Classification of cochlear neuritis of the auditory nerve
Cochlear neuritis is the most common reason why a person's ability to perceive sound is reduced. Auditory nerve disease can affect one side, but sometimes hearing loss affects both sides. According to this, they divide:
- unilateral neuritis;
- bilateral neuritis.
Another classification of the disease concerns the degree of clinical development of cochlear neuritis. It shows how long the nerve dysfunction has been occurring and how severely it is affected. Thus, the following three forms of cochlear neuritis are distinguished:
- Acute cochlear neuritis. The period of the disease at this stage is up to four weeks. If you consult a doctor at this stage of the disease, the probability of complete hearing restoration is 70-90%.
- Subacute sensorineural hearing loss. This stage is diagnosed if the nerve damage lasts from one to three months. Treatment is also used here, the probability of recovery is about 30-70%.
- Chronic sensorineural hearing loss, which lasts for 3 months, is difficult to treat.
There are different types of cochlear neuritis according to the nature and level of damage diagnosed by the doctor. Since the disease is neurosensory in nature, nerve dysfunction can have different origins:
- peripheral cochlear neuritis - causes of impaired sound perception in the inner ear;
- central sensorineural hearing loss - the causes of hearing loss are caused by dysfunction of the corresponding structures in the brain.
According to the degree of development of the disease, four stages of cochlear neuritis are distinguished:
- Mild (I) degree, when the threshold for sound perception is 26-40 dB;
- Moderate (II) degree, the auditory limit here reaches 41-55 dB;
- Moderately severe (III) degree, sound perception threshold 56-70 dB;
- Severe (IV) degree, when the auditory limit is 71-90 dB.
If sound perception is almost completely impaired and the patient is unable to hear any sounds, the doctor diagnoses complete deafness.
According to the likely results of treatment, the nature of the course and symptoms, cochlear neuritis is classified into:
- reversible;
- progressive;
- stable.
In addition, cochlear neuritis is distinguished by the cause of the disease.
- Congenital sensorineural hearing loss, which manifests itself in childhood.
- Acquired cochlear neuritis, the cause of which can be many things. According to this, acquired sensorineural hearing loss is also considered as:
- ischemic;
- radial;
- professional;
- post-traumatic;
- allergic.
If cochlear neuritis occurs before a person learns to speak, then this type of disease is called prelingual. If it appears after, then such neuritis is classified as postlingual.
There can be many reasons for the occurrence of cochlear neuritis, and they differ for congenital and acquired hearing loss.
Ischemic cochleovestibular syndromes: algorithm for diagnosis and complex therapy
Ischemic cochleovestibular syndromes (ICVS) are one of the most common causes of dizziness and develop in the presence of circulatory failure in the arteries supplying the inner ear and the root of the VIII nerve, as well as the vestibular nuclei and pathways.
The article proposes an algorithm for diagnosing ischemic cochleovestibular syndromes and describes the principles of treatment of patients with ICVS. Oxidative stress plays a special role in the clinical and morphological picture of ischemia. Using Actovegin as an example, the possibilities of including drugs with neurometabolic effects that improve the survival of neurons under conditions of chronic hypoxia into ICS therapy are considered.
MRI – magnetic resonance imaging; Ultrasound – ultrasound examination; ECG – electrocardiography; EEG – electroencephalography.
Dizziness is one of the most common causes of loss of balance and complaints among patients visiting general practitioners [1]. Dizziness is very often caused by ischemic cochleovestibular syndromes (ICVS), which are a combination of vestibular disorders (dizziness, unsteadiness) with tinnitus and hearing loss. ICVS develops in the presence of circulatory failure in the arteries supplying the inner ear and the VIII nerve root [2], which is caused by increasing manifestations of general cerebral ischemia, chronic cerebral vascular insufficiency and steal syndromes [1, 3–5].
There are peripheral and central cochleovestibular syndromes. Peripheral ICVS is associated with circulatory failure in the small arteries supplying the labyrinth and the VIII nerve [6, 7]. Central cochleovestibular syndrome occurs as a result of ischemia of the vestibular nuclei located in the brain stem [8, 9]. The etiological factors for the development of dizziness in these cases are atherosclerotic damage to extra- and intracranial cerebral vessels (stenosis, occlusion), arterial hypertension, deformation of the vertebral arteries, anomalies of the arteries of the vertebral-basilar system, disorders of hemorheology and hemostasis, arterio-arterial and cardiac embolisms, thrombosis venous sinuses, disturbance of central hemodynamic parameters [10, 11].
Dizziness often occurs with brain tumors, epilepsy, degenerative diseases of the central nervous system, as well as with metabolic disorders (primarily diabetes mellitus, in which the blood circulation of the inner ear is impaired), cognitive disorders, anxiety disorders, and degenerative diseases of the cervical spine. The pathogenesis of all ischemic cochleovestibular syndromes is based on local and cerebral hemodynamic disorders, entailing various forms of functional disorders of the vestibular system. Pathogenetic factors in the development of ICVS are ischemia, disruption of the trophism of labyrinth receptors and labyrinth-dependent brain structures and metabolism as a result of cerebral vascular diseases of various origins and, as a consequence, secondary encephalopathic disorders [12, 13].
