Experts from the World Health Organization believe that a stroke is a rapidly developing total or focal impairment of brain function that lasts more than 24 hours or leads to death. Stroke in women occurs between the ages of 18 and 65. The disease affects the patient’s quality of life and can lead to disability or death. The main reason is that women present with strokes a few days after the onset of the disease, when doctors have to deal with the consequences of the disease, and not with the disease. Neurologists at the Yusupov Hospital quickly diagnose stroke using modern examination methods:
- computer and magnetic resonance imaging;
- Dopplerography of cerebral vessels;
- video electroecephalogram;
- electromyography.
Such methods allow you to quickly determine the signs of stroke in women and apply appropriate treatment.
Symptoms of stroke in women are most often atypical. The patient may accidentally confuse the first sign with a simple malaise or another disease. Signs of a stroke in a woman have the following characteristics:
- age. In women, stroke develops mainly between the ages of 18 and 65;
- type of disease. Most often, women develop a hemorrhagic stroke due to a rupture of a cerebral artery against the background of high blood pressure. This is facilitated by emotional shock, sudden changes in hormonal levels, increased sensitivity to stress;
- hormonal background. Pregnancy, childbirth, taking contraceptives leads to changes in blood clotting and increases the susceptibility to stroke by 20-22%;
- course of the disease. Women are more likely than men to develop stroke complications and have a higher mortality rate. The disease is characterized by a severe course; warning signs of a stroke in a woman occur suddenly;
- ignoring the disease. The first symptoms of a stroke in women do not cause alarm.
Often, the precursors of stroke in women are vegetative-vascular dysfunction and transient cerebrovascular accidents.
Precursors of stroke in women
Stroke occurs more often in women than in men.
Signs of an impending stroke in women:
- limbs move worse or do not move, weakness in the arm and leg on one side;
- weakness, drowsiness, increasing headache, which leads to nausea, lethargy;
- decreased sensation in a limb or one side of the body;
- impaired speech perception and ability to speak;
- loss of balance, ability to navigate in space.
Development and risk groups
The development of a stroke is caused by a sharp increase in blood pressure, physical activity, and emotional stress. In such situations, a vessel ruptures followed by hemorrhage or spasm with ischemia. Predisposing factors are diabetes mellitus, high cholesterol, heart, vascular and blood diseases, and excess weight. In these diseases, blood vessels lose their elasticity and their walls stretch. People who or their close relatives have had a stroke or heart attack should be especially careful.
There are scales that determine the degree of risk of developing a stroke: the Framingham scale for assessing individual risk of developing stroke, the London School of Hygiene questionnaire on cardiovascular diseases by J. Rose.
By undergoing such testing, you can identify the degree of risk, undergo an examination and undergo a course of treatment in a timely manner before your health is affected.
Risk groups are identified:
- by age and gender - the likelihood of a stroke increases after 30 years. Ischemic stroke occurs more often in men aged 50-69 years. The incidence of hemorrhagic stroke up to 60 years of age is the same in men and women, then higher in women;
- in terms of lifestyle - unfavorable factors include inactivity, bad habits, stress, heavy physical labor. These factors worsen health and provoke chronic heart and vascular diseases.
Signs of a stroke
A stroke is localized in the brain or spinal cord.
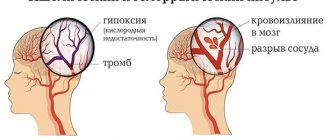
It is divided into ischemic and hemorrhagic. In an ischemic stroke, part of the brain tissue dies due to circulatory failure. The hemorrhagic type occurs when the vessel wall is damaged and blood flows into the brain tissue. It occurs suddenly, more often during the day. It is preceded by a hypertensive crisis.
The first signs of a stroke in women:
- gradually increasing headache;
- weakness;
- speech disorder;
- vomit;
- loss of consciousness, coma;
- pupils of different sizes;
- frequent noisy breathing;
- weakness in the limbs on one side, paralysis in the arm or leg on one side (hemiparesis);
- speech disorder.
The stroke that occurs in older women (after 50-60 years) is in some way different from the one that develops in women 30-35 years old or 40-50 years old.
