1.What is Devic's syndrome (opticomyelitis)
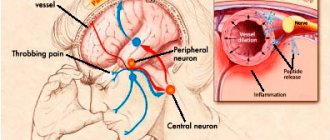
Devic's syndrome is a special form of multiple sclerosis, characterized by a rapid course and severe symptoms. Pathogenetically, neuromyelitis optica belongs to the group of autoimmune diseases. The neurological manifestations of Devic's syndrome are caused by a combination of optic neuritis and damage to the protective fat-like membrane of the spinal cord (transverse myelitis). Developing symptoms affect vision, motor functions, as well as processes regulated by the autonomic nervous system.
Devic's syndrome predominantly develops in old age, and women are more often affected. Foci of transverse myelitis are usually localized at the level of the thoracic or cervical segment of the spinal cord. Vision may decrease symmetrically or in only one eye. The degree and speed of its loss varies from person to person, up to complete blindness. Severe clinical manifestations also include decreased sensitivity, leading to dysfunction of the intestines and bladder.
The reasons for the development of Devic's syndrome are not clear. There is some connection with past infectious diseases - in most patients, the first manifestations of the disease were preceded by fever and other phenomena characteristic of a viral or bacterial infection. It is difficult to say whether they were a true manifestation of a possible immune reaction to pathogenic flora or whether they represented a prodromal period of neuromyelitis optica itself.
A must read! Help with treatment and hospitalization!
Devic's neuromyelitis optica: causes, symptoms, diagnosis
Devic's neuromyelitis is considered a separate nosological entity, although the morphological substrate of the syndrome resembles multiple sclerosis.
Selection into a separate category is due to the need for unique treatment. Incorrect diagnosis makes early therapy impossible and irreversible changes occur, so we recommend immediately doing an MRI of the brain for early verification of the pathology. There are two forms of Devic's disease (DD):
- Transverse myelitis - affecting the spinal structures (LETM);
- Neuritis (acute, subacute) – accompanied by an inflammatory process of the optic nerve.
Correct treatment is possible only with timely diagnosis of the varieties of the disease.
Devic's opticomyelitis MRI in lateral projection
2. Clinical picture and diagnosis of Devic syndrome
Manifestations of Devic's disease are not specific. They may well have a different origin. However, the picture always includes severe neurological disorders, such as:
- decreased visual acuity, blindness in one or both eyes;
- paralysis and paresis of the lower extremities;/li>
- loss of skin sensitivity;
- dysfunction of the bladder, intestines, sphincters.
The full symptom complex develops over two months with a gradual increase in the severity of the disorders. The disease occurs in multiphases. Characteristic is the alternation of relative remission with acute periods. Usually, at the first manifestations, patients go to the hospital because they significantly lose important functions. For the purpose of differential diagnosis, a set of diagnostic measures is carried out. Devic's syndrome can be distinguished from other types of multiple sclerosis, as well as any other neurological pathology can be excluded, based on the following signs:
- the presence of diffuse foci of inflammation, atypical for multiple sclerosis, leading to cerebral edema and hemorrhages;
- magnetic resonance imaging reveals plaques in the spinal cord, optic nerve and periventicular substance;
- necrotic lesions affect three or more segments of the spinal cord;
- there is a total or subtotal lesion across the diameter;
- at the initial stages, thickening of the spinal cord is diagnosed in areas affected by inflammation, and in the long term they atrophy;
- The optic disc is also initially characterized by swelling, and subsequently by atrophy;
- the brain is affected predominantly by small foci of inflammation.
Devic's syndrome can be differentiated from other diseases with similar symptoms through analysis that identifies specific markers.
Visit our Neurology page
Symptoms of neuromyelitis optica
The first signs that may indicate Devic's disease usually arise from the visual and optical systems:
- Muscles weaken and it becomes difficult for a person to move.
- There is a decrease in visual clarity, blurred vision, and the picture may appear double.
- The patient may complain of pain that is neurological in nature.
- In case of neuromyelitis optica, disruptions may occur in the proper functioning of the intestines.
- Muscle spasms often occur.
During a diagnostic examination, the doctor discovers that the patient has myelitis, an inflammation of the spinal cord, and optic neuritis, an inflammation of the optic nerve. Moreover, often the inflammatory process in these areas does not develop in parallel, but at intervals from several months to several years, and sometimes decades.
3. Treatment options for Devic syndrome and prognosis
Devic's disease can have an acute course. Pathology in this form most often develops as a complication of acute respiratory viral infection and is diagnosed as post-infectious demyelinating encephalomyelitis. In this case, treatment includes intravenous administration of immunoglobulin, methylprednisolone, and corticosteroids. If the disease does not acquire a chronic form, then the prognosis is quite favorable - we can talk about the possibility of a complete cure or with the preservation of minor residual disorders.