It can be assumed that in the pathogenesis of acute ICVS, an important role is played by the obstruction of venous outflow from the transverse sinus during a hypertensive crisis as a result of the opening of arteriole-venous shunts. Often in such patients, “secondary” hydrops of the labyrinth is detected, which is caused by impaired circulation of the inner ear against the background of impaired venous outflow from the cranial cavity and/or external hydrocephalus. Hemolytic fluid dynamics disorders are aggravated by an increase in the activity of lipid peroxidation, a decrease in the main indicators of the antioxidant system, changes (like hypercoagulation) in blood rheology and lipid metabolism indicators. However, an indisputable fact is that the development of cerebrovascular diseases is based on changes in the metabolism and trophism of neurons and neurotransmitter systems [5, 10, 14]. Disturbances in metabolic and protein synthetic processes in the vascular wall and neurons underlie subsequent morphological damage (atherosclerotic or neurodegenerative in nature), which is the foundation for the further development and manifestation of the disease. Equally important is the disruption of neurohumoral regulation processes, in particular neurotransmitter systems, vascular tone and adaptive capabilities of the vascular bed [3]. Depending on the nature of the vascular changes, the pathological focus can be localized both in the “periphery” (in the labyrinth) and at any level of the brain, which is clinically manifested by peripheral and central labyrinthine syndrome.
Symptoms of ICVS have age-related characteristics [15]. This is due to the fact that in old age it is difficult to single out one cause for the development of ICVS; hypercholesterolemia, bending of one or both vertebral arteries, atherosclerotic stenosis (often hemodynamically insignificant) of the internal carotid arteries, and the presence of degenerative changes in the spine can lead to ICVS [16 ]. In elderly and senile age, multiplicity and recurrence of acute ischemic strokes are often observed, especially in the vertebrobasilar system. Clinically, this is manifested by frequent attacks of dizziness, nystagmus, balance and coordination disorders. Chronic cerebral ischemia is reflected by changes in the white matter (leukoaraiosis), primarily in the deep parts of the brain. In elderly patients, a relationship has been identified between the prevalence of leukoaraiosis, especially in the anterior parts of the brain, the localization of lacunar lesions in the lenticular nucleus and the severity of walking and balance disorders [13]. In patients with cognitive disorders, it is difficult to collect a correct history and differentiate complaints, so diagnosing ICVS in this group of patients is difficult.
Diagnosing ICVS in general is challenging. On the one hand, dizziness in different diseases can occur identically, on the other hand, it can have a different clinical picture for the same disease. For example, in outpatients with dizziness, the cause of dizziness is identified only in 20% of cases [4]. In order to make the correct diagnosis and prescribe optimal treatment to the patient, the doctor must adhere to a certain diagnostic algorithm (Fig.).
Research methods for ICVS
First of all, it is necessary to carefully examine the patient, including a detailed history taking and analysis of complaints in order to determine the type of dizziness. Measure blood pressure in a supine and standing position: with a significant decrease in systolic pressure (more than 20 mm Hg) in an upright position, symptoms similar to those of vertebrobasilar insufficiency are usually caused by orthostatic hypotension. During a neurological examination, attention should be paid to the presence or absence of nystagmus, static or dynamic ataxia. Indicative tests are Romberg (the patient, standing with his eyes closed, deviates in the direction of the labyrinth lesion) and Babinsky-Weil (the patient with his eyes closed takes five steps forward and backward several times - with a unilateral vestibular lesion, his route will be shaped like a star). In elderly patients and patients with a complicated history (abuse of alcohol, toxic substances, drugs), neuropsychological testing should be performed to identify cognitive disorders.
Systemic dizziness
Systemic dizziness is the result of impaired functioning of the vestibular analyzer due to its damage [7, 17]. Proprioceptive systemic vertigo is distinguished (a feeling of passive movement of one’s own body in space or a tactile tactile sensation of support moving under the feet or hands, lifting or sinking of the body, feeling “on a wave,” swaying back and forth, left and right, up and down, “walking like a over bumps") and visual systemic vertigo (a feeling of progressive movement of objects in the field of vision). Depending on the level and depth of the lesion, systemic vertigo is classified as peripheral (damage to the vestibular ganglia, semicircular canals) or as central systemic vertigo (damage to the cerebellum, brain stem and, in particular, the vestibular nuclei or their connections with other components of the central nervous system).
Peripheral systemic vertigo is most often associated with inflammatory diseases of the inner ear, viral lesions, Meniere's disease, trauma or ischemia of the labyrinth [3, 18]. Typically, systemic vertigo is paroxysmal in nature, manifests itself more intensely than central vertigo, and is accompanied by severe vegetative symptoms (nausea, repeated vomiting not associated with food intake, pallor (hyperemia) of the face, hyperhidrosis, etc.). Peripheral systemic vertigo is always accompanied by spontaneous nystagmus - clonic, horizontal or horizontal-rotatory of varying degrees of intensity, associated with a harmonious deviation of the torso and arms towards the slow component.
