Vertebral (vertebral) artery syndrome is the definition of a group of syndromes (vascular, autonomic) resulting from impaired blood flow in the vertebral arteries caused by various problems. The main etiological causes of the development of vertebral artery syndrome are the following diseases.
- Vascular diseases with impaired vascular patency, such as atherosclerosis, various arthritis, embolism.
- Changes in the shape of the arteries (deformations) - abnormal tortuosity, significant kinks, abnormal structural changes in the arteries.
- Extravasal vascular compression (compression of arteries by osteophytes, hernias, disc protrusions, compression by bone abnormalities, tumors, scar tissue)
Considering that the syndrome can be caused by various factors, sometimes difficulties arise with the interpretation of such a diagnosis as vertebral artery syndrome , since this syndrome can designate a variety of conditions, for example, acute circulatory disorders. But in clinical practice, the most important are degenerative-dystrophic changes in the cervical spine and abnormal phenomena in the atlas, which lead to disruption of blood flow in the vertebral arteries and the appearance of symptoms of cerebrovascular accident.
There are extracranial and intracranial sections of the vertebral artery.
A significant part of the extracranial section of the vertebral arteries passes through a mobile canal formed by openings in the transverse processes of the vertebrae. The sympathetic nerve (Frank's nerve) also passes through this canal. At the C1-C2 level, the vertebral arteries are closed only by soft tissue. This anatomical feature of the passage of the vertebral arteries and the mobility of the cervical spine significantly increase the risk of developing compression effects on the vessels from surrounding tissues.
The resulting compression from surrounding tissues leads to compression of the artery of the autonomic endings and constriction of blood vessels due to reflex spasm, which leads to insufficient blood supply to the brain.
Degenerative changes in the cervical spine (osteochondrosis, arthrosis of the facet joints, uncovertebral arthrosis, instability of motor segments, disc herniations, spondylosis deformans, bone growths (osteophytes), muscle reflex syndromes (inferior oblique muscle syndrome, anterior scalene muscle syndrome) are often the cause of compression vertebral arteries and the development of vertebral artery syndrome . Most often, compression occurs at the level of 5-6 vertebrae, slightly less often at the level of 4-5 and 6-7 vertebrae. The most common cause of the development of vertebral artery syndrome is uncovertebral syndrome. The close location of these joints to the vertebral arteries leads to the fact that even small exostoses in the area of uncovertebral joints lead to mechanical effects on the vertebral arteries.With significant uncovertebral exostoses, significant compression of the lumen of the vertebral arteries is possible.
Anomalies of Kimberly and Powers play a fairly significant role in the development of vertebral artery syndrome.
1.General information
Cochlear neuritis is a collective diagnosis that generalizes the condition of hearing loss due to damage to the auditory nerve; The terms “sensorineural hearing loss” and “sensorineural hearing loss” are also widely used (in some cases as a synonym, in others as a designation of an axial symptom).
Unlike the vast majority of diagnoses ending in “-itis,” cochlear neuritis does not imply the dominant etiopathogenetic significance of infectious and inflammatory processes. Some authors, defining the scope and content of this concept, generally insist on the non-infectious nature of the lesion; in other sources the significance of the inflammatory factor is veiled, etc. Generally speaking, the formulation “cochlear neuritis” refers to those diagnoses that are perceived and interpreted (even by specialists) more on an intuitive than on a rational level. The English term “Auditory neuropathy” seems to be somewhat more successful.
One way or another, hearing loss caused by lesions of auditory neural conductors is widespread: according to modern data, this is the most common cause of partial or complete hearing loss. At the same time, epidemiological estimates published in different sources differ significantly. As a first approximation and taking into account WHO reports, the total number of hearing impaired people in the world is at least 300 million people. According to other sources, this figure is even higher and reaches 10% of the world's population, of which 125 million people are actually disabled (three quarters of them are residents of the poorest countries). In Russia, the number of socially significant hearing loss is estimated at 13 million people, with at least a million being children and adolescents.
Thus, partial or complete hearing loss is one of the global health problems, and its severity is dramatically aggravated by the fact that today there are no truly effective methods for treating cochlear neuritis as the dominant etiopathogenetic factor of hearing loss.
A must read! Help with treatment and hospitalization!
