Acute disseminated encephalomyelitis is a single-phase autoimmune demyelinating disease in which the pathological process is localized in the central nervous system. Damage to the brain or spinal cord can occur after an infectious disease or vaccination. The reasons for the development of the idiopathic form of the disease are unknown. Rarely do neurologists diagnose recurrent or multiphasic acute disseminated encephalomyelitis.
The Yusupov Hospital has created optimal conditions for the successful recovery of patients:
- examination using the latest diagnostic equipment from leading global manufacturers;
- treatment with effective pharmacological drugs that have a minimal range of side effects;
- the use of innovative methods of restorative therapy by rehabilitation clinic specialists.
Severe cases of the disease are discussed at a meeting of the expert council with the participation of doctors and candidates of medical sciences, leading experts in the field of demyelinating diseases of the central nervous system. Doctors at the neurology clinic, who have extensive experience in treating acute disseminated encephalomyelitis, treat the patient according to an individual plan. At the same time, they comply with the recommendations of domestic and international neurological communities.
Causes and consequences
The main reason for the development of acute disseminated encephalomyelitis is the patient’s autoimmune response to myelin or other antigens, which is accompanied by an inflammatory process in the brain or spinal cord, or involving both the spinal cord and the brain. Most often, the disease debuts in childhood. This is due to the characteristics of the immune system. When adequate therapy is started in a timely manner, the disease responds well to treatment.
Today, scientists are studying the mechanism of development of autoimmune reactions. In acute disseminated encephalomyelitis, cells of the immune system begin to perceive myelin as a foreign element and attack it. Why the immune system behaves this way is unknown. Typically, the pathological process is triggered as a result of exposure to viruses and bacteria that infect the upper respiratory tract when body temperature rises above 380C.
The following factors are known to provoke the onset of acute disseminated encephalomyelitis: herpes virus, measles, chickenpox, Epstein-Barr, mumps, rubella. Rarely, the disease develops after vaccination with live, weakened bacteria or viruses, when the immune system reacts inadequately.
Acute disseminated encephalomyelitis usually occurs without negative consequences. Sometimes residual brain lesions persist for life. In this case, a relapse of the disease or multiple sclerosis in the future may develop.
After acute disseminated encephalomyelitis, vision may decrease and sensitivity may be impaired. In severe cases of the disease, consciousness is impaired in patients. In rare cases, death occurs due to cerebral edema.
ADEM: acute disseminated disseminated encephalomyelitis
Acute disseminated disseminated encephalomyelitis (ADEM) is a neurological disease of an autoimmune nature, which is characterized by the development of demyelination processes in the spinal cord and brain. The disease occurs as a result of an acute inflammatory or infectious process in the body. ADEM is a rare neurological pathology. It develops more often in children, since the children's immune system is not yet able to adequately resist viruses and infections.
Causes
The development of acute disseminated disseminated encephalomyelitis is preceded by a viral or infectious disease, which is accompanied by an increase in body temperature above 38°C. Sometimes ADEM occurs as a result of exanthemal diseases: measles, chicken pox, rubella and others. The development of neurological disorders occurs one or several weeks after the first episode of fever.
With ADEM, an intense inflammatory process occurs in the brain. As a result, the destruction of myelin, the sheath of nerve fibers, begins. In the initial stages, ADEM is often mistaken for multiple sclerosis, since these neurological diseases have similar symptoms. Modern methods of laboratory and instrumental research allow identifying ADEM.
ADEM can occur when the body is infected with the following viruses:
- Herpes;
- Mumps;
- Epstein-Barr;
- Cytomegalovirus.
In rare cases, ADEM develops after vaccination. The use of active pathogens in a vaccine can provoke an abnormal response of the immune system, leading to autoimmune disorders.
Course of the pathological process
As a result of an autoimmune reaction, diffuse demyelination occurs and an inflammatory process develops in the Virchow-Robin space, the function of which is to regulate the production of cerebrospinal fluid and the exchange of substances between the cerebrospinal fluid and tissue fluid. The infectious agent enters the body through the upper respiratory tract or digestive organs. The infectious agent enters the spinal cord through the blood or perineural route. In acute disseminated encephalomelitis, the peripheral nervous system suffers less; the white matter of the brain is more affected.