Severe chronic forms of Devic syndrome are incurable. The pathology progresses in waves and leads to death. Therapy for such patients includes symptomatic and supportive treatment.
In rare cases, Devic syndrome is diagnosed in children. In this case, the disease, as a rule, has a single-phase acute course. After achieving remission, exacerbations are not typical. Timely treatment, including immunosuppressive therapy and corticosteroids, gives a favorable prognosis. Relapses in those affected in childhood are rare.
About our clinic Chistye Prudy metro station Medintercom page!
How does Devic's disease affect vision?
In Devic's disease, optic neuritis usually precedes inflammation of the spinal cord. Damage to the visual system is severe and may affect one or both eyes. According to statistics, in 50% of cases, five years from the onset of the disease, patients are diagnosed with blindness.
Magnetic resonance imaging helps to identify damage to the optic nerve, as well as the evoked potential method, when changes in the electrical activity of the visual cortex of the brain are monitored using special equipment. These methods help to accurately identify lesions in the visual system and assess the degree of development of the disease.
Diagnostics
To make a diagnosis, a neurologist collects anamnesis, studies the results of a lumbar puncture and MRI. The disease must be distinguished from retrobulbar neuritis, acute disseminated encephalomyelitis, myelopathy, and recurrent myelitis.
To study the cerebrospinal fluid, a sample of cerebrospinal fluid is required. The acute phase of neuromyelitis optica is indicated by over 50 pleocytosis cells per 1 mm3. Oligoclonal bodies, which are typical for multiple sclerosis, can be found in only 20% of patients. Characteristic is the presence of NMO-IgG, antinuclear and antithyroid antibodies.
Consultation with an ophthalmologist is necessary, including testing of visual acuity and ophthalmoscopy. Examination of the fundus shows swelling of the optic nerve, pallor and blurring characteristic of neuromyelitis optica, even with an asymptomatic course of the disease. To clarify the diagnosis, a study of visual EP is indicated.
MRI will help visualize lesions in spinal segments. This disease is characterized by necrotic damage to two or more segments. MRI of the brain shows demyelination of the optic tracts. Pathology can be detected in the hypothalamus region while the remaining cerebral structures are intact. This picture helps differentiate neuromyelitis optica from REM and multiple sclerosis. They are characterized by necrotic lesions in the brain.
The absolute criteria include: acute myelitis, optic neuritis, and the absence of other lesions and the presence of NMO-IgG antibodies.
International Neurological Journal 1 (71) 2015
The article was published on p. 141-147
Neuromyelitis optica (ONM, ICD-10, G36.0) - Devic's neuromyelitis optica, Devic's syndrome or disease - is an idiopathic severe inflammatory demyelinating disease characterized by selective involvement of the optic nerves and spinal cord in the pathological process with relative intactness of brain structures.
For a long time, the traditional localization of ONM was considered as a pathology of the central nervous system in the form of a monophasic disease with bilateral damage to the optic nerves and the simultaneous or after a short period of time development of severe transverse myelitis. However, at the end of the 20th century, the definition of this disease became more universal, allowing for significant differences in the variants of the course (monophasic and remitting), the degree of involvement of the optic nerves (unilateral or bilateral damage), the sequence of development of the process in the spinal cord and optic nerves, and the specific features of the course of optic neuritis and myelitis (level of spinal cord damage is longitudinal and transverse, limited or widespread, involvement of gray or white matter).
The first case of such a combination of damage to the optic nerves and spinal cord was described by S. Allbutt in 1870.
By 1894, 16 cases had been accumulated in Europe and the USA, which, together with their own observation, E. Devic and his student F. Gault studied in detail and proposed to identify them as a separate nosological form [14]. However, for a long time the disease was traditionally considered within the framework of one of the malignant variants of multiple sclerosis (MS). Progress in studying the pathogenesis of demyelinating diseases of the central nervous system made it possible by the end of the 20th century to consider ONM not a rare variant of the course of MS, but a separate nosological form [1, 3].
Characterizing the epidemiology of ONM, it should be noted that in European countries it accounts for 1–2% of the structure of other demyelinating diseases of the central nervous system. This is probably due to the fact that many cases of ONM are often mistakenly interpreted as MS, recurrent transverse myelitis, recurrent retrobulbar neuritis [5].
ONM is an autoimmune disease that predominates among non-Caucasians. The ratio of women to men is (2–8): 1. The age at which the disease debuts varies from 1 year to 77 years, most often it begins at 35–47 years [9].