Ischemic cochleovestibular syndromes (ICVS) are a combination of vestibular disorders (dizziness, instability) with tinnitus and hearing loss. ICVS are one of the most common forms of vertigo and develop with circulatory failure in the arteries supplying the inner ear, the VIII nerve root, the vestibular nuclei and their pathways [1]. As a rule, the development of ICVS is caused by increasing manifestations of cerebral ischemia [6, 7].
There are peripheral and central ICVS. Peripheral is associated with circulatory failure in small arteries supplying the labyrinth and VIII nerve [2, 14]. Central ICVS occurs as a result of ischemia of the vestibular nuclei of the brainstem [11, 17].
In rare cases, isolated vestibular vertigo may be caused by acute cerebrovascular accident due to occlusion of the distal branch of the anterior inferior cerebellar artery causing ischemia of the cerebellar flocculus, occlusion of the branches of the posterior inferior cerebellar artery, or occlusion of the labyrinthine artery [5].
Mechanisms of risk for developing ICVS
The main mechanisms for the development of ICVS are atherosclerotic lesions of extra- and intracranial cerebral vessels, arterial hypertension (AH), severe deformation of the vertebral arteries (VA), anomalies of the arteries of the vertebral-basilar system (VBS), disorders of the hemostatic system, arterio-arterial and cardiac embolism , severe disturbances of central hemodynamics [10, 11].
Atherosclerosis of the cerebral arteries is considered to be the most common cause of ICVS. The atherosclerotic process causes impaired cerebral circulation due to the formation of stenoses or occlusions of the main arteries of the head and/or intracranial arteries, deterioration of collateral redistribution of blood, increased cerebral peripheral vascular resistance, decreased cerebral perfusion, oxygen and energy starvation of brain tissue [7]. It should be noted that with age, the adaptation capabilities of patients to both exogenous and endogenous influences decrease. More than half of all ischemic strokes in the elderly are, to one degree or another, associated with damage to extracerebral arteries, primarily of atherosclerotic origin. In 50% of patients over 60 years of age, atherosclerosis is combined with hypertension [10].
Brain damage in hypertension is caused by a complex of disorders such as carotid and VA tortuosity, thickening of the intima-media complex, endothelial dysfunction, and impaired cerebrovascular reactivity. In this case, reparative and adaptive processes occur, hypertrophy of the muscular lining of extracerebral vessels develops with the appearance of “hypertensive stenoses” and subsequent obliteration of the lumen. Recalibration of arteries leads to a reduction in cerebral blood flow and ischemia of brain tissue [3–5]. The anatomical features of the blood supply to the brain are such that with uncontrolled hypertension, the deep parts of the white matter of the brain, the subcortical basal ganglia and the cerebellum are primarily affected. These parts of the brain are most often the area of localization of lacunar infarctions. Pathomorphological studies of the cerebral venous system in hypertension indicate its pronounced disorders, up to obliteration of the cerebral venous sinuses. Changes in the vascular wall occur with an increase in its permeability, periventricular edema, secondary compression of venules, and a slowdown in venous outflow [1, 24]. The state of microcirculation is also disrupted - platelet deformability worsens, hematocrit increases, and blood viscosity increases.
In addition to organic damage to extra- and intracranial vessels, there is a so-called stress-causing pathogenetic variant of the development of ICVS,
caused mainly by the depletion of energy metabolism and deterioration of blood circulation in the brain as a result of overstrain of the cerebral systems against the background of prolonged exposure to activating unconditioned and conditioned reflex stimuli [9].