The disease begins with a rise in temperature to 38°C - 39°C, nausea, vomiting, muscle pain and headache. Patients show signs of brain damage:
- convulsions;
- ataxia (impaired coordination of movements of various muscles in the absence of muscle weakness);
- partial blindness;
- strabismus;
- disturbance or loss of consciousness;
- epileptic seizures,
- speech disorders;
- swallowing disorder;
- hallucinations;
- drowsiness;
- breathing disorder.
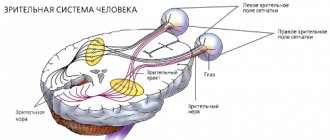
After peripheral nerves and spinal roots are involved in the pathological process, the patient develops pain, paresthesia (a crawling sensation), the pulse quickens, and the function of the pelvic organs is disrupted. The skin becomes pale. When the optic nerve is damaged, double vision occurs, white spots appear before the eyes, and difficulty focusing occurs.
In cases of severe brain damage, the disease progresses rapidly and death occurs within a few days. In the chronic course of the disease, improvement is replaced by exacerbation of the infectious process. In this case, difficulties arise with the differential diagnosis of the disease in a patient with multiple sclerosis.
The symptoms of acute disseminated encephalomyelitis increase rapidly, so specialized medical care should be sought at the first signs of damage to the nervous system. The Yusupov Hospital employs experienced neurologists who use the latest equipment, allowing them to perform diagnostics of any complexity and in the shortest possible time. This is especially important for establishing a final diagnosis when choosing the optimal treatment strategy for acute disseminated encephalomyelitis. The earlier therapy is started, the greater the chance that there will be no residual effects after treatment.
Make an appointment
Classification
It is customary to distinguish acute disseminated encephalomyelitis - ADEM (in English literature known as ADEM - acute disseminated encephalomyelitis). There are 3 types of WECM:
- post-infectious;
- post-vaccination;
- spontaneous.
It is also customary to distinguish between primary (idiopathic) and secondary encephalomyelitis.
Classification by stream:
- Acute encephalomyelitis. Characterized by lightning-fast, rapid development and increase in neurological symptoms. It appears against the background or immediately after an infectious disease. Patients complain of cough, muscle pain, fever, chills, and shortness of breath.
- Subacute encephalomyelitis . The rate of development of symptoms is slower than in the acute form.
- Chronic encephalomyelitis . Characterized not only by the slow development of clinical symptoms, but also by episodes of relapse, which makes this form similar to multiple sclerosis . Exacerbation of the disease occurs very often (5-33% of cases). Multiphase cases account for 20% of the incidence, and recurrent forms account for 80%. Multiphase forms are characterized by periods of exacerbation after the apparent completion of the acute process and transition to the stage of residual manifestations. Recurrent cases are characterized by increased neurological symptoms during treatment in the first 3 months of the disease.
Variants of acute disseminated encephalomyelitis depending on clinical manifestations:
- diffuse encephalomyelitis;
- encephalomyelopolyradiculoneuritis;
- myelopolyneuritis;
- optoencephalitis.
There is also myalgic encephalomyelitis , a benign chronic fatigue syndrome. The pathology is characterized by long-term (at least 6 months), excessive, disabling fatigue and is accompanied by numerous infectious, articular and neuropsychic symptoms.
The diagnosis of “myalgic encephalomyelitis” is established if the patient has at least 4 of the 8 listed symptoms for 6 months:
- impaired concentration and memory;
- joint pain (without swelling or redness);
- pain on palpation of the axillary and cervical lymph nodes;
- pharyngitis;
- lack of feeling of vigor and freshness after sleep;
- muscle stiffness and soreness;
- headache;
- feeling of fatigue and exhaustion after mental or physical labor, lasting for 24 hours or more.
Diagnostics
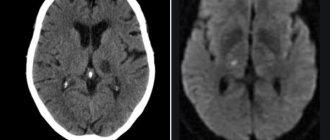
Magnetic resonance imaging helps to establish an accurate diagnosis if a patient is suspected of having acute disseminated encephalomyelitis. On MRI, radiologists detect multifocal lesions in the white matter of the brain (pons, cerebellum, hemispheres). Foci of damage to the gray matter can also be identified (in the thalamus, hypothalamus, basal ganglia). They are absent from the corpus callosum.
MRI reveals large lesions, which are accompanied by perifocal edema. In other cases there are no changes. With timely treatment of acute disseminated encephalomyelitis, after several weeks of adequate therapy, inflammatory changes in individual areas of the brain disappear.