During the acute onset of an attack, patients feel the apparent movement of objects towards the diseased ear, nystagmus is also directed in the same direction (stage of irritation or irritation of the labyrinth), subsequently (in the stage of inhibition of the labyrinth) - a sensation of apparent movement of objects and the direction of nystagmus towards the healthy ear. The duration of attacks can range from several minutes to several hours. There is a positive effect of turning the head (towards the slow component of nystagmus). As a rule, peripheral vestibular vertigo is caused by a unilateral pathological process and is accompanied by hearing impairment and tinnitus on the affected side [19]. In some cases, hearing impairments are not intense and are more often associated with impaired speech intelligibility. Recurrences of attacks are associated with increases or fluctuations in blood pressure, turns of the head and torso, and changes in body position.
The causes of dizziness of central origin are most often vertebrobasilar insufficiency and trauma [3, 18]. In addition, severe neurological diseases can be the cause of central vertigo [20]. In rare cases, isolated vestibular vertigo may be caused by acute cerebrovascular accident [21, 22]. This is how occlusion of the distal branch of the anterior inferior cerebellar artery manifests itself, causing ischemia of the cerebellar patch, occlusion of the median cerebellar branch of the posterior inferior cerebellar artery (when vestibular vertigo occurs without other manifestations of Wallenberg-Zakharchenko syndrome), occlusion of the labyrinthine artery. The artery of the labyrinth supplies blood not only to the peripheral vestibular apparatus, but also to the cochlea, and since the latter is less sensitive to ischemia, there may be no hearing impairment when the artery is occluded.
More than 70% of elderly patients have vertebrobasilar insufficiency [4]. More than half of all ischemic strokes in elderly patients are, to one degree or another, associated with damage to extracerebral arteries, primarily of atherosclerotic origin. In 50% of patients over 60 years of age, atherosclerosis is combined with arterial hypertension [10]. The atherosclerotic process causes changes in cerebral circulation, leading to stenosis and occlusion of the main arteries of the head, deterioration of the possibility of collateral redistribution of blood, an increase in cerebral peripheral vascular resistance, a decrease in cerebral perfusion, oxygen and energy starvation of brain tissue, contributing to the development of discirculatory disorders [4]. Changes in the vascular wall occur with an increase in its permeability, periventricular edema, secondary compression of venules, and a slowdown in venous outflow [2, 5]. A common cause of dizziness in hypertension is increased intracranial pressure: up to 60% of patients with intracranial hypertension suffer from dizziness in combination with hearing loss. Central dizziness often occurs with blood diseases (anemia, thrombocytopenia, thrombophilia, polycythemia). Polycythemia deserves special attention because the arteries of the inner ear are small in diameter. Their blood circulation depends not only on systemic hemodynamics, but also on the rheological properties of the blood. Polycythemia causes severe circulatory disorders, especially in small arteries, and dizziness can also be a leading syndrome [18].
With migraine, dizziness also often occurs in the structure of vascular paroxysms. Each paroxysm, especially a prolonged one, can worsen blood circulation in the ear area [23]. Degenerative diseases of the spine can also lead to dizziness [24]. Osteophytes formed during osteochondrosis and spondylosis deformans in the area of uncovertebral joints have the greatest compressive effect on the vertebral artery. They cause dynamic irritation of its sympathetic plexus only during certain positions or movements in the cervical spine. In addition to mechanical compression, vascular spasm may occur as a result of irritation of the periarterial nerve plexus. Displacement and compression of the vertebral arteries can also be observed as a result of subluxation of the articular processes of the vertebrae. The vertebral artery is injured by the apex of the superior articular process of the underlying vertebra due to pathological mobility between the individual segments (two vertebrae connected by a disc) of the cervical spinal column [16, 25]. Compression of the vertebral arteries is also possible by the neck muscles (scalenus, longus colli, inferior oblique capitis) when they contract in certain positions of the head.
Central vertigo is characterized by a less acute onset, dizziness can be systemic and non-systemic in nature, hearing loss (less severe) or tinnitus is often bilateral in nature, nystagmus is bilateral in nature. With central vertigo, occipital headaches appear, radiating to the neck, sometimes to the parietotemporal region and the orbit, instability is observed when walking and standing (static ataxia), less often dynamic ataxia, indicating transient ischemia of the cerebellar structures. Attacks of sudden falling without loss of consciousness (drop attacks) and syncope often develop. Progression of visual and oculomotor disorders is possible: transient diplopia, attacks of “blurred vision”, “spots” and “zigzags” in the visual field, transient hemianopia - all this indicates ischemia of the occipital lobes of the brain. In addition, memory for current events deteriorates; occasionally, attacks of transient global amnesia occur, when the patient’s working memory (memory ability) is impaired for several hours, the patient is confused and disoriented. Often, dizziness of central origin is accompanied by sleep disturbances, increased fatigue, and autonomic disorders (hyperhidrosis, pallor or cyanosis of the skin) [9]. The general practitioner should remember that a patient with systemic dizziness must be referred for consultation to an otoneurologist.
Unsystematic dizziness
Non-systemic dizziness often occurs with arterial hypotension, asthenic conditions, with chronic somatic diseases, with conditions associated with a decrease in blood volume (anemia, acute blood loss, hypoproteinemia and low plasma volume, dehydration) [9, 13]. When blood pressure drops against the background of ongoing cerebrovascular disease, ischemia often develops in the brain stem, which also manifests itself as non-systemic dizziness [21]. Deficiency of adrenergic effects and, consequently, clinical manifestations of orthostatic hypotension are manifested in the picture of Addison's disease, renal amyloidosis, in some cases of the use of pharmacological agents (ganglionic blockers, antihypertensive drugs, dopaminomimetics such as Nakoma, Madopar and some dopamine receptor agonists), with organic pathology of the heart and blood vessels (with aortic stenosis, ventricular arrhythmia, tachycardia, atrial fibrillation) [3].