Difference between stroke in young and old age:
- The course of the stroke.
- Greater aggressiveness, pathology, and rate of damage to brain tissue in women over 70-80 years of age.
- In the consequences after a stroke in elderly women.
- How favorable the prognosis after a stroke can be for women over 60-80 years of age.
- Signs of stroke in young women.
Bibliography
- Hemorrhagic stroke in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021. Developers: Association of Neurosurgeons of Russia. - Electronic text. - URB: (access date 08/18/2020).
- Efremova M.D. Stroke as an urgent socio-psychological problem / M.D. Efremova – electronic text//Skif. Questions of student science.- 2021 - No. 2(24) URB: (date of access 08/17/2021) Access mode: Cyberleninka electronic library system. — Text: electronic.
- Ischemic stroke and transient ischemic attack in adults: clinical recommendations of the Ministry of Health of the Russian Federation, 2021 developers: All-Russian Society of Neurologists, National Association against Stroke, Association of Neurosurgeons of Russia, Association of Neuroanesthesiologists and Neuroreanimatologists, Union of Rehabilitologists of Russia. - Electronic text. - URB: ( access date 08/18/2020).
- Machinsky P.A. Comparative characteristics of incidence rates of ischemic and hemorrhagic stroke in Russia / P.A. Machinsky, N.A. Plotnikova, V.E. Ulyankin [and others] – Direct text.// News of higher educational institutions. Volga region. Medical Sciences.- 2021.- “2(50)-P.112 – 132 DOI 10.21685/2072-3032-2019-2-11.
- Monitoring the implementation of the federal project “Combating Cardiovascular Diseases” - Presentation Department of Organization of Medical Care and Sanatorium Affairs of the Ministry of Health of the Russian Federation URB: (date of access 08/17/2021).
- Order of the Ministry of Health of the Russian Federation dated November 15, 2012 N 928n “On approval of the Procedure for providing medical care to patients with acute cerebrovascular accidents.” — URB: (access date 08/17/2021) Access mode: Electronic library system “Garant”. — Text: electronic.
- Order of the Ministry of Health of the Russian Federation dated July 31, 2021 No. 788n “On approval of the Procedure for organizing medical rehabilitation of adults.” – URB: (date of access 08.17.2021).- Access mode: Electronic library system “Garant”. — Text: electronic.
- Prevention of cerebrovascular accidents: textbook. manual / Compiled by: L.B. Novikova, A.P. Akopyan. – Ufa: Publishing house of the State Budgetary Educational Institution of Higher Professional Education BSMU of the Ministry of Health of Russia, 2015.-58 p.
- Stakhovskaya L.V. Analysis of epidemiological indicators of recurrent strokes in the regions of the Russian Federation (based on the results of the territorial-population register 2009-2014) / L.V. Stakhovskaya, O.A. Klochikhina, M.D., Bogatyreva, etc.]. CONSILIUM MEDICUM, 2021, vol. 5, no. 9, p. 8-11.
- Shamalov N. A. Analysis of the dynamics of the main types of stroke and pathogenetic variants of ischemic stroke / N. A Shamalov, L. V Stakhovskaya, O. A Klochikhina [and others]. Direct text. // Journal of Neurology and Psychiatry named after. S.S. Korsakov. Special issues. 2019;119(3-2):5-10. doi.org/10.17116/jnevro20191190325.
- 1RRE Electronic edition. Updated daily Stroke Day is celebrated on October 29, 2021 URB: (accessed 08/17/2021).
Author:
Pugonina Tatyana Alekseevna, Therapist
First aid for stroke
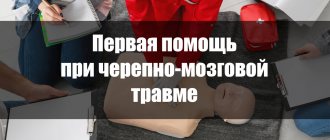
It is impossible to determine the nature of a stroke in the first hours, therefore it is necessary to normalize vital functions (breathing, blood circulation) and ensure the prevention of possible complications (pneumonia, thromboembolism, bedsores).
The first step is to call an ambulance. It is advisable to reassure the patient and measure blood pressure. If there is vomiting, place the patient on his side and place his hand under his head. Do not bend your neck, because blood flow cannot be impaired. The airways need to be clear. In case of severe respiratory distress, mechanical ventilation must be started.