Degenerative-dystrophic diseases of the spine can also lead to the occurrence of ICVS due to disruption of the perivascular plexuses and the lower cervical sympathetic ganglion, which provide sympathetic innervation to the VA [3, 16]. The possibility of damage to the VA in degenerative lesions of the cervical spine is determined by its topographic and anatomical features. A significant part of the extracranial segment of the VA is located in a mobile bone canal passing through the transverse processes of the cervical vertebrae. In this area, the lateral wall of the VA is adjacent to the uncovertebral joint, and the posterior wall is adjacent to the superior articular process. At the CI-CII level, the PA is covered only by soft tissues, mainly by the inferior oblique muscle of the capitis. Under physiological conditions, when there is compression and restriction of blood flow in one of the arteries, the flow of blood to the brain is usually not impaired due to sufficient compensatory capabilities. The situation changes with hypoplasia or the presence of atherosclerotic stenosis of one of the VAs. In this situation, extravasal factors (compression by articular processes due to instability of the cervical spine or osteophytes in uncovertebral areas, etc.) become the main causes of circulatory failure in the VBS. It is believed that it is osteophytes that have the greatest compressive effect on the VA; they can cause irritation of the sympathetic plexus only in certain positions or movements in the cervical spine. In addition to mechanical compression, vascular spasm is possible as a result of irritation of the periarterial nerve plexus. Displacement and compression of the VA can also be observed as a result of subluxation of the articular processes of the vertebrae. In addition, due to the pathological mobility of individual vertebral motor segments of the cervical spine, the VA can be injured by the apex of the superior articular process of the underlying vertebra [23, 25]. It is also possible that the VA may be compressed by the neck muscles (scalenus, longus colli, inferior oblique capitis) in certain head positions. Most often, the VA is compressed in the area between the V and VI cervical vertebrae, somewhat less often - between the IV and V, VI and VII vertebrae [26]. Due to the proximity of the VA to the atlantoaxial joint, where the common fascial sheath of the neurovascular bundle is adjacent to the outer layer of its capsule, a decrease in blood flow through the VA is possible with lateral tilt or rotation of the axis tooth [9, 28]. Coming out of the transverse process of the atlas, the VA is directed back horizontally and lies in the sulcus of the VA. In some people, a bone bridge forms above the groove - Kimmerle's anomaly, which can have a compression-irritative effect with a sharp decrease in blood flow in the VA. As a rule, in clinical practice, ICVS develop with mixed (compression-irritative) types of VA lesions.
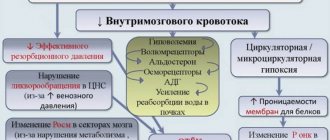
Pathogenesis of ICVS
ICVS is based on hemodynamic disturbances, which entail various forms of functional disorders of the vestibular system. The pathogenetic basis of ICVS is ischemia, disturbances in the trophism of the receptors of the labyrinth and associated brain structures and metabolism in them due to vascular damage to the brain [14, 15, 18, 19]. These disorders are determined by a combination of factors: the state of metabolism in the brain tissue, oxygen tension (pO2), carbon dioxide (pCO2), acid-base state and pH of brain tissue, the level of systemic blood pressure, local neurogenic regulation of vascular tone, including impulses from the vasomotor center of different parts of the brain stem and hypothalamus, from the nerve plexus of the tympanic cavity [1].
Depending on the nature of changes in the vascular bed, the ischemic zone can be localized both in the periphery (in the labyrinth) and in other parts of the brain, which clinically, in addition to other symptoms, can manifest as peripheral or central ICVS. It can be assumed that the obstruction of venous outflow from the transverse sinus during a hypertensive crisis as a result of the opening of arteriole-venous shunts plays a role in the pathogenesis of acute ICVS. Often in such patients, secondary hydrops of the labyrinth is detected, caused by impaired circulation of the inner ear against the background of impaired venous outflow from the cranial cavity. Disorders of liquor dynamics are aggravated by an increase in the main parameters of lipid peroxidation, a decrease in the efficiency of the antioxidant system, hypercoagulation and hyperaggregation of platelets, and lipid metabolism disorders.
The development of cerebrovascular diseases is based on changes in the metabolism and trophism of neurons and dysfunction of neurotransmitter systems [22, 24]. Disturbances in metabolic and protein synthetic processes in neurons underlie neurodegenerative damage, which is the basis for further progression of the disease. Equally important are disturbances in the functioning of neurotransmitter systems and regulation of vascular tone, which reduce the adaptive capabilities of the vascular bed.
Clinical manifestations of ICVS
Peripheral ICVS is characterized by an acute onset, pronounced systemic dizziness, accompanied by nausea, vomiting, and sometimes loss of consciousness, combined with unilateral hearing loss, a sensation of tinnitus, and nystagmus. In some cases, hearing impairment is mild and manifests itself only as impaired speech intelligibility. Central ICVS is characterized by a subacute onset, a combined systemic and non-systemic nature of dizziness, a gradual bilateral hearing loss or sensation of tinnitus, and bilateral nystagmus. Characterized by occipital headaches, sometimes radiating to the neck, parietotemporal region and orbits, instability when walking and standing (static ataxia), less often - dynamic ataxia. Attacks of sudden falling without loss of consciousness (“drop attacks”) and syncope are possible. Some patients have visual and oculomotor disorders in the form of transient diplopia, photopsia, and transient hemianopsia. Often there is a decrease in memory for current events, attacks of transient global amnesia, when the patient’s ability to remember is impaired for several hours while the ability to carry out purposeful actions is preserved. To a certain extent, this condition has similar features to Korsakoff syndrome and is associated with transient ischemia of the mediobasal parts of the temporal and parieto-occipital lobes of the brain [13].