Isolated familial cases of Devic's neuromyelitis optica have been described in the literature.
Quite often, ONM (50–70%) is combined with other autoimmune diseases - Sjogren's syndrome, autoimmune thyroiditis, rheumatoid arthritis, systemic lupus erythematosus, pernicious anemia, ulcerative colitis, primary sclerosing cholangitis, thrombocytopenic purpura.
Devic's disease occurs in Southeast Asian countries, especially in Japan, predominating in middle-aged women [15].
In 2004, NMO-IgG antibodies specific to ONM were first identified, which were detected in 63–73% of patients. Their presence confirmed the autoimmune mechanisms of the pathogenesis of neuromyelitis optica.
Such antibodies are absent in patients with classic MS, in inflammatory and non-inflammatory diseases of the central nervous system, in other autoimmune diseases and in healthy individuals [1].
The target of the antibodies is aquaporin-4, isolated in 2005, a protein channel that regulates the water balance of the nerve cell. It is closely associated with the blood-brain barrier, with elements of the dextroglycan complex in the area where astrocytes adjoin the vascular wall. The highest concentration of aquaporin-4 in the central nervous system was observed in the gray matter of the spinal cord, hypothalamus, and periventricular areas [11].
The disease usually affects the optic nerve, chiasm, spinal cord, hypothalamus, and brain stem. Pathophysiologically, with ONM, demyelination and necrosis of white and gray matter occur. In this case, the inflammatory infiltrate contains a large number of polymorphonuclear leukocytes, macrophages, and eosinophils, which distinguishes ONM from MS. There is hyalinosis of the medium-sized spinal cord arteries, which is usually accompanied by necrosis of the spinal cord.
In areas of demyelination and around vessels, deposition of complement components and IgG is found, associated with fibrosis and vascular proliferation [9].
Chronic foci of inflammation in the brain are represented by cystic degeneration, gliosis and atrophy of nervous tissue, which can lead to the development of secondary syringomyelia [10].
To date, the identification of focal lesions of the nervous system outside the optic nerves and spinal cord does not contradict the diagnosis of ONM.
The described features of morphological changes in the spinal cord may resemble autoimmune inflammation occurring as vasculitis. In almost 100% of cases, vascular hyalinization is detected in spinal foci of inflammation, therefore there is a component of vasculitis in ONM. Such changes are not found in typical MS lesions, infarct lesions, or in lesions of acute disseminated encephalomyelitis. In contrast to typical MS, the leading role of B cell-induced reactions is assumed in the pathogenesis of ONM.
A similar immunopathological reaction is discussed in severe relapsing-remitting and secondary progressive MS.
In some cases, ONM serves as a manifestation of systemic lupus erythematosus, antiphospholipid syndrome, and pulmonary tuberculosis.
The special role of humoral immunity in ONM may also be one of the main differences between its pathogenesis and MS. This assumption is supported by the recent discovery of plasma autoantibodies NMO–IgG Devic [11].
The main target for the immune response, as mentioned above, is aquaporin-4 (AQPH). Serum antibodies (NMO-IgG) bind to cerebral microvessels, pia mater, and Virchow-Robin spaces. Aquaporin-4, located in the processes of astrocytes or covering areas of vessels not covered with astrocytic stalks, is involved in the formation of the blood-brain barrier and, if it is damaged, cannot cope with its function.
Damage to astrocytes promotes access of other immune complexes to the central nervous system and activates the formation of an autoimmune process in it [10]. In Devic's syndrome, the sheath of the fat-like substance of astrocytes that protects the optic and spinal nerves is affected.
Therefore, initially in the clinical picture of the disease, visual impairment occurs in the form of its decrease, up to complete loss, and after some time the symptoms of severe transverse myelitis are added - paraparesis, tetraparesis, dysfunction of the pelvic organs.
Currently, it is accepted that ONM can have both a monophasic and remitting type of course. However, repeated attacks with it are less typical, as are remissions.
Analyzing the clinical course of ONM according to 71 patients for the period 1950–1997, I. Miyazawa et al. (2002) showed that ONM can be either monophasic or remitting. In the latter case, a severe exacerbation of optic neuritis or myelitis develops within 3 years. In a third of cases, the cause of death is the development of respiratory disorders [12].
With a general tendency towards a poor prognosis, several possible outcomes are possible. In some cases, complete recovery is assumed; another variant of the course of ONM is the presence of remissions of the disease. The most unfavorable option occurs as progressive deterioration and death of the patient.
Analyzing the prognostic significance of the type and characteristics of the course of ONM, D. Wingerchuk et al. [12] noted that the outcome is worse in the group of patients with a monophasic course of the disease, as well as with a persistent decrease in visual acuity and persistent paralysis.
