HIV infection is a progressive anthroponotic disease with a predominantly contact mechanism of infection, characterized by specific damage to the immune system with the development of immunodeficiency, which is manifested by the development of opportunistic infections, malignant neoplasms, and the occurrence of autoimmune reactions.
Since the beginning of the study of HIV infection, more than 60 million people with HIV have been registered in the world. This problem is especially acute for Russia and the CIS countries, where the incidence of HIV is higher than in other regions of the world [1]. There are more than 700 thousand patients in Russia, and the estimated indicators exceed the actual detection rate by 2-4 times [2, 3].
Due to the introduction of highly active antiretroviral therapy (HAART) into clinical practice, HIV infection has moved from the category of a fatal disease to a chronic, drug-controlled disease with a human life expectancy of several decades. However, the prevalence of the disease remains high.
HIV has great genetic diversity, forming types, groups, subgroups and recombinant forms, which can (in addition to common properties) due to genetic differences acquire biological characteristics, including tropism for damage to the central nervous system, which has been the subject of active discussion in recent years [4] . In terms of the frequency of damage to various organs and systems during HIV infection, which causes acquired immunodeficiency syndrome (AIDS), the nervous system (neuroAIDS) is in second place after the immune system. This is associated with many pathogenetic mechanisms of damage to both the central and peripheral nervous systems [5]. According to autopsy data, pathomorphological changes in the nervous system occur in 70-80% of those who died from AIDS. Damage to the central nervous system during HIV infection is, as a rule, an important disabling factor. 40-60% of patients have a variety of neurological, mental and cognitive disorders, which significantly complicates their social adaptation, and in severe cases leads to complete disability.
Neurological manifestations of HIV infection can be caused by HIV itself, as well as by opportunistic infections, neoplasms, and the toxic effects of antiretroviral drugs. The direct effect of HIV on cells of the nervous system is to infect and destroy cells that have the CD4 receptor (microglial cells, astro-, mono-, oligodendrocytes, endothelial cells of blood vessels and neurons themselves) [6]. In addition, CNS cells are destroyed by the membrane protein gp 120, which plays a key role in the pathogenesis of neuronal damage by blocking neuroleukin. Various pathogenetic mechanisms can lead to clinical manifestations with a variety of neurological deficits [7].
Complex biochemical disorders play an important role in the pathogenesis of neurological disorders. Changes in the regulatory activity of the hypothalamic-pituitary system lead to disturbances in neurotransmitter metabolism, deficiency of γ-aminobutyric acid and glycine, which are associated with the development of epileptic seizures, a decrease in serotonin production leads to depressive disorders and ataxia, impaired vasopressin metabolism leads to memory disorders, damage to endothelial cells choroid plexus of the meninges and ventricular ependyma - to the development of secondary demyelination; depression of cellular immunity - to the development of opportunistic infections and neoplastic processes. As a rule, there is a combination of these factors, which determines the clinical manifestations of CNS damage in a particular patient.
Currently, a number of primary and secondary lesions of the central nervous system are identified in HIV infection:
— acquired immune deficiency syndrome, combining manifestations of infectious and degenerative processes (neuroAIDS);
— AIDS dementia syndrome;
— HIV-associated neurocognitive disorders (HAND);
— HIV-associated encephalopathy;
— HIV-related lesions of the central nervous system (primary);
— opportunistic lesions of the central nervous system [1].
Primary lesions of the nervous system in HIV include disorders associated with the direct influence of the virus: NAND, HIV-associated encephalo-, myelo-, polyneuropathies, other CNS lesions caused by HIV infection (aseptic meningitis, meningoencephalitis). HAND is a clinical diagnosis in HIV-infected patients with cognitive impairment if, based on clinical and laboratory studies, infectious and metabolic lesions of the central nervous system, depression and other causes are excluded. Establishing a diagnosis requires a holistic assessment of the patient’s virological and immune status, an assessment of the nature of the medications he is taking, drug use, analysis of concomitant diseases, as well as a neuro- and neuropsychiatric examination. HAND is not usually associated with impaired level of consciousness, focal neurological symptoms, or signs of systemic injury.