Clinical manifestations of ICVS have age-related characteristics. In elderly and senile age, multiplicity and recurrence of acute episodes of acute ischemia in the VBS are often observed. Clinically, this is manifested by attacks of dizziness, nystagmus, balance and coordination disorders. The results of the study [22] convincingly prove that vertebrobasilar insufficiency is a relatively rare cause of dizziness in the elderly. In 17.1% of cases, dizziness is caused by a reversible disorder of cerebral circulation in the VBS and damage to the central vestibular structures, and only in 5.7% of patients it is a consequence of an acute cerebrovascular accident, which was confirmed by neuroimaging studies and vestibulometry. In 8 (11.4%) patients, postural disorders were caused by chronic cerebrovascular insufficiency. This is due to the fact that in old age it is difficult to identify a single leading cause for the development of ICVS. As a rule, they are multiple - hypercholesterolemia, tortuosity of one or both VAs, atherosclerotic stenosis of the internal carotid arteries, the presence of degenerative changes in the spine [10].
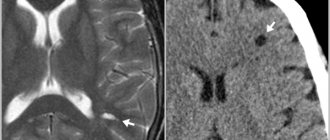
An important manifestation of chronic cerebral ischemia is a change in the white matter (leukoaraiosis) of the deep parts of the brain. In elderly patients, a relationship has been recorded between the prevalence of leukoaraiosis, especially in the anterior parts of the brain, the localization of lacunar lesions in the lenticular nucleus and the severity of walking and balance disorders, and cognitive impairment (CD) [29]. Correct diagnosis of ICVS in patients with CR can be difficult [31]. After a stroke, 25-30% of patients develop dementia within a year. Up to 30-70% of patients who have suffered a stroke suffer from moderate CR, which makes it difficult to collect anamnesis and correct interpretation of complaints.
Diagnosis and differential diagnosis of ICVS
Diagnosing ICVS is not an easy task. On the one hand, dizziness in various diseases can occur in exactly the same way, on the other hand, it can have a different clinical picture for one type of pathology. For example, in outpatients with dizziness, the cause of the disease is identified only in 20% of cases [7]. When making a diagnosis, it is necessary to conduct a thorough examination of the patient, including a detailed history taking and analysis of complaints. It is important to measure blood pressure in the supine and standing positions - with a significant decrease in systolic pressure (more than 20 mm Hg) in an upright position, accompanied by symptoms, clinical manifestations similar to vertebrobasilar insufficiency should be considered as a consequence of orthostatic hypotension. During a neurological examination, attention should be paid to the presence or absence of nystagmus, static or dynamic ataxia. The results of the Romberg tests (the patient, standing with his eyes closed, deviates towards the labyrinth lesion) and Babinsky-Weil tests (the patient with his eyes closed takes five steps forward and back several times - with a unilateral vestibular lesion, his route will be shaped like a star) are of significant value. In elderly patients and patients who abuse alcohol, toxic substances, and drugs, it is necessary to conduct neuropsychological testing to identify CR. The diagnostic algorithm also includes an otoneurological examination, including computer electronystagmography (CENG), audiometry, and recording of auditory evoked potentials (AEP). If a spondylogenic effect on the VA is suspected, an X-ray or MRI of the cervical spine and duplex scanning of the VA are performed. Differential diagnosis of ICVS should be carried out taking into account the characteristic features of Meniere's disease, demyelinating diseases of the central nervous system, and tumors of the cerebellopontine angle.
An attack of Meniere's disease is similar to an attack during ICVS, but is much shorter in duration, and the course of the disease is recurrent. It is characteristic that a sudden attack of intense systemic dizziness in combination with nausea and vomiting, spontaneous nystagmus, and unilateral hearing loss is completely relieved within 1-3 hours. During the examination, there are no other neurological symptoms.