Predictors of the relapsing-remitting form of ONM are longer intervals between the first two attacks, older age at onset of the disease, female gender, and less severe motor deficits in spinal cord lesions.
Residual severe deficits after an acute attack are more common in ONM than in MS [5], which has a certain differential significance.
One of the main symptoms of ONM is optic neuritis. Ophthalmoscopy often reveals a normal fundus picture, slight blurring of the optic discs, mild swelling, atrophy and pallor of the optic discs in chronic cases.
In ONM, optic neuritis, usually bilateral, usually precedes myelitis (in 80% of cases). After a few weeks, or less often months, severe transverse myelitis develops. In most cases, the development of myelitis occurs in less than 3 months. However, in 20% of cases, transverse myelitis may precede optic neuritis [4].
Damage to the spinal cord during ONM can occur in an isolated form. In this case, the course is acute partial transverse or longitudinal widespread myelitis. The development of complete transverse myelitis in MS is quite rare.
A study conducted in groups of patients with ONM, longitudinal widespread myelitis, and acute partial transverse myelitis showed that in the presence of NMO-IgG immunoglobulins, longitudinal widespread myelitis can be considered as an incomplete form of ONM.
Typical symptoms of myelitis are muscle weakness, spasticity, incoordination, ataxia, Lhermitte's sign, urinary retention, autonomic dysfunction, and possible sonority disorders below the level of spinal cord damage.
With a monophasic type of course (less than 20% of patients with ONM), unilateral or bilateral optic neuritis and transverse myelitis develop simultaneously, then repeated episodes of myelitis and/or optic neuritis are not recorded.
In the recurrent course of ONM, on the contrary, the first attacks of optic neuritis and myelitis can be separated in time by weeks or even years, but optic neuritis, or myelitis, or both of these conditions recur over the next months or years; During the first year, relapse occurs in 55% of patients; during the first 3–5 years, in 78 and 99%, respectively [6].
In patients with a recurrent monophasic course of the disease, despite the greater initial severity of the disorders, the long-term prognosis is better, since there is no accumulation of neurological deficits that occur with repeated attacks.
In the literature there are indications of an atypical onset of Devic's disease. Thus, a number of scientists noted that before the onset of neurological symptoms, there was a prodromal period in the form of fever, infection, and other autoimmune diseases.
Norajima et al. (2011) [6] report a very rare, atypical debut of Devic’s disease - a syndrome of inappropriate secretion of antidiuretic hormone. According to the authors, in the presence of this syndrome with no signs of damage to the optic nerves and spinal cord and in the presence of MRI-confirmed lesions in the hypothalamus, Devic syndrome should be considered as a possible cause of this condition.
E.G. Mendelevich et al. (2004) report 2 clinical observations of ONM complicated by syringomyelic cavities formed in areas of necrosis of inflammatory foci in the spinal cord. The authors suggest the pathogenesis of syringomyelia as a result of discirculation of cerebrospinal fluid (CSF) in the central spinal canal and subarachnoid spaces of the spinal cord in the presence of a necrosis zone in the spinal cord. A lethal outcome of ONM can occur as a result of a severe attack of myelitis involving the cervical spinal cord and the development of respiratory failure.
The disease occurs single-phase, rarely multiphasic. As mentioned above, neuromyelitis optica (Devick's syndrome) is characterized by unilateral, often simultaneous bilateral, severe damage to the optic nerves with swelling in the acute period and atrophy subsequently.
Changes in the optic nerves are visible both during fundus examination and neuroimaging; the latter, unlike MS, involve the optic nerves over a large area. In almost all cases, ONM must be differentiated from MS.
In contrast to ONM, in MS, demyelination foci in the spinal cord usually do not exceed one segment in length. MRI of the brain with ONM either does not reveal any pathological changes, or (in 50–60% of cases) nonspecific, often asymptomatic foci of demyelination are detected.
In some cases, there is more massive brain damage consistent with multiple sclerosis.
MRI indicators are different in different clinical variants of acute demyelinating encephalomyelitis and in neuromyelitis optica [16].
MRI reveals typical changes in the spinal cord during ONM. In most cases, lesions are visualized that extend over more than two vertebral segments, usually of a necrotic nature (Fig. 1).
Additional opportunities are provided by the results of CSF analysis and its examination for the presence of oligoclonal bands.
Differential diagnosis is also carried out with acute demyelinating encephalomyelitis (ADEM), which occurs shortly after an infection or acute respiratory viral infection and is symptomatically similar to neuromyelitis optica.
