndrome Community Canada www.swscommunitycanada.org
- Search PubMed for Sturge-Weber www.ncbi.nlm.nih.gov/PubMed/
© All rights reserved. Link to authors and source is required
Bottom line
Hemianopsia is a neurological disorder that causes blind spots in the visual field of both eyes. This pathology is not an independent disease; it accompanies diseases of a neurological and other nature. Hemianopsia can be congenital, acquired, or genetic. Acquired and congenital pathology can be cured; genetic pathology cannot be corrected. To ensure that the level of vision in a genetic disease does not decrease, symptomatic treatment is carried out. Sometimes you have to be treated for the rest of your life.
Sources used:
- Kvasova M. D. Vision and heredity. - Moscow / St. Petersburg: Dilya, 2002.
- Skoromets A. A. Topical diagnosis of diseases of the nervous system: A guide for doctors. — 1st ed. - L.: Medicine, 1989
- D. Hubel. Eye, brain, vision. — ed. A. L. Byzova. - M.: Mir, 1990.
- Wikipedia article