The appearance of dizziness is possible with bradycardia due to an increase in the vagal reflex. In this case, there is a decrease in heart rate until loss of consciousness in the absence of any heart disease. This is probably due to the fact that stimuli capable of causing such an unusual autonomic response can come from different organs, the afferent innervation of which is vagal, trigeminal, glossopharyngeal or spinal. The prefainting state is characterized by a feeling of lightheadedness and near loss of consciousness, and there is no true sensation of rotation of the patient himself or the world around him [23]. Unsystematic dizziness is manifested by a sudden onset of general weakness, a feeling of lightheadedness, “darkening in the eyes,” ringing in the ears, a premonition of an imminent fall and loss of consciousness (fainting). In the latter case, that is, when dizziness precedes loss of consciousness (fainting), it is called a presyncope [9]. A presyncope does not necessarily lead to fainting (this depends on the speed and extent of the drop in blood pressure). These conditions can often recur, then the main complaint of the patient will be dizziness.
There are vasodepressor (vasovagal); hyperventilation fainting (syncope); syncope associated with carotid sinus hypersensitivity; cough fainting; nocturic, hypoglycemic, orthostatic and other types of fainting. In all these cases, the patient experiences a feeling of lightheadedness, complains of dizziness and a premonition of loss of consciousness [3, 14, 26]. In such cases, fainting must be differentiated from epileptic seizures using electroencephalography.
Differential diagnosis of ICVS with dizziness of other etiologies
Differential diagnosis of ICVS should be carried out taking into account the characteristic features of certain pathological conditions. Psychogenic dizziness is observed as part of anxiety and depressive disorders. This is the most difficult section of neurological diagnostics. The prevalence of psychogenic dizziness reaches 12–15% of cases. The diagnosis is established in the absence of a morphological cause or any focal damage. In addition, dizziness can be a manifestation of somatized depression - neuroses with phobic disorders, vegetative paroxysms, pathological personality changes during hysteria [27]. Physiological dizziness occurs when the vestibular apparatus is overstimulated. It is observed in the case of a sharp change in movement speed (sickness), due to prolonged rotation, when observing moving objects, being in a state of weightlessness, etc.
Sometimes they are perceived and described by patients as conditions resembling dizziness, imbalance and gait disturbances (dysbasia), associated with paretic, atactic, hyperkinetic, akinetic, apractical or postural disorders [9]. The causes of imbalance caused by changes in the efferent part of the motor act include normal pressure hydrocephalus, Parkinson's disease, chronic subdural hematoma, tumors of the frontal lobes, as well as taking a number of medications - anticonvulsants (phenytoin, phenobarbital, carbamazepine), benzodiazepines, neuroleptics (phenothiazines, haloperidol ), lithium preparations. The most pronounced disorders develop with cerebellar disorders, tumors of the cerebellopontine angle, temporal bone and posterior cranial fossa. They are characterized by a feeling of instability, difficulty walking or maintaining a certain posture, and possibly increased discomfort when performing actions that require precise coordination of movements. Characteristically, symptoms worsen in the dark. Systemic dizziness is observed much less frequently with this pathology. In the vast majority of cases, concomitant neurological symptoms are detected.
In acute traumatic brain injury, especially with a fracture of the temporal bone pyramid, dizziness is noted as the leading syndrome. Virtually every concussion has a cervical component due to ballistic changes in the head-to-spine mass ratio [8, 9]. Cervical whiplash often occurs in a car accident when there is sudden hyperextension, then sudden hyperflexion in the cervical spine. Difficulties in diagnosis are due to the fact that symptoms of dizziness do not appear in the acute period, but 1–2 weeks after the injury, and the injury occurs in the absence of visible injuries to the neck. The cause of dizziness is pathological proprioceptive pulsation associated with injury to the soft tissues of the neck and spinal joints [18]. It must be remembered that dizziness can be part of the structure of a convulsive seizure when the epileptogenic focus is localized in the temporal lobe of the brain. Dizziness can occur as the only symptom, which then ends on its own (a discharge that occurs in the form of dizziness), and can also be part of the structure of a partial seizure of secondary origin. The onset of the attack in these cases develops with dizziness followed by the development of tonic-clonic convulsions. In such cases, the patient's examination should include electroencephalography [4].
An attack of Meniere's disease resembles an attack in peripheral cochleovestibular syndrome, but is much shorter in duration, and the course of the disease is recurrent. A sudden unexpected attack of pronounced systemic dizziness appears in combination with nausea and often vomiting, decreased hearing in one ear (or noise in it), spontaneous nystagmus with a short duration (1-3 hours) and complete relief of all symptoms. Characteristically, there are no other neurological symptoms or changes in the blood vessels of the brain (during examination). Dizziness may also accompany multiple sclerosis. The disease is relapsing in nature and is typically characterized by a combination of vestibular and cerebellar disorders with other symptoms of multiple sclerosis. Magnetic resonance imaging of the brain reveals areas of white matter demyelination. For tumors of the cerebellopontine angle (neurinoma of the VIII nerve), an early sign is damage to auditory function (sharp hearing loss, usually in one ear); less commonly, vestibular dysfunction (dizziness is not pronounced), often with damage to other nearby cranial nerves; in the later stages, balance disorders are added. The diagnosis can be confirmed by magnetic resonance imaging.