In contrast to Devic's syndrome, some patients with ADEM end in complete recovery; in some cases, residual effects persist [10].
Modern diagnostic criteria for Devic's opticomyelitis were formulated by D. Wingerchuk [5] and include three “absolute” criteria: 1 - the presence of optic neuritis, 2 - the presence of acute myelitis, 3 - the absence of clinical manifestations of the disease outside the optic nerves and spinal cord.
In addition, to confirm the diagnosis, the presence of one of the “major” confirming criteria is necessary: 1— absence of MRI changes in the brain; 2 - focal changes in the spinal cord extending at the level of three vertebral segments or more; 3 - presence of pleocytosis in the CSF of more than 50 cells per 1 mm3 or more than 3 neutrophils per 1 mm3.
“Minor” confirmatory criteria include 2 of the following: 1 - bilateral optic neuritis; 2 - severe optic neuritis with permanent loss of vision in at least one eye; 3 - severe persistent residual weakness of one limb or more.
New criteria for ONM are autoantibodies—NMO–IgG markers. Therefore, the combination of clinic, MRI data and assessment of NMO-IgG status provides the maximum diagnostic opportunity compared to individual components of the diagnosis.
Currently, with ONM, the possibility of involving central nervous system structures outside the optic nerves and spinal cord is accepted. There are descriptions of clinical cases where patients with an objective diagnosis of ONM have a combination of the clinical picture of neuromyelitis optica with asymptomatic or symptomatic lesions in the brain, for example, in the projection of the structures of the hypothalamic-pituitary axis [9].
This is explained by the fact that NMO-IgG, being specific markers of ONM, selectively binds to aquaporin-4 (AQP4), the concentration of which is significantly increased in different parts of the brain. This explains why brain changes outside the optic nerves and spinal cord are localized to the hypothalamus, periventricular areas - precisely where AQP4 expression is highest. In addition to ONM, high expression of this protein has been detected in patients with epilepsy and certain types of tumors. It is believed that ONM may represent an unknown variant of autoimmune channelopathy. It has been suggested that the binding of autoantibodies to AQP4 may result in direct damage to the function of ion channels with the development of swelling, or the antibodies may activate complement, which subsequently initiates the aggressive inflammatory response characteristic of ONM. The immunological characteristics of demyelinating disease variants also differ, allowing some cases to be interpreted as atypical MS.
In the blood serum of patients with ONM, in almost half of the cases, antibodies (antinuclear, to extractable nuclear antigens, to double-stranded DNA, antithyroid) and their combinations are detected, which indicates the predisposition of these patients with endocrinopathies to the development of autoimmune diseases [10].
During an attack of myelitis with OM, cerebrospinal fluid analysis in one third of patients shows pleocytosis (> 50 leukocytes per 1 mm3) with the presence of neutrophils and an increase in protein levels within varying limits. Such changes are rarely observed in MS [3]. A stratified approach to the treatment of ONM in the future may allow systematization of these rare forms of demyelinating diseases.
Currently, there is no generally accepted standard for the treatment of Devic's syndrome. Symptomatic and restorative treatment is used to support existing neurological functions.
Corticosteroids may be prescribed. One treatment option is the use of drugs that partially block B cells, such as rituximab. For pathogenetic treatment, six drugs that modify the course of the disease are registered in the world. Three of them belong to the group of interferons; interferons beta-1a, betfer-1a and interferons beta-1b and betfer-1b [7].
High doses of corticosteroids are used to treat attacks of myelitis and optic neuritis. Along with this, the use of plasmapheresis is also effective.
The effectiveness of preventive immunomodulatory therapy in patients with ONM has not been formally studied. There is conflicting information about the effectiveness of interferon beta-1 and immunosuppressive therapy. The treatment of choice is a combination of prednisolone and autoprin.
Treatment of patients with ONM is always a difficult task. Its basis is the earliest possible start of immunosuppressive therapy. Clinical data suggest that plasmapheresis and immunosuppressive therapy are more indicated for the treatment and prevention of attacks, and standard immunomodulatory therapy does not have a significant effect on the course of ONM.
Despite the therapy, Devic's syndrome in many cases leads to death [8].
We present our own clinical observation of Devika, a patient with neuromyelitis optica.
Patient K.N.V., born in 1983, does not work.
She was admitted to the neurological department with complaints of lack of movement in the lower extremities, a feeling of numbness in the lower half of the body and legs, and dysfunction of the pelvic organs such as retention.