HIV-associated mild cognitive-motor disorders
occur in more than 80% of AIDS patients [8]. A neurological examination carried out in the initial stages of the disease may not reveal any abnormalities, however, neuropsychological testing, as a rule, reveals impairments in the performance of neuropsychological tests corresponding to moderate or more severe cognitive impairment. On examination, signs of diffuse symmetrical damage to the pyramidal tracts, hyperreflexia and symptoms of damage to the frontal lobes may be revealed. Detected disorders include motor and psychomotor retardation, impaired attention, inability to concentrate, mental disorders, difficulties in learning and information processing [9]. In the early stages of the disease, short-term memory suffers, which is associated with impaired memorization and retrieval of information.
HIV encephalopathy (AIDS-dementia complex), as a rule, develops in the later stages of HIV infection and has varying severity of symptoms up to the development of dementia. Syndromologically, it is a subcortical dementia that usually develops over several weeks or months. The acute development of neuropsychological symptoms indicates another cause of encephalopathy. Often the first manifestations of encephalopathy are first noticed by the patient’s relatives, and not by the patient himself. Characteristic symptoms include slowness of thinking, forgetfulness, difficulty concentrating, a feeling of loss of energy, manifestations of depression, dulling of emotions, difficulty performing fine movements (for example, when writing, fastening buttons), the appearance of an imperative urge to urinate, and erectile dysfunction.
There are several groups of symptoms of HIV encephalopathy:
1. Neurological: at an early stage they may be absent or have insignificant severity. Possible gait disturbances, slowdown in rapidly alternating movements, hypomimia, and tremor. Subsequently, there is an increase in reflexes, the appearance of pathological reflexes, a slowdown in saccadic movements of the eyeballs, pelvic disorders, and the possible development of concomitant polyneuropathy. The terminal stage is characterized by the development of spastic tetraplegia and urinary and fecal incontinence. 2. Cognitive impairment with slow psychomotor activity, disorders of short-term memory and attention switching. The dynamics of mental disorders also have a staged nature. At an early stage of the disease, increased distractibility, dullness of emotions, flattened personality traits, and lack of initiative are detected. In later stages, the patient may be disoriented in time, space and situation. As a result, mutism usually develops.
Impaired consciousness, meningeal symptoms, and focal neurological symptoms are not typical for HIV encephalopathy. Psychotic disorders (without cognitive or motor impairment) also do not meet the diagnosis of HIV encephalopathy. Rarely, such encephalopathy manifests itself with partial or generalized convulsive seizures.
The diagnosis is mostly made by exclusion. Cognitive and mental disorders are always combined with motor ones, although the latter may be mild. To identify and assess the severity of cognitive impairment in HIV encephalopathy, it is convenient to use appropriate psychometric semi-quantitative scales [10].
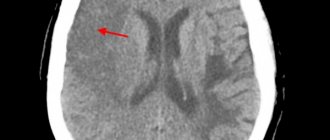
Laboratory and instrumental studies are aimed mainly at excluding other causes of neurological disorders. Of the neuroimaging methods, it is preferable to use MRI, which reveals signs of leukoencephalopathy (relatively symmetrical focal and diffuse changes in the density of the white matter of the brain), which never extend to the cortical parts. Sometimes there is atrophy of the brain substance with expansion of the ventricles and sulci of the cerebral hemispheres. Brain swelling, tissue compression, and contrast-enhanced MR signal enhancement are not characteristic of HIV encephalopathy and should suggest some other process, although mild symmetrical diffuse contrast enhancement of the MR signal from the basal ganglia is possible. These changes are not specific. Sometimes there are no changes on MRI. There are no focal changes on the EEG; sometimes mild signs of diffuse slowing of bioelectrical activity are detected.
Changes in cerebrospinal fluid (CSF) are nonspecific. In patients receiving highly active antiretroviral therapy (HAART), pleocytosis may be detected in the CSF, indicating an immunological response to HIV as the immune system recovers. Even before the widespread introduction of HAART into clinical practice, a weak but statistically significant relationship was established between a high viral load in the CSF and the severity of HIV encephalopathy.