In patients suffering from acute disseminated meningoencephalomyelitis, new lesions do not appear. If a doctor detects new areas of demyelination on an MRI, this indicates multiple sclerosis. In order to establish an accurate diagnosis, neurologists perform a spinal puncture and send cerebrospinal fluid for laboratory testing.
Symptoms
Damage to the nervous system occurs a couple of weeks after the onset of the infectious disease with an increase in body temperature. The most common trigger for ADEM is viral infections of the upper respiratory tract. The clinical course of the disease includes frequent attacks of fever, headaches, chills, and numbness of the extremities.
One or several weeks after the first episode of fever, neurological symptoms of ADEM appear:
- Confusion;
- Loss of coordination;
- Speech disorders;
- Difficulty swallowing;
- Double vision;
- Weakness in the arms and legs;
- Breathing disorder;
- Impaired consciousness up to coma.
ADEM is characterized by a rapid increase in symptoms. Changes in the brain begin to occur, which give rise to a diagnosis.
Diagnostics
Correct and timely diagnosis is the key to successful recovery of the patient. An experienced neurologist will suspect the development of ADEM based on the clinical picture. To accurately determine the disease, doctors at the Yusupov Hospital prescribe laboratory tests and magnetic resonance imaging (MRI). Cerebrospinal fluid analysis will show increased protein content and lymphocytic pleocytosis. The blood test will show moderate leukocytosis and increased erythrocyte sedimentation rate.
MRI is a key factor in diagnosing ADEM. An MRI will show multiple abnormalities in the structure of the white matter of the brain. White matter is the nerve fibers that suffer in acute disseminated disseminated encephalomyelitis. They are covered with a myelin sheath, which is destroyed by the immune system. ADEM lesions can spread over large areas of white matter. With adequate and timely treatment, these changes gradually disappear.
Treatment
Neurologists at the Yusupov Hospital provide complex therapy for ADEM with the following drugs:
- Corticosteroids;
- Immunoglobulins;
- Nootropics;
- Amino acids;
- Vitamins.
The drugs are aimed at accelerating the healing process, relieving symptoms and restoring metabolic processes in the brain. Glucocorticosteroids are prescribed in high doses for 5-7 days. For maintenance therapy, measures to reduce body temperature, drugs to eliminate seizures and reduce intracranial pressure are used. The body is detoxified using plasmapheresis.
Treatment
Neurologists at the Yusupov Hospital provide complex therapy for acute disseminated meningomyelitis. To suppress the abnormal immune response, glucocorticoid hormones are administered intravenously for 3-5 days. If there is no result from pulse therapy with corticosteroids, doctors in the intensive care unit perform 4-5 sessions of plasmapheresis.
If the inflammatory process is caused by bacteria, patients are prescribed antibiotics. If the viral nature is established, a-interferon preparations or interferonogens are used. High fever is reduced with antipyretics. To improve metabolic processes in the cerebral cortex, patients are prescribed nootropic drugs. Medicines that reduce intracranial pressure and normalize blood supply to the brain are also used. Neurologists provide maintenance therapy with vitamin and mineral complexes and amino acid mixtures.
Rehabilitation clinic specialists provide a course of non-drug therapy to restore cognitive and social functions. Rehabilitators use modern effective methods of physical therapy, various types of massage, physiotherapeutic procedures, and acupuncture. If indicated, the patient can consult a psychiatrist.
Consequences
ADEM is a rare disease. Most often it is recorded in childhood, which is associated with the characteristics of the immune system. The disease responds well to treatment if therapy is started in a timely manner. Acute disseminated encephalomyelitis can be cured with medication and in most cases the disease leaves no consequences.
Sometimes residual lesions of the brain persist for life, which threatens relapse of the disease or the development of multiple sclerosis in the future. After acute disseminated encephalomyelitis, decreased vision and sensory disturbances may occur. In severely advanced cases of the disease, significant disturbances of consciousness occur. In rare cases, death occurs due to cerebral edema.
In order to make an appointment with a neurologist at the Yusupov Hospital, call the contact center phone number at any time of the day, regardless of the day of the week.
Make an appointment
Affected Populations
ADEM can develop at any age, but it is much more common in children than in adults. Men and women are affected in equal numbers, although a slight male predominance was noted in paired pediatric studies. In children, the disease is diagnosed on average at the age of 5-8 years. The exact incidence of ADEM among the Russian population as a whole is unknown. The disease appears to peak during the winter and spring months in studies conducted in the United States.