Patients with multiple sclerosis may experience dizziness and other symptoms characteristic of ICS. The disease is relapsing in nature and is characterized by a combination of vestibular and cerebellar disorders with signs of damage to other parts of the central nervous system, and the presence of foci of demyelination of the white matter on MRI of the brain. Tumors of the cerebellopontine angle are characterized by hearing impairment (one-sided sharp hearing loss), phenomena of vestibular dysfunction in the absence of dizziness, and signs of damage to nearby cranial nerves.
Principles of therapy
Although many patients with dizziness can be effectively treated, treatment is often inadequate [12]. There is no doubt that treatment of patients with ICVS, first of all, should be aimed at eliminating the cause that caused them, but the causes cannot always be identified and easily eliminated. In this regard, symptomatic treatment is essential. Currently offered drugs for the treatment of patients with ICVS belong to different pharmacological groups and have different efficacy and tolerability. There is still no clear picture in understanding the mechanisms of the vestibulolytic action of the most widely used drugs.
The main goals of therapy are to prevent the onset or progression of the pathological process, improve cognitive functions and general therapeutic measures [27, 28]. The main issue in medical practice is the search for the “ideal” drug or complex of drugs and compliance with the requirements for their use. ICVS therapy should be comprehensive and include drugs with a multi-vector mechanism of action. To prevent secondary ischemic disorders, it is necessary to prescribe antiplatelet agents (acetylsalicylic acid, ticlopidine), and if symptoms increase, anticoagulants [20]. Treatment of systemic dizziness is largely determined by its cause; in addition, symptomatic therapy plays an important role [30]. A clear distinction should be made between so-called immediate and long-term therapy [21].
Early administration and long-term use of vestibulolytic drugs is necessary. For example, betahistine dihydrochloride preparations, which act on histamine H1 and H3 receptors and improve microcirculation in the labyrinth and neurotransmission in the area of the vestibular nuclei of the central nervous system [4]. Betahistine is a drug that promotes the accumulation and release of histamine in neuronal synapses of the central and peripheral nervous system, but does not have the side effects of histamine. At the periphery, this drug increases microcirculation in the inner ear and improves cochlear blood flow. Under the influence of betahistine, central histamine receptors are able to compensate and accelerate vestibular adaptation. The drug has a prohistamine effect on the postsynaptic membrane, predominantly affecting H3 receptors located on the presynaptic membrane. Dizziness is blocked due to the agonistic effects of the drug on central and peripheral H1 receptors. However, betahistine does not affect the H2 receptors of the gastrointestinal tract. The use of this drug does not provide a quick clinical effect; it requires compliance with the dosage regimen (daily dose 48 mg) and long-term use (at least 1 month).
“First aid” therapy for ICVS should be carried out with drugs that have vasoactive, neuroprotective and metabolic properties (Cavinton, Vasobral, Piracetam, Mexicor). It is extremely important that this therapy is aimed at correcting local pathophysiological mechanisms - impaired tone of cerebral arteries and veins, metabolic processes in the brain, hemorheology and microcirculation [32]. The clinical effect of these drugs is usually achieved within 10-14 days. The duration of the course of treatment and the choice of drug are determined by the doctor individually. Due to a decrease in the tone of the cerebral veins and disturbances of venous outflow, venotonics (troxevasin, tanakan) are successfully used. Due to the fact that oxidative stress plays a special role in the clinical and morphological picture of ischemia, drugs with neurometabolic effects are used that improve the survival of neurons under conditions of chronic hypoxia. Some of them have antioxidant properties.
One of the most well-known, thoroughly studied drugs in this area is ethyl apovincamine (Cavinton, JSC Gedeon Richter) [8]. Cavinton is an ethyl ester of apovincamine acid, a synthetic derivative of vincamine, a natural alkaloid of Vinca minor. The mechanism of action of the drug consists of inhibition of phosphodiesterase (Ca/calmodulin-dependent type 1), leading to an increase in the level of cAMP and cGMP and inhibition of voltage-dependent Na+ channels - protection against excessive neuronal activation. Cavinton has a direct effect on glutamate receptors, inhibits lipid peroxidation due to the normalization of cellular processes, captures adenosine, causes vasodilation, increases the intracellular level of cGMP in the smooth muscles of the vascular wall, and in terms of the severity of this effect it significantly exceeds all vasodilators, inhibits platelet aggregation, increases deformation of red blood cells. The combination of a pronounced decrease in the resistance of the cerebral arteries and an almost stable level of systemic pressure allows us to regard the vasodilating effect of Cavinton as selective in relation to the cerebral arteries. In patients with persistently elevated levels of systemic blood pressure, the use of Cavinton is accompanied by a moderate hypotensive effect (pressure decreases by 10-15 mmHg).