Additional examination methods
Additional examination methods include the classic and advanced otoneurological method using data from computer electronystagmography, audiometry, auditory evoked potentials, the study of central hemodynamics, determination of hemorheological parameters, ultrasound methods for studying cerebral blood flow (duplex scanning, transcranial Dopplerography), computer and magnetic resonance imaging brain, magnetic resonance angiography and radioisotope angioscintigraphy of the brain. If a spondylogenic effect on the vertebral artery is suspected, radiography or magnetic resonance imaging of the cervical spine is performed.
Choice of ICS therapy
The main principles of ICS therapy are preventing the onset or progression of the pathological process, improving cognitive functions and taking general therapeutic measures [6, 10, 26]. ICVS therapy should be comprehensive and include drugs with multidirectional mechanisms of action. In order to prevent secondary ischemic disorders, it is necessary to prescribe antiplatelet agents (acetylsalicylic acid, ticlopidine, dipyridamole), and in case of increasing symptoms, anticoagulants [24]. Treatment of systemic dizziness is largely determined by its cause; in addition, symptomatic therapy plays an important role [4]. A clear distinction should be made between so-called “emergency” therapy and long-term therapy [12]. Early and long-term use of vestibulolytic drugs is necessary. An example of such drugs is betahistine dihydrochloride, which has an effect on histamine H₁ and H₃ receptors and improves microcirculation in the labyrinth and neurotransmission in the area of the vestibular nuclei of the central nervous system [6]. The use of this drug does not provide a quick clinical effect, but requires compliance with the dosage regimen (daily dose 48 mg) and long-term use (at least 1 month).
“First aid” therapy for ICVS should be carried out with drugs that have vasoactive, neuroprotective and metabolic properties (Vasobral, Cavinton). It is extremely important that this therapy is aimed at correcting local pathophysiological mechanisms - impaired tone of cerebral arteries and veins, metabolic processes in the brain, hemorheology and microcirculation [12]. The clinical effect of these drugs is usually achieved within 10–14 days. The duration of the course of treatment and the choice of drug are determined by the doctor individually. Due to a decrease in the tone of the cerebral veins and disturbances of venous outflow, venotonics are successfully used. Due to the fact that oxidative stress plays a special role in the clinical and morphological picture of ischemia, drugs with neurometabolic effects are used that improve the survival of neurons under conditions of chronic hypoxia (Actovegin).
Actovegin is a deproteinized hemoderivative from the blood of calves, containing low molecular weight peptides and nucleic acid derivatives [28]. It should be noted the activating effect of Actovegin on the energy metabolism of cells of various organs [11, 19, 22]. This is due, first of all, to the ability of the drug to increase the uptake and utilization of glucose and oxygen, leading to an improvement in aerobic energy production in the cell and oxygenation in the microcirculatory system. At the same time, anaerobic energy exchange in the vascular endothelium improves, accompanied by the release of endogenous substances with powerful vasodilating properties - prostacyclin and nitric oxide. As a result, organ perfusion improves and peripheral resistance decreases [18]. Activation of oxygen energy exchange in almost all organs that are in a state of metabolic insufficiency contributes to increased metabolism of high-energy phosphates in the cell, activation of oxidative phosphorylation enzymes and acceleration of the synthesis of carbohydrates and proteins and the breakdown of anaerobic glycolysis products [20]. An increase in oxygen consumption by various tissues under the influence of hemodialysate has been demonstrated in in vitro experiments, in animal models and in humans [5, 8, 9, 12, 14, 16, 22, 25]. Studies on healthy volunteers have shown that under conditions of hypoxia, the drug not only increases oxygen consumption, but also promotes its accumulation, that is, the maximum effect of the drug is manifested precisely in conditions of oxygen deficiency.
Actovegin has an insulin-like effect, which increases the effectiveness of its use in patients with ICVS due to diabetes mellitus. It stimulates the transport of glucose into the cell without affecting insulin receptors [19]. It is assumed that Actovegin takes part in the final stage of activation of glucose carriers present in the membrane [20]. In terms of activity in relation to intracellular glucose transport, the drug is only two times inferior to insulin. In addition, Actovegin stimulates (up to 5 times) lipid biosynthesis. This effect is also insulin-independent and is not affected by insulin antibodies. The drug has a pronounced inhibitory effect on the lipolytic effect caused by stimulation of the adrenergic system. Actovegin has a positive effect on impaired cerebral metabolism during ischemia, providing noticeable changes in the accumulation of glucose, adenosine triphosphate and lactate under the influence of the main substrates of the drug [17]. In addition to cases of general cerebral ischemia, hemodialysate has been successfully used to improve the energy status of cells in lesions of the hippocampus.