In August 2011 (6 months after the second birth), pain appeared in the thoracic spine. Symptoms increased over the course of 2 weeks: pain in the spine intensified, numbness and weakness appeared in the right leg. 09/05/11, accompanied by relatives, turned for help to the Kyiv Regional Hospital (in the department of vascular pathology and diseases of the central nervous system), where the diagnosis was made: acute myelitis of the thoracic spinal cord at the Th4–Th8 level, Brown-Séquard syndrome (she was inpatient treatment) . As a result of the therapy, positive dynamics were noted: the strength in the right leg increased to 4 points, sensitivity was restored, and pain in the spine disappeared. In February 2013 (during the third pregnancy), the patient experienced symptoms of the n.trigeminus type of neuralgia, followed by regression of facial pain. The real deterioration of the condition since 08/05/13 (1.5 months after the third birth) was manifested by severe pain in the thoracic spine. Over the course of a week, the symptoms progressed: numbness of the lower half of the torso and lower extremities developed. On 08/10/13, severe weakness in the lower extremities and delay-type dysfunction of the pelvic organs appeared, and on 08/11/13 the patient, accompanied by relatives, was urgently taken to the emergency department of the Regional Clinical Hospital.
Neurological status (at the time of examination in the neurological department): clear consciousness, asthenized, emotionally labile, fixed on her feelings. Palpebral fissures D = S, pupils D = S, their photoreactions are live, ophthalmodynamics are not impaired. The face is symmetrical. Active movements in the hands in full; there is no movement in the legs (lower paraplegia), muscle tone in the legs is increased in a pyramidal pattern, (+) Babinski’s symptom on both sides. Tendon reflexes from the upper extremities are brisk, D = S; high, from lower D = S. Conduction type hypoesthesia from level Th4. Dysfunction of the pelvic organs by type of delay.
Surveys
RV dated 04/11/13: negative.
UAC dated 08/13/13: E 4.01 T/l, L 6.6 G/l, Hb 105 g/l; ESR 11 mm/h; n 1, s 78, l 10, m 11; anisocytosis is weakly expressed.
UAC dated 08.27.13: E 4.10 T/l, L 7.6 G/l, Hb 108 g/l; ESR 14 mm/h; e 2, p 7, b 1, m 4, l 22, p 64; anisocytosis.
Blood test for LE cells dated 08/14/13: not detected.
Coagulogram dated 08/27/13: PTV 18”; PTI 80.5%; INR 1.31; APTT 28".
Tests for the activity of rheumatism from 08/14/13: CRP (=); RF (–); antistreptolysin–O (–); seromucoids - 0.29.
RG OGK dated 08/11/13: no pathological changes in the chest organs were detected.
Antibodies to aquaporin-4 from 08/15/13: anti-aquaporin-4 IgA, G, M (IgA - negative, IgG - +++ 1: 320, IgM - negative); serological diagnosis: Neuromyelitis optica (NMO), opticospinal encephalomyelitis, Devic syndrome Anti-Hu - negative. Anti-Ri - negative. Anti-Yo - negative. Anti-Tr - negative. Anti-MAG - negative. Anti-Myelin - negative. Anti–Ma/Ta – negative. Anti-GAD - negative. Anti-Amphiphysin - negative. Anti-Glutamat Rezeptoren - negative. Anti-Gaba-b-Rezetoren - negative. Anti-LGIl - negative. Anti-CASPR2 - negative. Anti-Glycinrezeptoren - negative.
Blood test for TORCH infections dated 08/15/13: IgG antibodies to CMV - 2.53; IgG antibodies to HSV - 3.65, IgG antibodies to Rubella - 3.36, IgG antibodies to Toxoplasma gondii - 2.57; IgM antibodies to HSV - 0.52, IgM antibodies to Rubella - 0.07, IgM antibodies to Toxoplasma gondii - 0.13.
MRI of the brain dated 08/12/13: no volumetric or focal changes in brain structures were detected.
MRI of the thoracic spine dated 08/12/13: on a series of sagittal, coronal and axial sections of the thoracic spine in T1- and T2-weighted images when compared with an MRI study dated 09/02/11 in the structure of the spinal cord at the level of Th4–Th9 (up to the upper edges of the Th9 vertebral body) a centrally located zone of pathological changes in signal intensity is preserved, extending to almost the entire thickness of the spinal cord, hyperintense in T2-WI, STIR, isohyperintense in the FLAIR sequence. At the level of Th11–Th12 and in the projection of the epiconus, another focus of a hyperintense nature in T2-WI, STIR, of a hypointense nature in T1-WI, which was also determined on previous images, is visualized. Conclusion: changes in the structure of the spinal cord may be caused by a diffuse form of transverse myelitis. When compared with the MRI study of 09/02/11, some progression of the underlying disease is noted. Intravenous contrast enhancement was recommended; the patient refused the administration of a contrast agent. Signs of a degenerative-dystrophic process such as osteochondrosis. Discopathy at the Th7–Th8 level.
