Home | About us | Delivery | Advertisers | Login | Registration
Delivery on Sundays and holidays does not work!
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2021 Pharmacy 84.
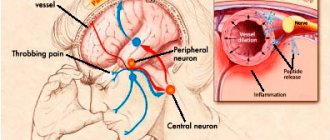
Perception and control of the orientation and movement of the body in space are provided by the integrative function of the central nervous system, which involves receiving information from three sources - the visual analyzer, the vestibular organ in the inner ear and sensors in the muscles, ligaments and skin, which provide proprioceptive information about body movements and physical contacts with the environment. Failure of any component of this system can cause discomfort, dizziness and unsteadiness, which in turn can lead to work-related accidents and personal injuries due to falls.
Every year, falls occur in 30% of people over 65 years of age, and among people over 75 years of age this percentage is even higher, with 20–30% of those who fall receiving injuries that reduce their mobility and independence and increase the risk of premature death.
The increase in postural instability in older people is likely due to the fact that at this age there are noticeable changes in the physiological mechanisms that provide motor function and coordination. As is known, from 50 to 70% of all falls in elderly and senile people occur while walking [1].
Among the various causes of balance disorders in old and senile age, pathology of the peripheral vestibular apparatus and central mechanisms of balance against the background of vascular diseases of the brain dominates. Foreign literature also contains data on the connection between sleep disturbances and excessive daytime sleepiness and balance indicators. All studies have proven the negative impact of sleep disorders on postural control and adaptation among young volunteers [2–4].
Since aging weakens compensatory mechanisms for maintaining balance, it can be assumed that sleep disturbance has a greater destabilizing effect on postural control in older people compared to younger people [5].
Sleeping pills are the most commonly prescribed medications for the treatment of sleep disorders in old age. Numerous studies have shown the negative effects of sleeping pills on balance.
One study examined the effect of zolpidem on postural function in inpatients. Impaired postural control in elderly patients has been demonstrated while taking the drug. Studies have also shown that when zolpidem was used to treat insomnia, the side effects of balance were not significantly different from those of other drugs such as opioids, antidepressants, antipsychotics, benzodiazepines and antihistamines [6].
Thus, on the one hand, the disturbance of night sleep that develops during insomnia is accompanied by a deterioration in balance function, especially in people of older age groups. On the other hand, the use of sleeping pills to improve night sleep can also compromise the system of regulation of stability and walking, and increases the risk of imbalance due to side effects. Where is the “sweet spot” where we can use sleep medications to improve sleep in older adults without the risk of increasing the risk of falls? We have a number of our own observations of elderly patients with insomnia, where the benefits of improved sleep outweighed the potential danger of deterioration of balance while taking a modern sleeping pill, which was proven instrumentally.
Clinical case
Patient N., 64 years old, complained of falling asleep for a long time in the evening after going to bed; frequent awakenings at night; prolonged falling asleep after waking up at night; early awakening, after which I could not fall asleep; periodically complete lack of sleep at night; feeling of general weakness in the afternoon; constant feeling of dizziness and unsteadiness when walking; pressing headache in the occipital region; deterioration of memory and attention, which is associated with sleep disorders; anxiety, decreased mood. The frequency of sleep disturbances is 3–4 times a week.
From the medical history: the above-described manifestations have been troubling since 2010 after suffering a stressful situation associated with a high work load and problems in family life. Periodically she took sleeping pills of herbal origin (she doesn’t remember the names) without a significant positive effect. No sleep examination was performed. No family member was known to have sleep problems.
From the life history: in childhood, she did not lag behind her peers in development. Past diseases: acute respiratory viral infections. She was vaccinated according to the vaccination calendar. There were no surgical interventions. Denies chronic diseases. Denies bad habits. Lives with family. Living conditions are satisfactory. Works as an accountant. There is no allergic history.
Somatic status: hypersthenic build, height – 165 cm, weight – 80.6 kg, body mass index – 29.4 kg/m2.
Blood pressure – 120/80 mm Hg. Heart rate – 75 beats per minute.
The neurological status reveals a mild ataxic syndrome, manifested by instability in the Romberg test.
Somnological status: goes to bed at 23.00 in the evening, gets up at 7.00 on weekdays and weekends. Falling asleep takes 1–2 hours every evening. Night awakenings occur 2-3 times per night. After night awakenings, it takes up to 30 minutes to fall asleep almost every night. Periodically (1–2 times a month) there is a complete lack of night sleep. Subjective sleep duration: about 5 hours.
Questionnaire data:
- Epworth sleepiness scale: 10 points (norm is no more than 9 points) [7].
- Insomnia severity index (ISI): 19 points (moderate sleep disturbances) [8].
- Pittsburgh Sleep Quality Index (PIQS): 16 points (more than 5 points are considered evidence of poor sleep quality) [9].
- Berlin Apnea Questionnaire: 2 points (normal <2) [10].
- Spielberger Situational Anxiety Inventory: 38 points (norm <30) [11].
- Spielberger Personal Anxiety Questionnaire: 47 points (norm <30) [11].
- Beck Depression Inventory: 9 points (normal <10) [12].
- Dementia rating scale: 0 points (normal) [13].
- Montreal Cognitive Function Rating Scale: 30 points (normal) [13].
According to the questionnaires, the patient has severe sleep disorders and affective disorders in the form of increased anxiety.
Actigraphy: to objectify sleep disorders, motor activity was recorded with a wristwatch-shaped sensor attached to the wrist for two days. The SOMNOwatchtm device (SOMNOmedics, Germany) and DOMINO light software (version 1.4.0) were used. The following indicators were determined: time of falling asleep and time of the sleep period, time of wakefulness during sleep and sleep efficiency.