Actovegin has both a central effect, stimulating cerebral metabolic processes, and a fairly pronounced effect in peripheral arterial disorders. This mechanism ensures stabilization of the functional metabolism of tissues under conditions of temporarily induced stress and hypoxia during peripheral ICVS [8]. Actovegin is most effective when used in high doses – from 800 mg to 4 g [15, 22]. In patients with ICVS, the drug is prescribed in doses of 800–1200 mg/day intravenously for 10 days, followed by switching to oral administration at 200 mg 3 times/day for 1–3 months. The advantages of Actovegin include its low toxicity and good tolerability. The only contraindication to the use of the drug is hypersensitivity. In most studies, drug tolerability was assessed as “very good” and “good” [17, 20, 22]. In rare cases, hypersensitivity reactions have developed. Discontinuation of the drug due to poor tolerability was extremely rare in clinical studies.
Understanding the mechanism of action of drugs expands the range of possibilities for drug therapy for ischemic cochleovestibular syndromes [26]. The final conclusion about the effectiveness of the chosen treatment and the need for its correction can be made in the absence of a therapeutic effect after 2-3 courses lasting at least 3 months. You should not refuse the chosen drug unless its dose has been increased to an individual maximum and well tolerated. In case of insufficient effectiveness, but good tolerability of the drug substance, another drug from a different class can be added to the selected drug. However, despite the fact that new opportunities have appeared in the arsenal of doctors, many unresolved questions remain. Apparently, it is necessary to radically reconsider approaches to the study of this topic, to define strict criteria for the prescription, combination and dosage of drugs.
Conclusion
Thus, the prevalence of dizziness in patients with cerebral ischemia and the complexity of drug correction of its negative consequences is one of the most complex and pressing problems of modern medicine. Research in this area is of great importance for clinical practice. The use of the proposed algorithm will allow us to systematize knowledge about the causes, types and possibilities of drug correction of ICVS.
Causes of congenital cochlear neuritis
Congenital cochlear neuritis, symptoms of which appear from birth, may occur due to genetic abnormalities, illnesses suffered by the mother during pregnancy, or problems during the birth process.
- Hereditary hearing loss can occur due to Waardenburg syndrome, branchiootorenal syndrome, Refsum disease, Alport syndrome, Stickler syndrome.
- Diseases suffered by the mother during pregnancy that can cause cochlear neuritis. Among them are: rubella, meningitis, syphilis, influenza, otitis media, mumps, herpes, ARVI.
- Problems during childbirth can cause damage to the auditory nerve. For example, such a disease can be caused by fetal hypoxia, premature birth, weakness of labor or its incoordination, birth trauma, or a narrow pelvis of the laboring mother.
Causes of acquired cochlear neuritis
Acquired cochlear neuritis in a third of cases is caused by inflammatory and infectious diseases. In addition, damage to the auditory nerve is caused by drugs, impaired blood supply, injury, and allergies.
- Infections and inflammatory processes that can cause cochlear neuritis include: ARVI, influenza, rubella, scarlet fever, mumps, syphilis, typhus and syphilis.
- Toxic effects of drugs, for example, antibiotics, anti-arrhythmia drugs; medications containing heavy metals or phosphorus.
- Trauma to the skull, tumors that can damage the auditory nerve.
- Arterial thrombosis, atherosclerotic plaques that disrupt cerebral circulation and blood supply to the auditory nerve.
- Long-term professional activity associated with constant exposure to noisy environments, loud sounds or vibrations.
- Age-related cochlear neuritis associated exclusively with gradual changes in the auditory nerve.
Symptoms of cochlear neuritis
Both unilateral and bilateral cochlear neuritis are characterized by two main symptoms that are constantly present:
- hearing loss (decreased);
- feeling of constant noise.
These manifestations of the disease may be complemented by other problems with the perception of sound, for example, a shift in the sense of the sound source. There are disorders of the vestibular apparatus, dizziness, vomiting, nausea. These symptoms are more characteristic of chronic cochlear neuritis.
Due to the fact that the disease affects the auditory nerve and the perception of sounds is difficult, children with cochlear neuritis suffer from psycho-emotional problems, moral disorders, and difficulties with speech. There is a decrease in the emotional background, isolation, and isolation from society.
3. Symptoms and diagnosis
The most typical manifestations of cochlear neuritis, in addition to hearing loss itself, are sensations of constant extraneous noise in the head and asymmetrical hearing loss. Some patients also experience a complex of vestibular disorders (dizziness, coordination and balance disorders, unsteadiness of gait, etc.).
Obviously, any hearing loss, incl. caused by cochlear neuritis, is a socially significant problem, since it leads to disruptions in communication and social functioning, requires the use of hearing aids, in many cases limits or excludes professional suitability, and provokes the development of psychological disorders of the depressive register.
The degree of functional failure of the auditory analyzer is established in a series of audiometric, tuning fork and other similar tests. Otoscopy and microotoscopy are performed; Electrocochleagraphy, vestibulometric studies, consultations (and corresponding examinations) of specialized specialists, and a battery of laboratory tests are also prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnosis of cochlear neuritis
In order to begin treatment of the disease, it is necessary to conduct a broad diagnosis of this problem. As already mentioned, cochlear neuritis exists in a wide variety of types and types and can be classified and defined into groups. Therefore, the doctor needs to conduct many tests, analyzes and procedures in order to fully describe the disease, identifying all aspects of cochlear neuritis and determining its genesis, causes, symptoms, period of occurrence, etc. This is a meticulous process, difficult at an early stage both if there is unilateral and bilateral cochlear neuritis.