At the same time, it was found that intravenous administration of the drug in patients with initially normal or even low blood pressure was accompanied by a very moderate increase (by no more than 20/10 mmHg). It has a normalizing effect on cerebral vessels with both increased and decreased tone, preventing, in particular, inadequate vascular reactions. The drug restores the ability to autoregulate cerebral circulation, prevents the development of vasoconstrictor changes that cause the “no-reflow” phenomenon in the early post-ischemic period. The drug prevents the loss of neurons in the hippocampus by 40%, has a pronounced membrane-stabilizing effect, stimulates the noradrenergic system of the ascending reticular formation, and is involved in the modulation of plasticity (increases the growth of dendritic spines). The therapeutic effect when using Cavinton is observed from the first day of treatment. Its severity increases as the drug is taken. Delayed effects persist for 1 year after the end of therapy. Course therapy with Cavinton improves the general clinical condition of patients with ICVS, their mental and physical performance. Therapy with new forms of Cavinton (25 mg/5 ml and 50 mg/10 ml) and Cavinton Forte (10 mg No. 90) according to a new regimen significantly reduces subjective manifestations of cerebrovascular diseases: headache by 82%, dizziness by 75%, tinnitus by 46%. The most pronounced positive dynamics were revealed in regression of oculomotor disorders, nystagmus, vestibulo-ataxic and amyostatic syndromes [8]. Improvement in cognitive functions during treatment with Cavinton is caused by its corrective effect on various parts of chronic cerebral hypoperfusion. The effectiveness and safety of long-term use of the drug (1-2 years) is confirmed by studies conducted in Hungary, Germany, Italy and Japan (evidence category B). The drug is used in a daily dose of 25-50 mg intravenously (drip) for 7-10 days, followed by switching to oral administration of the drug Cavinton Forte 10 mg 3 times a day for 1-3 months.
Understanding the mechanism of action of drugs on the body expands the range of possibilities for drug therapy for TCVS. The effectiveness of the drug is determined from the standpoint of evidence-based medicine and is expressed in reducing the clinical manifestations of the disease and improving the patient’s quality of life. A special place is occupied by the safety of medicines. The final conclusion about the ineffectiveness of the chosen treatment and the need for its correction can be made in the absence of a therapeutic effect after 2-3 courses lasting at least 3 months. You should not refuse the chosen drug unless its dose has been increased to an individual maximum and well tolerated. If the drug is insufficiently effective but is well tolerated, a second drug from a different class can be added to it. Modern knowledge makes it possible to combine two or more drugs. The most optimal combination is a combination of a vertilolytic drug (betahistine) + a neuroprotector (Cavinton) + an energy corrector (Actovegin). This combination can provide a more pronounced therapeutic effect with a lower likelihood of side effects, because lower doses are used. However, the following rule must be observed: early initiation and long-term continuation (up to 3-4 months) of therapy.
Thus, ICVS, having different etiopathogenetic mechanisms, requires careful diagnosis, early complex drug therapy and subsequent neurorehabilitation.
2. Reasons
Cochlear neuritis can develop under the influence of many factors:
- infectious diseases (flu, measles, ARVI, herpes, scarlet fever, etc.);
- intoxication with salts of heavy metals, industrial hydrocarbons, drugs (antibiotics, chemotherapy, antiarrhythmics, diuretics, etc.);
- industrial hazards (vibration, noise);
- acute and chronic conditions associated with cerebrovascular disorders (blood supply to the brain);
- traumatic brain, acoustic, radiation, birth injuries;
- cancer;
- neurodegenerative processes and age-related changes.
As can be seen from the above, in most cases, cochlear neuritis is acquired. However, there is also congenital sensorineural hearing loss, which is usually caused by hereditary factors and is one of the elements of one or another chromosomal syndrome.
Visit our Otolaryngology (ENT) page
Diagnostics
Diagnosis of vertebral artery syndrome presents certain difficulties and both overdiagnosis and underdiagnosis of vertebral artery syndrome often occur. Overdiagnosis of the syndrome is often due to insufficient examination of patients, especially in the presence of vestibulo-atactic and/or cochlear syndrome, when the doctor fails to diagnose diseases of the labyrinth.