Hematologist dated 08/16/13: diagnosis: anemia caused by neurological pathology and after pregnancy. Recommended: gyno-tardiferon 1 tablet. 1 rub. per day 1 month; preparations of B vitamins; monitoring of peripheral blood parameters over time.
Gynecologist dated 08/12/13: no gynecological pathology was detected.
Ophthalmologist dated 08/12/13: diagnosis: optic nerve atrophy.
Visual EPs 08/12/13 - the amplitude of the response is reduced with deformation of the VEP complex symmetrically. Signs of axonal damage to both optic nerves were revealed.
Urologist dated 08/14/13: neurogenic bladder of hypotonic type, against the background of myelitis. Recommended: omnix 1 k. per night for 1 month; no-shpa 1 table. 3 r. per day 10 days; Dicloberl suppositories 50 mg, 1 stick. 1 rub. per day 10 days; palin 2 tablets. 2 r. per day 14 days; rinse the urethral catheter with sterile saline solution 10.0 ml + decasan 10.0 ml 2 r. in a day. Urologist dated 09/06/13: neurogenic bladder. Acute urinary retention.
Recommended: install a permanent urethral catheter; catheter care - dekasan 4 ml + 16 ml saline. solution - rinse 1 r. in a day; Canephron 2 tablets. 3 r. per day 1 month. Treatment given: solu-medrol (1000 mg intravenously for 7 days); L-lysine aescinate, gliatilin, neurobion, essentiale, sulfocamphocaine, proserin, ATP, analgin, diphenhydramine, cefatoxime, omnix, alora, herbastress, dostinex, omez, Keltican, Tonginal, ATP-long. Exercise therapy, massage of the lower extremities. EF with proserin on the bladder area; electrical stimulation of the lower extremities, plasmapheresis (3 sessions).
During the hospital stay, no intolerance to medications was noted.
As a result of the treatment, some positive dynamics were noted in the patient’s condition: minimal movements appeared in the distal parts of the lower extremities (movements in the left foot and in the toes of the right foot), she began to sit up independently, turns in bed, the urge to urinate and defecate appeared, sensitivity was restored in lower extremities to the level of the upper third of the thighs.
The neurological symptoms present in our patient clearly characterize damage to the optic nerves and thoracic segments Th11–Th12 of the spinal cord. The presence of antibodies to aquaporin-4 indicates an active autoimmune process. The clinical course of the disease is assessed as remitting, since the next attack of ONM occurred in the postpartum period and was accompanied by damage to the same organs, which was confirmed by neuroimaging.
In the hospital, differentiation was carried out with the relapsing course of the spinal form of MS, acute necrotizing transverse myelitis of Alajuanin. The onset and exacerbation of the process after childbirth, the presence of 2 lesions (optic nerves and spinal cord), as well as the transient nature of prosopalgia, which regressed on its own, testified in favor of MS.
Symptoms such as transverse myelitis, which, according to MRI of the spinal cord, spread classically - longitudinally over 2-3 segments, absence of changes on MRI of the brain, as well as the presence of antibodies to aquaporin-4 IgG, may indicate against MS.
Acute necrotizing transverse myelitis of Foix-Alajouanin was also supported by the acute development of the disease, characterized by transverse lesions of the thoracic spinal cord with the development of spinal sensorimotor and sphincter disorders corresponding to this level of lesion.
In addition, with necrotizing transverse myelitis, various types of sensory disorders such as Brown-Séquard syndrome, posterior columnar, spinothalamic in nature, early trophic disorders in the form of bedsores, inflammatory nature of the cerebrospinal fluid, and possibly blood, are observed.
In addition, damage to the optic nerves is atypical for this disease.
Taking into account the fact that our patient, along with atrophy of the optic nerves, had no inflammatory changes in the CSF and peripheral blood, posterior columnar and segmental types of sensory disorders, or bedsores, the diagnosis of transverse myelitis was removed.
There is no doubt that the initial diagnosis is currently neuromyelitis optica (Devic's disease). However, given the common autoimmune pathogenetic mechanisms of this disease and MS, it is not possible to exclude the possibility of transformation into MS.
In this regard, dynamic monitoring of the patient and appropriate immunological control are justified.
The clinical diagnosis can be formulated as follows: neuromyelitis optica (Devic's disease), remitting course, exacerbation, lower spastic paraplegia, dysfunction of the pelvic organs by the type of delay, atrophy of the optic nerves of both eyes.