Treatment of HIV encephalopathy should be aimed at suppressing HIV replication in the central nervous system, therefore the main focus of therapy is the administration of antiretroviral drugs. Preference should be given to drugs that penetrate the blood-brain barrier well. HAART led to a 2-fold reduction in the incidence of HIV encephalopathy [11, 12], while life expectancy increased from 6 to 48 months or more. The number of CD4 cells in peripheral blood during treatment increases from 50-100 per 1 μl to a normal level [13]. With HAART, significant clinical improvement in the course of HIV encephalopathy can be observed, even restoration of work ability in patients who previously required outside care. During the first months of treatment, despite significant clinical improvement, neuroimaging signs of leukoencephalopathy may increase, but gradually disappear over the next 1-2 years. It is currently believed that the presence of even minimal cognitive impairment is a sufficient basis for prescribing HAART [14]. The additional administration of nootropic and neurometabolic drugs is of an auxiliary nature, since it is not able to reduce the replication of the virus, but can help slow down the neurodegenerative processes caused by it.
Acute HIV-associated meningoencephalitis
is the most severe acute, rare form of primary CNS damage in HIV infection. Acute encephalitis is associated with direct damage to brain cells by the human immunodeficiency virus. The development of HIV meningoencephalitis coincides with or even precedes changes in the results of serological studies. At the onset of the disease, depression of consciousness (even coma) and epileptic seizures are possible. Neurological symptoms can completely regress within a few weeks, but in the future, some patients who have suffered acute meningoencephalitis may develop chronic HIV encephalopathy. A somatic examination may reveal generalized lymphadenopathy, splenomegaly, maculopapular rash, and urticaria. Nonspecific inflammatory changes in the form of pleocytosis are detected in the CSF; Neuroimaging signs of brain damage may be absent.
In the acute stage, the differential diagnosis is made with encephalitis caused by the herpes simplex virus. The latter can be excluded if, within 3 days, a repeat CT scan does not reveal brain pathology in the form of foci of low density.
The widespread use of HAART has led to an increase in the duration of the disease and made it more favorable - chronic forms of meningoencephalitis are more often observed than acute and subacute ones [15].
In 20% of HIV-infected patients, HIV-associated myelopathy often develops with severe immunodeficiency .
It can develop without the accompanying cognitive and mental disorders characteristic of HIV encephalopathy. The clinical picture is dominated by gait disturbances due to increased muscle tone of the spastic type and ataxia of the limbs, hyperreflexia, pathological reflexes, pelvic disorders, in particular erectile dysfunction. Sensitivity may be impaired in a conductive or “socks” and “gloves” type due to concomitant polyneuropathy. Isolated HIV myelopathy can be diagnosed in cases where concomitant cognitive impairment is less pronounced than the symptoms of myelopathy, or is absent. In diagnosis, the main role is given to neuroimaging methods and electrophysiological studies; an increase in the latent period of somatosensory and motor evoked potentials during transcranial magnetic stimulation is revealed. Treatment is based on HAART.
HIV-infected patients at any stage of HIV infection may develop syndromes of damage to the peripheral nervous system, which are observed in approximately ½ of patients. The most common clinical conditions are polyneuro- and polyradiculopathies, which can develop as a result of both the direct effect of HIV and opportunistic infections.
Distal symmetric sensory polyneuropathy most often develops
. It usually occurs in the later stages of HIV infection, when the number of CD4 lymphocytes becomes less than 200 per μl. The risk of its development is higher in older patients, as well as those who use narcotic drugs [16]. The connection between peripheral nerve damage and the use of neurotoxic antiviral drugs is less convincing. The disease manifests itself as slowly increasing sensory disturbances - sensations of numbness, tingling, crawling on the feet and legs. Approximately 30-50% of patients develop neuropathic pain syndrome with burning, cutting or stabbing pain in the distal extremities. Upon examination, a decrease or absence of Achilles reflexes, an increase in the threshold of vibration sensitivity on the toes, feet, ankles and a decrease in pain sensitivity in the distal extremities are revealed; proprioceptive sensitivity, as a rule, is not impaired. Weakness and atrophy of the foot muscles are mild. Hands and fingers are rarely affected. In many patients with distal symmetric sensory polyneuropathy, loss or dysfunction of small sympathetic and parasympathetic nerve fibers can cause orthostatic hypotension and erectile dysfunction. The diagnosis uses electroneuromyography, which reveals the axonal type of damage to nerve fibers.