The degree of damage to the auditory nerve is determined using audiometry or acoustic impedance testing. Additionally, the ability of the vestibular apparatus to respond to stimuli and load is studied. To determine the nature of the disease, various tests and analyzes are carried out; separately, using computed tomography, x-rays or magnetic resonance imaging, the vascular system, cranial bones, and human brain are studied.
To clarify the diagnosis and check its truth, manipulations are carried out aimed at detecting other diseases. Thus, the patient can be checked for otitis media, cerumen impaction, and otosclerosis using endoscopy or otoscopy.
After other possible options have been excluded from the diagnostic field, the doctor narrows the search and not only records the disease, but also characterizes it, describing the type, variety, and possible cause that caused it.
Prices
| Disease | Approximate price, $ |
| Prices for diagnosis and treatment of sinus pathologies | 10 370 — 17 560 |
| Prices for the treatment of thyrotoxic goiter | 22 590 — 22 670 |
| Prices for treatment of laryngeal cancer | 6 170 — 77 000 |
| Disease | Approximate price, $ |
| Prices for diagnosing migraine | 7 060 — 8 260 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for brain shunting for hydrocephalus | 33 180 |
| Prices for treatment of Parkinson's disease | 58 600 |
| Prices for migraine treatment | 9 680 |
| Prices for the diagnosis of amyotrophic lateral sclerosis | 6 550 |
| Prices for diagnosing epilepsy | 3 520 |
| Prices for rehabilitation after a stroke | 78 300 — 82 170 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of multiple sclerosis | 4 990 — 17 300 |
Otolaryngology in Israel receives extremely positive reviews, and the reason for this is not only the high effectiveness of the treatment, but also its affordable cost for most medical tourists. Prices for diagnostic and treatment procedures in Israeli hospitals are at least a third lower than in similar medical institutions in Western Europe, the USA, Canada and other countries with developed medicine.
The cost of treatment for an ENT disease in Israel depends on its nature, location, stage of development, medications used, the number and type of diagnostic procedures required, therapeutic methods, as well as the individual characteristics of the patient. You can find out the approximate cost of solving a particular ENT problem from a medical representative of the clinic during a free consultation. The final cost will be clear on the spot, after all examinations have been completed and the treatment plan has been approved by the doctor.
Treatment of cochlear neuritis
The goal of treatment for this disease is complete or partial restoration of hearing. If the patient is sick with a chronic form of cochlear neuritis, treatment is prescribed aimed at stabilizing the existing condition and preventing its deterioration. In other cases, cochlear neuritis may respond to various forms of treatment, both in a hospital and in a regular setting.
Drug treatment is used, usually prescribed intravenously. Vasodilator drugs, venotonics, neuroprotectors and disaggregants are indicated for administration over a period of two weeks. Then they move on to another stage of treatment, when the medicine can be taken orally or administered intramuscularly.
If hearing loss was caused by intoxication, first a course of procedures is carried out to remove harmful substances from the body, such as heavy metals, arsenic, phosphorus. After the toxic element is eliminated, treatment is prescribed.
The symptoms of the disease are also relieved, eliminating pain, dizziness, nausea, and vestibular disorders, if any.
In addition to treatment with medications, manipulations are also prescribed. With the wide possibilities of modern ENT medicine, procedures such as electrical stimulation, oxygen barotherapy, electro-, laser-, acupuncture, as well as phonophoresis are successfully used.
This range of treatment options is indicated for those types of disease where there is a possibility of complete or partial restoration of hearing. If the task is such that it is necessary to maintain the patient’s existing health condition, or as an additional therapy, hearing prosthetics may be prescribed.
Hearing aids are indicated not only to make it easier for patients to perceive sounds, but also to restore speech function. Linear, analog, and digital hearing aids are used. In order for the prescribed prosthesis to function correctly, its adjustment and selection must be carried out by a specialized ENT professional.
Surgical intervention, the possibility of which we mentioned earlier, is indicated if cochlear or brainstem implantation is required, or hearing impairment is caused by injury, tumor or neoplasm, the removal of which is necessary. In addition, the operation will be performed on those patients for whom the symptom of dizziness or noise becomes painful.
If the patient has a severe form of cochlear neuritis, then surgery may be aimed at manipulating the cochlea.
Case from practice
In March 2007, the parents of patient K., born in 2005, came to the St. Petersburg Research Institute of ENT with complaints about the child’s lack of reaction to sounds and lack of speech. During the examination, a diagnosis was made: Chronic bilateral sensorineural hearing loss of IV degree, congenital etiology. Secondary receptive and expressive language disorder. Consequences of intrauterine cytomegalovirus infection, intrauterine damage to the central nervous system. Residual organic damage to the central nervous system. Left-sided spastic upper monoparesis. Aplasia of the first finger of the left hand. Hip dysplasia. Spasmodic torticollis. Pelvic dystopia of the hypoplastic right kidney. Delayed psychomotor development.
According to the conclusion of a child psychologist, the child’s cognitive abilities are within the age norm, intelligence is preserved.