If breathing is impaired, it is necessary to free the patient from tight clothing. Free the oral cavity from foreign objects, mucus, and vomit. If the patient is indoors, access to fresh air is necessary. If a person is conscious, it is advisable to cheer him up and calm him down.
If you lose consciousness, you need to make sure that the person is not injured or bruised.
There is no need to take medications so as not to worsen the patient’s condition.
If it is not possible to call an ambulance, then you must transport the victim to the hospital yourself.
How to determine the onset of a stroke
It is impossible to distinguish a transient ischemic attack from an irreversible acute circulatory disorder without medical assistance. Both situations require hospitalization. Serious attacks can be identified using a simple test:
- The patient needs to symmetrically extend both arms forward, then alternately touch his nose with each palm. The inability to do this, sudden disturbances in the trajectory of movements, and a distorted body are signs of an attack.
- When looking in the mirror or at your interlocutor, you should smile broadly, stick out your tongue far, and say a few words. A possible stroke is indicated by distorted or paralyzed corners of the mouth, deviation of the tongue to the side, and slurred speech.
- You must try to write on paper or type any text on the keyboard. During a stroke, this is very difficult to do; the result is a meaningless set of letters.
One or more alarming symptoms is a reason to urgently call for medical help or go to the hospital. The first 3 hours after a stroke are most important for restoring blood circulation and preventing irreversible brain damage. A doctor is also necessary in cases where health has recovered on its own.
The relationship between brain regions and the clinical picture of stroke
If the right lobe is affected, this is expressed by paralysis of the left limbs or loss of sensitivity in them.
The patient has a pronounced depressive state and a decrease in the desire for recovery. If the hippocampus area is affected, then the patient cannot grasp objects with his hand, loses the ability to navigate in space, cannot remember what happened yesterday, but memories of a longer period are preserved.
The hippocampus is responsible for emotions, short-term and long-term, spatial memory necessary for orientation in space.
If the left lobe is affected, then paralysis, decreased or loss of sensitivity in the right half of the body is characteristic, the patient does not perceive speech and speaks inarticulately.
If the cerebellum is affected, there is a lack of coordination, the patient feels nausea and dizziness. When the stem structures are damaged, the patient may experience double vision, the act of swallowing is disrupted, and involuntary movements occur.
Kinds
The main classification of strokes (according to ICD-10) takes into account the cause and mechanism of stroke.
- An ischemic stroke is characterized by a cessation of blood flow to the brain tissue. The reason is a violation of blood flow, blockage of an artery with a blood clot and/or narrowing by an atherosclerotic plaque (atherothrombotic), vasospasm, and a decrease in pressure. Most often develops at the age of 50-69 years. The incidence is 64-75% among all types of stroke.
- Hemorrhagic stroke is a hemorrhage into the substance of the brain or under the arachnoid membrane due to rupture of a vessel as a result of high blood pressure, atherosclerosis, vasculitis, aneurysms, coagulation disorders. Patients aged 50-69 years are at high risk. At 39-49 years old it is less common. The incidence is 15-20% among all types of stroke.
There are classifications that distinguish types of stroke taking into account other signs.
1. By severity:
- minor, including microstroke (transient ischemic attack) - a passing disturbance of cerebral circulation with complete disappearance of neurological symptoms within 1 day to 3 weeks;
- moderate severity;
- severe, extensive stroke of the brain - damage to a large area with pronounced neurological symptoms and severe condition, sometimes with falling into a deep coma.
2. By location
- left or right hemisphere. Each side is responsible for different functions, so the symptoms will be different. For example, if the left half is affected, the movements of the right side of the body suffer, speech and memory are impaired. The person loses the ability to read and write.
When the right hemisphere is damaged, the movement of the left side of the body, the perception of oneself, one’s body, and the surrounding space are impaired, and mental disorders develop.
3. By quantity
- primary stroke (first) and repeated strokes (second, third, fourth). Repeated strokes are more severe because the lesion area increases each time.