Acute and chronic inflammatory demyelinating polyneuropathy (AIRDP and CIDP) also occur in HIV infection.
. AIDP usually develops during seroconversion or during the asymptomatic stage of HIV infection, and can rarely occur during recovery of the immune system. It occurs as Guillain-Barré syndrome. The CSF of HIV-infected patients (as opposed to HIV-negative patients) often shows mild pleocytosis. Approximately 1/3 of patients experience residual effects of varying severity.
CIDP is a chronic progressive and relapsing disease characterized by the development over several months of flaccid paresis and neuritic sensory disturbances. In some cases, relapses alternate with incomplete remissions and periods of stabilization. In CIDP, as in ARDP, protein levels in the CSF increase and mild pleocytosis is often detected. CIDP is a rare complication of HIV infection and usually develops soon after seroconversion or in the early stages of HIV infection.
Toxic drug-induced neuropathies occupy an important place among secondary lesions of the nervous system during HIV infection.
related to the prescription of antiretroviral, antimicrobial, cytostatic drugs. Approximately 10% to 30% of patients receiving didanosine, stavudine, or zalcitabine develop distal symmetric sensory polyneuropathy, which is clinically and electrophysiologically indistinguishable from polyneuropathy due to HIV infection. The only difference is a history of taking neurotoxic nucleoside reverse transcriptase inhibitors (NRTIs). Nucleoside neuropathy develops on average 12-24 months from the start of taking the drug. After its withdrawal, the condition sometimes continues to worsen for 2-4 weeks, but after 1.5-3 months it usually begins to improve. Sometimes recovery is incomplete due to the initial damage to peripheral nerve fibers caused by HIV neuropathy. With subclinical dysfunction of peripheral nerves, confirmed by electroneurography, the risk of developing neuropathy while taking NRTIs increases.
Polyneuro- and polyradiculopathies in the later stages of HIV infection can be a complication of opportunistic diseases. Multiple mononeuropathy in most cases is a complication of cytomegalovirus infection (CMV) and non-Hodgkin's lymphoma. Acute and subacute polyradiculopathy, in particular cauda equina syndrome with rapidly progressive flaccid lower paraparesis, fecal incontinence and sensory disturbances, can be caused by opportunistic infections, as well as tumor infiltration of the meninges in lymphoma. Other causes of polyneuropathy are chronic alcoholism, diabetes mellitus, exhaustion due to chronic diseases of the gastrointestinal tract, and neoplasms.
Diagnosis of neuropathies in HIV infection is usually based on anamnesis and clinical examination. To confirm the diagnosis and exclude other diseases, electroneurography is necessary. If opportunistic infections are suspected, a CSF examination is required. Sural nerve and muscle biopsy is only required in atypical cases, such as painful distal symmetric sensory ponyneuropathy in a patient with a high CD4 cell count and low viral load who is not taking neurotoxic drugs and in the absence of other risk factors. Sometimes, if there are patient complaints, an objective examination, including electrophysiological examination, does not reveal any changes. In this case, symptoms may be due to isolated neuropathy of small unmyelinated autonomic nerve fibers. To clarify the diagnosis, a puncture biopsy of the peripheral nerve with histological assessment of the density of intraepidermal nerve fibers or recording of pain-related somatosensory evoked potentials is required.
The main causes of secondary lesions of the central nervous system during HIV infection are opportunistic infections and neoplasms that develop in the later stages of HIV infection, in the stage of AIDS. Many of them often lead to the death of the patient. Toxoplasmosis is the most common cause of focal damage to the central nervous system in patients with AIDS (detected in approximately 10% of patients). In most cases it is the result of reactivation of a latent infection. Neuroimaging techniques play a crucial role in the diagnosis of toxoplasmosis. Neuroimaging reveals areas of damage to the brain substance with edema, more intense staining with intravenous contrast, often in the form of rings. Lesions are usually found in the basal ganglia. CNS toxoplasmosis in patients with AIDS often recurs after cessation of treatment, so most patients require ongoing maintenance therapy [17, 18].