General information about the disease
The first time a similar clinical picture was described was in 1870. By 1894. Devik outlined 16 cases of this pathology and made a proposal to include it in a separate nosology. Before this, neuromyelitis optica was considered a severe form of multiple sclerosis. By the end of the 20th century, Devic's disease began to be considered an independent disease. It is most widespread in Southeast Asia. Mostly women aged 35-47 years are affected. But debut is possible between the ages of 1 and 77 years. According to statistics, for every 1 sick man there are 2-8 representatives of the fairer sex.
Demyelination
Demyelinating brain disease according to ICD-10 has codes G35, G36 and G77. The process caused by damage to the nervous tissue negatively affects the functioning of the entire organism as a whole. Certain nerve endings are covered with a myelin sheath, which performs important functions in the body. For example, myelin ensures the rapid transmission of electrical impulses and, accordingly, if this process is disrupted, the entire system suffers. Myelin consists of lipids and protein compounds in a 70/30 ratio.
Demyelinating disease is not only multiple sclerosis, it is also neuromyelitis optica and acute disseminated encephalomyelitis. These diseases have no cure, but their progression can be slowed down. In general, doctors give a favorable prognosis when treating these pathologies. The diagnosis of “multiple sclerosis” is now made more often, but the disease itself is milder than 30-40 years ago.
Make an appointment
Causes
The pathogenesis of the disease is not fully understood. Now it is classified as an autoimmune disease. In 2004, specific NMO-IgG antibodies were identified. They can be found in 65-73% of patients. This makes it possible to differentiate the disease from multiple sclerosis, inflammatory lesions of the central nervous system, and REM. The target for antibodies is the protein channel aquaporin-4. It is predominantly located in the tissues of the spinal cord, in the hypothalamus and periventricularly. Localized in the walls of the blood-brain barrier and in the processes of astrocytes. Therefore, damage to these channels leads to an increase in the permeability of the barrier and the penetration of immune complexes through it. This is how autoimmune inflammation occurs.
With neuromyelitis optica, necrosis of gray and white matter begins. Zones of demyelination appear. The pathology extends to the optic nerves, spinal cord, chiasm and hypothalamus. IgG deposits accumulate perivascularly and in areas of demyelination. Spinal foci of inflammation are represented by atrophy, gliosis and cystic degeneration. Cavities characteristic of syringomyelia may also form. Almost all patients have autoimmune vasculitis.
Therapy
Treatment of this disease requires an integrated approach. It is complicated by the contradictory results of the use of immunosuppressive and immunomodulatory drugs. Of the 6 drugs registered in the world for the treatment of neuromyelitis optica, 3 are interferons with unproven clinical effectiveness. Plasmapheresis and high doses of corticosteroids can stop attacks. If there is no effect, mitoxantrone and rituximab may be prescribed. Prednisolone can prevent exacerbation.
Symptomatic therapy includes:
- Antidepressants;
- Muscle relaxants;
- Intrathecal baclofen infusion;
- Physiotherapeutic procedures: SMT, electrophoresis, paraffin therapy;
- Massage;
- Exercise therapy.
Treatment
Treatment of Devic's neuromyelitis optica is a difficult process. The main goal of doctors is to slow down the progression of pathology and improve the patient’s quality of life. For pathogenetic therapy, drugs that inhibit B-cell function (mitoxantrone) were previously popular. At the moment, monoclonal antibodies that suppress autoimmune inflammation are considered more effective. An example is rituximab.
To stop the exacerbation of the disease, glucocorticosteroids are used in large doses - prednisolone, hydrocortisone, dexamethasone. Partial blood purification from circulating immune complexes is carried out using plasmapheresis.
Symptomatic therapy is used to improve the patient's quality of life.
Groups of drugs used:
- Muscle relaxants. Medicines reduce pathological hypertonicity. Representatives: dantrolene, tolperisone.
- Antidepressants. Improves the emotional state of patients. Representatives: imipramine, amitriptyline.
- Centrally acting painkillers – pregabalin.
Therapeutic exercise and physiotherapy are auxiliary techniques that help increase the effectiveness of basic therapy. The practice uses electrophoresis, massage, and paraffin baths.
Development mechanisms
The nervous system consists of central and peripheral sections. The regulation mechanism between them works as follows: impulses from the receptors of the peripheral system are transmitted to the nerve centers of the spinal cord, and from there to the brain. The disruption of this complex mechanism causes demyelination.
Nerve fibers are covered with a myelin sheath. As a result of the pathological process under consideration, this membrane is destroyed and fibrous tissue is formed in its place. She, in turn, cannot conduct nerve impulses. In the absence of nerve impulses, the functioning of all organs is disrupted, since the brain cannot issue commands.