To establish a diagnosis of vertebral artery syndrome, 3 criteria must be present.
- The presence in the clinic of symptoms of one of 9 clinical options or a combination of options
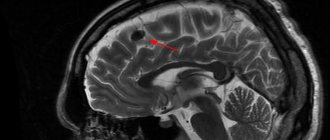
- Visualization of morphological changes in the cervical spine using MRI or MSCT, which may be the main reasons for the development of this syndrome.
- The presence of changes in blood flow during ultrasound examination when performing functional tests with flexion - extension of the head and rotation of the head.
3. Symptoms and diagnosis
The most typical manifestations of cochlear neuritis, in addition to hearing loss itself, are sensations of constant extraneous noise in the head and asymmetrical hearing loss. Some patients also experience a complex of vestibular disorders (dizziness, coordination and balance disorders, unsteadiness of gait, etc.).
Obviously, any hearing loss, incl. caused by cochlear neuritis, is a socially significant problem, since it leads to disruptions in communication and social functioning, requires the use of hearing aids, in many cases limits or excludes professional suitability, and provokes the development of psychological disorders of the depressive register.
The degree of functional failure of the auditory analyzer is established in a series of audiometric, tuning fork and other similar tests. Otoscopy and microotoscopy are performed; Electrocochleagraphy, vestibulometric studies, consultations (and corresponding examinations) of specialized specialists, and a battery of laboratory tests are also prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms
According to the clinical course, two stages of vertebral artery syndrome are distinguished: functional and organic.
The functional stage of vertebral artery syndrome is characterized by a certain group of symptoms: headaches with some autonomic disorders, cochleovestibular and visual disturbances. Headache can have various forms, both acute throbbing and constant aching or sharply intensifying especially when turning the head or prolonged static load. The headache may spread from the back of the head to the forehead. Disturbances in the cochleovestibular system can manifest as paroxysmal dizziness (swaying instability) or systemic dizziness. In addition, some hearing loss may occur. Visual disturbances can manifest as darkening of the eyes, a feeling of sparks, sand in the eyes.
Prolonged and prolonged episodes of vascular disorders lead to the formation of persistent foci of ischemia in the brain and the development of the second (organic) stage of vertebral artery syndrome . In the organic stage of the syndrome, symptoms of both transient and persistent hemodynamic disorders of the brain appear. Transient hemodynamic disturbances are manifested by symptoms such as dizziness, nausea, vomiting, and dysarthria. In addition, there are characteristic forms of ischemic attacks that occur during turning or tilting the head, during which attacks of falling with preserved consciousness may occur, so-called drop attacks, as well as attacks with loss of consciousness lasting up to 10 minutes (syncope episodes). Symptoms usually regress in a horizontal position and are thought to be due to transient ischemia of the brainstem. After such episodes, general weakness, tinnitus, and autonomic disturbances may occur.
Based on the type of hemodynamic disturbances, several variants of vertebral artery syndrome are distinguished (compressive, irritative, angiospatic and mixed forms).
Vessel narrowing in the compression variant occurs due to mechanical compression on the artery wall. In the irritative type, the syndrome develops as a result of reflex spasms of the vessel due to irritation of sympathetic fibers. In the clinic, most often, combined (compression-irritative) variants of vertebral artery syndrome are encountered. In the angiospastic variant of the syndrome, there is also a reflex mechanism, but it arises from irritation of receptors in the area of the motor segments of the cervical spine. In the angiospastic variant, vegetative-vascular disorders predominate and the symptoms are not so strongly associated with head turns.
4.Treatment
Effective etiotropic therapy is possible only in cases where the causes of nerve damage are identified and when these causes are reversible. In different situations, neurological, antibiotic, antiviral, and physiotherapeutic treatment is prescribed (the role and possibilities of the latter are very large and have not been sufficiently studied to date). In some cases, hearing is restored after surgery, which eliminates, for example, the factor of mechanical pressure on the nerve.
According to data published today, significant improvement or complete restoration of hearing function can be achieved in approximately 80% of cases. If all measures taken are ineffective, a hearing aid is selected; The characteristics and design of modern high-tech digital models can radically reduce the psychological, social and professional limitations caused by hearing loss.