4. By age
- in children, starting from the prenatal period, young, elderly. The severity of clinical manifestations and prognosis depend on the patient’s age, the cause of concomitant pathology, and the timeliness of diagnosis. The most difficult prognosis is for delayed detection of a stroke, a large lesion, a weakened body due to concomitant diseases, bad habits, and vitamin deficiency.
5. By localization
:
- in the vertebrobasilar basin with damage to the occipital lobe of the brain, cerebellum and brainstem - visual disturbances develop, gait changes;
- frontal lobes - speech and swallowing suffer;
- temporal lobes - memory, writing, speech deteriorate;
- parietal lobe - speech and speech understanding suffer.
Parietal lobe
Responsible for tactile sensitivity and some other functions.
- Inability to recognize objects blindly.
- Physical hallucinations. They manifest as unpleasant sensations under the skin. The patient complains of movements and swarming.
This is the result of false signals from the brain to the nerve endings along the reflex arc. Hence the itching, burning, desire to scratch the suspected location of discomfort.
Something similar is observed in mental illnesses; it is necessary to distinguish the conditions from each other.
The main differential feature is complete criticism of one’s own position. These are the so-called senestopathy.
Another option is apparent touches from the outside, which in reality are not there. Tactile sensations are false.
Possibly inverted state. The patient does not pay attention to individual parts of her own body and does not recognize them as her own.
- Complex clouding of consciousness. Oneiroids. All senses are involved, the patient is completely at the mercy of the illusory world that her consciousness creates. Duration - from a couple of minutes to several hours. The critical state ends with apathy and a depressive mood under the influence of negative false images.
- Lack of purposeful mental activity. The victim cannot perform simple arithmetic operations and lacks the ability to read and write.
Occipital lobe
The functions of this part of the nervous system include color recognition and normal vision. Processing incoming visual information and converting it into understandable images.
- Complete blindness. Temporary or so-called transient. The disorder has no connection directly with the retina or the visual tract up to the brain.
- Inability to estimate the distance to an object. Understand its dimensions. Metamorphopsia occurs. Small objects appear larger than the patient herself and vice versa. The small room seems like a huge hall.
This is a direct indication of the neurogenic origin of the disorder, because the eye is not able to independently process information. This is just a source, an input for images; the processes of transformation and analysis take place in the cerebral cortex.
- Induced color blindness. Inability to recognize colors.
- Scotomas. Loss of areas of the visual field. They look like black spots that block your view. In the paracentral areas and along the periphery, usually from the side of the temples.
- The simplest visual disturbances. Photopsias. Flashes of light, bright dots, lines. Rings, geometric shapes. There is no objective source of irritation. The central nervous system is excited spontaneously. Restoring blood flow leads to compensation of the condition.
How to avoid getting sick?
Neurologists admit that it is better to prevent a stroke than to treat it. Restoring lost functions of the human brain is extremely difficult. How to avoid a stroke?
- Monitor your blood pressure. Since the most common cause of apoplexy is high blood pressure, doctors urge to fight it. It is important to monitor him and take all necessary medications.
- Quit alcohol and smoking. By quitting smoking, even the most heavy smokers reduce the risk of cerebral hemorrhage by 4 times.
- Eat a balanced diet and avoid foods rich in cholesterol.
- Fight excess weight.
- Increase physical activity.
- Monitor your emotional health.
- Do not overdo it with the uncontrolled use of hormonal drugs, both contraceptives and during menopause.
If it was not possible to avoid a dangerous disease, then only intensive therapy in the next 2-3 hours can increase the chances of a favorable outcome.
Prevention
- Primary prevention consists of proper nutrition, exercise, giving up bad habits and stress, adequate sleep and rest, and regular medical examinations.
- Secondary prevention of stroke includes the elimination of risk factors - treatment of concomitant pathologies, regular monitoring by the attending physician, elimination of risk factors. This approach will help not only prevent stroke, but also improve overall health. According to WHO estimates, the creation of an adequate system of care for patients with stroke will make it possible in the coming years to reduce mortality during the 1st month of the disease by 20% and ensure independence in everyday life 3 months after its onset in at least 70% of patients.