Primary CNS lymphoma is detected in 5% of AIDS patients. Neurological symptoms may indicate focal or diffuse central nervous system damage. Such patients have a high titer of antibodies to the Epstein-Barr virus. When using neuroimaging methods, one (or more) hyper- or isodense lesion with signs of edema of the brain substance is identified, but the changes are not specific for lymphoma [19].
Herpesvirus complications of AIDS include damage to the central nervous system by cytomegalovirus, Herpes
zoster
, herpes simplex types 1 and 2. They can cause damage to both the brain substance and its membranes. Herpes zoster usually results from reactivation of a latent infection and occurs at different stages of HIV infection. Patients with AIDS more often have disseminated herpes and postherpetic neurological syndrome, as well as multifocal leukoencephalitis with focal or lateralized neurological symptoms and signs of hydrocephalus [20].
Tuberculosis, syphilis, and fungal infections also often lead to infectious damage to the brain and its membranes in patients with AIDS. Infectious lesions of the central nervous system are usually observed in patients with late stages of AIDS [21]. The diagnosis of these diseases is determined by the characteristics of each of them, but the infection is often verified only retrospectively, in particular in response to specific therapy. Suspicion may arise from the analysis of clinical symptoms, neuroimaging examination data, and, less commonly, from serological studies or biopsy data. There is often a co-infection with several pathogens.
Thus, neurological disorders in HIV infection are very diverse, in some cases they are the first symptoms of HIV infection and can serve as a reason for prescribing HAART.
What is HIV encephalopathy?
HIV is a virus that attacks and weakens the immune system, which can increase the risk and impact of potential complications. One such complication is HIV encephalopathy. This usually occurs due to the effects of a virus or opportunistic infections such as toxoplasmosis on the brain.
HIV encephalopathy usually appears when HIV reaches its final stages, so it can appear many years after infection. This condition is more common in people who are not taking effective HIV medications and those who have very low counts of CD4 cells, a type of white blood cell that fights infections. HIV encephalopathy is less common in people who receive early and ongoing treatment.
HIV encephalopathy - diagnosis
Diagnosing HIV encephalopathy is difficult because many factors can contribute to symptoms. These include:
- nutritional deficiency
- depression
- side effects of medications
- opportunistic infections
Doctors may use the following diagnostic tests to make a diagnosis:
- mental status tests
- neuropsychological testing
- basic tests of physical ability or movement
- MRI scan
- CT scan
- blood tests
- cerebrospinal fluid tests
Treatment of HIV encephalopathy
Without treatment, HIV encephalopathy can be fatal. Evidence suggests that no specific treatment can cure all complications of HIV encephalopathy. People may need different medications, such as opioids, anticonvulsants, antidepressants, and antiretroviral therapy, to treat different symptoms.
Antiretroviral therapy is the main treatment for HIV. This is a combination of drugs that reduces the amount of virus in the blood. Research suggests that drugs can reverse some of the damage that occurs as a result of HIV encephalopathy, potentially improving scores on tests that measure thinking skills.
An article published in 2021 describes antiretroviral therapy as the most effective treatment for HIV encephalopathy, noting that treatment reduces the prevalence of severe cases. Treatment effects:
- reversing some brain damage from HIV
- improved results of neuropsychological and cognitive tests
- delaying the onset of symptoms indicating brain damage
However, the effectiveness of antiretroviral therapy for milder forms of HIV-associated cognitive decline is unclear. The lack of evidence is due to the fact that cognitive difficulties in such cases are minor, so they sometimes go undiagnosed.
HIV encephalopathy - causes
Researchers still do not understand exactly the mechanism that causes the development of HIV encephalopathy. However, most evidence suggests that it is due to inflammation and damage that occurs when the virus crosses the blood-brain barrier and infects the brain. Some evidence also suggests that HIV can mutate in the brain, making it different from the virus circulating in the rest of the body. This may cause some treatments to be less effective.
HIV encephalopathy by stages
The World Health Organization (WHO) lists HIV encephalopathy as a symptom of the final stage of HIV.
It is also the most severe of the three stages of HIV-associated neurocognitive disorder:
- Asymptomatic neurocognitive impairment
: This form has no symptoms of cognitive decline. - HIV-associated mild neurocognitive disorder
: Mild symptoms of cognitive impairment may occur. - HIV encephalopathy
: presents with severe symptoms of cognitive decline.