The child received binaural hearing aids with heavy-duty hearing aids, without effect. According to the audiological examination, short-latency auditory evoked potentials were not recorded at a maximum signal level of 103 dB, and otoacoustic emissions were not recorded on both sides.
When conducting game audiometry in hearing aids, reactions to sounds with an intensity of 80-95 dB in the frequency range from 250 to 1000 Hz were revealed.
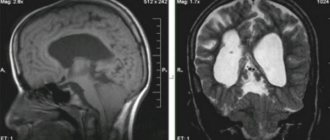
CT scan of the temporal bones revealed the presence of a bilateral anomaly of the cochlea in the form of incomplete division of type I (Table 4). Moreover, this statement is true for both the left and right ears, despite the seemingly different picture (Fig. 1).
After the examination, the patient underwent CI on the left ear using the classical approach through anthromastoidotomy and posterior tympanotomy, with the introduction of an electrode through a cochleostomy. For the operation, a special shortened electrode (Med-El, Austria) was used, having a working length of the active electrode of about 12 mm, specially designed for use in cases of anomaly or ossification of the cochlea.
Despite the intact auditory ossicles and stapedius muscle tendon, acoustic reflexes from the stapedius muscle were not recorded during the operation. However, when performing neural response telemetry, clear responses were obtained when 7 out of 12 electrodes were stimulated.
Postoperative transorbital radiography of the cochlea revealed that the active electrode of the implant is located in the common cavity (Fig. 4, arrow), taking the shape of an ideal circle.
During a control audiological examination one year after surgery, the patient was found to have reactions in the free sound field to sounds with an intensity of 15-20 dB in the frequency range from 250 to 4000 Hz. The patient’s speech is represented by one- and two-syllable words (“mom”, “give”, “drink”, “kitty”, etc.), a simple phrase of no more than two one- or two-syllable words. Considering that the patient’s age at the time of the re-examination was less than 3 years, the results of auditory-speech rehabilitation in this case should be considered excellent.
Prognosis for cochlear neuritis
The prognosis for the effectiveness of treatment for cochlear neuritis largely depends on the duration and symptoms of the disease. Modern and proven ENT techniques show themselves very well, having proven to be truly effective and efficient solutions to this problem, however, if cochlear neuritis was diagnosed at a late stage, then no medicine can help here. However, in the case when the patient consults a doctor on time, for example, at the stage of acute cochlear neuritis, the probability of recovery and complete restoration of hearing is 50%. Partial hearing restoration is guaranteed for another third of patients.
Chronic cochlear neuritis is practically untreatable; drug and procedural intervention will help little, but the efforts of doctors will be aimed at stabilizing and maintaining the current state of human health. It is important to prevent regression and further damage to the auditory nerve. This is why such patients are prescribed hearing prosthetics: it minimizes the likelihood of further deterioration of the condition, since it significantly facilitates the functioning of the auditory system, preventing it from overstraining.
Doctors repeatedly emphasize the importance of promptly going to the hospital in case of damage to the auditory nerve. Both if cochlear neuritis occurs suddenly, and if it bothers the patient for a certain period of time, it is necessary to go to a specialist. Early diagnosis can save your hearing or prevent it from deteriorating further. Remember that your health is the most important thing, and hearing problems are far from local in nature: damage to the auditory nerve entails disturbances in speech, and therefore in socialization, behavioral sphere, emotional background, mental and moral state.
Literature
- Jackler RK Congenital malformations of the inner ear: a classification based on embryogenesis//RK Jackler, WM Luxford, WF House/ Laryngoscope. – 1987. – Vol. 97, no. 1. – P. 1 – 14.
- Jackler RK The large vestibular aqueduct syndrome//RK Jackler, A. De La Cruz/ Laryngoscope. – 1989. – Vol. 99, No. 10. – P. 1238 – 1243.
- Marangos N. Dysplasien des Innenohres und inneren Gehörganges//N. Marangos/HNO. – 2002. – Vol. 50, no. 9. — P. 866 – 881.
- Sennaroglu L. A new classification for cochleovestibular malformations//L. Sennaroglu, I. Saatci/Laryngoscope. – 2002. – Vol. 112, No. 12. – P. 2230 – 2241.
- Siebenmann F. Grundzüge der Anatomie und Pathogenese der Taubstummheit// F. Siebenmann/Wiesbaden: JF Bergmann; 1904. – 76s.
- Stellenwert der MRT bei Verdacht auf Innenohrmissbildung//S. Kösling, S. Jüttemann, B. Amaya et al. / Fortschr Röntgenstr. – 2003. – Vol. 175, No. 11. – S. 1639 – 1646.
- Terrahe K. Missbildungen des Innen- und Mittelohres als Folge der halidomidembryopathie: Ergebnisse von Röntgenschichtuntersuchungen//K. Terrahe/Fortschr Röntgenstr. – 1965. – Vol. 102, No. 1. – P. 14.
The head of the department for the development and implementation of high-tech treatment methods is Doctor of Medical Sciences, Professor Anikin Igor Anatolyevich. Clinic phone number
Commission for the selection of patients for the provision of high-tech medical care Secretary of the commission - candidate of medical sciences Vladislav Evgenievich Kuzovkov, phone
Schedule of consultation appointments with clinic staff