According to the study, the time to fall asleep was 57 minutes (the norm is less than 30 minutes), the sleep period was 7.1 hours. Sleep time – 6.2 hours. Wakefulness during sleep is 55 minutes (norm <30 minutes), sleep efficiency is 86.9% (norm ≥85%).
A neurovestibular study performed using the Halmagi, Unterberger, and Dix-Hallpike tests revealed no signs of pathology of the peripheral vestibular apparatus.
Posturography: balance indicators were assessed using a computerized posturography platform with biofeedback (stabiloplatform ST-150 “Biomera”, Russia). The study was conducted in the morning two hours after waking up. The stabilographic study included the Romberg test, in which the patient stood on a platform for 30 seconds with her eyes open and then with her eyes closed. When performing the test, the patient stood with support on two legs (heels together, toes slightly apart) with her arms down. The length and area of the statokinesiogram, as well as the speed of movement of the center of pressure were assessed (see figure).
According to the study: the length of the statokinesiogram with open eyes was 564.7 mm, with eyes closed – 737.5 mm. The area of the statokinesiogram with open eyes is 599.6, with closed eyes – 897.9 mm2. The speed of movement of the center of pressure: with open eyes – 18.8, with closed – 24.6 mm/s.
Thus, clinical and instrumental examinations showed that the patient had signs of chronic insomnia according to the criteria of the 3rd version of the International Classification of Sleep Disorders 2014 [14].
Firstly, she complains of disrupted night sleep in the form of an increase in the time it takes to fall asleep, frequent night and early morning awakenings. These complaints are confirmed by data from an objective study - actigraphy, which revealed an increase in the time of falling asleep and the time of wakefulness within sleep. Secondly, she has sufficient conditions and time for sleep. Thirdly, the patient’s sleep disorders lead to disturbances in activity during daytime wakefulness. Thus, she notes a feeling of general weakness and drowsiness in the afternoon, deterioration of memory and attention. She experiences sleep disturbances 3–4 times a week, which also meets the quantitative criteria for insomnia. Sleep disorders continue for more than 3 months, which meets the criteria for a chronic course of the disease.
Based on these criteria, the patient was given a clinical diagnosis of chronic insomnia.
As part of the treatment of sleep disorders, first of all, a conversation was held with the patient about the rules of sleep organization (sleep hygiene) and the reasons for her development of insomnia.
The main treatment method was zopiclone Somnol® (Grindeks JSC, Latvia) at a dose of 7.5 mg for 10 days, 40 minutes before bedtime. The choice of a sleeping pill is determined by the fact that it is the representatives of this group (the so-called Z-drugs) that have the greatest evidence base regarding the effectiveness of treating insomnia. Zopiclone has a selective effect on the α1 subunit of the GABAA receptor complex, which determines its hypnotic effect. In addition, among the drugs of this group, zopiclone has a fairly high level of agonism with other components of the GABAAergic complex - α2-, α3- and, possibly, α5-subunits, which are responsible for the anxiolytic effect of the ligands of this receptor, which can positively affect the level of anxiety on the part of this patient, which turned out to be elevated [15]. The half-life of the drug is about 5 hours, in this case this was important, since the patient had difficulty falling asleep not only after going to bed in the evening, but also after waking up at night, and there was also a problem with early morning awakening. The relatively long half-life made it possible to provide a hypnotic effect throughout the entire night's sleep.
The effectiveness of treatment was assessed during a repeat examination, which took place 10 days later.
During a conversation with the patient, an improvement in subjective feelings of sleep was noted in the form of a reduction in the time of falling asleep, night awakenings and an increase in sleep duration.
According to the questionnaire, there was also a pronounced decrease in the severity of insomnia manifestations: according to the results of ITI (from 19 to 14 points) and PICS (from 16 to 12 points). Treatment with zopiclone was also accompanied by a decrease in anxiety levels on the Spielberger Situational Anxiety Scale (from 38 to 35 points).
When repeating the balance study, it was found that, against the background of improved sleep indicators, the patient had an improvement in all posturographic indicators (see figure and table). Thus, the length of the statokinesiogram with open eyes during treatment decreased by 43%, the area of the statokinesiogram with open eyes - by 40%, and the speed of movement of the center of pressure with open eyes - by 60%. The patient herself, along with improved sleep, noted improved stability when walking.
The patient was recommended to continue taking Somnol at a dose of 7.5 mg and follow the rules of sleep hygiene.
Discussion
The clinical case we presented of improving balance indicators against the background of correction of insomnia disorders allows us to discuss several important issues for clinical somnology and gerontology.
The first is: how dangerous is the use of modern sleeping pills in relation to balance in older people? Indeed, in the early era of hypnotic use, an increase in the incidence of incoordination was documented with the use of long-lived GABAA receptor agonists such as barbituric acid and benzodiazepine derivatives. Thus, H. Javelot et al. (2018) showed that when using benzodiazepines in older people, there was a significant increase in the risk of falls [16]. Studies of the effects of selective GABAA receptor agonists (Z-drugs) on balance have also demonstrated impaired postural control in this group of patients. Thus, in a study by M. Mets et al. (2010) Z-drugs (zopiclone, zolpidem, zaleplon) had the same negative effect on the balance of the elderly as benzodiazepine hypnotics (nitrazepam, triazolam, lorazepam, temazepam, loprazolam) [17].
The second question is: to what extent can sleep disturbances themselves worsen balance? In a study by Y. Morad et al. (2007) examined the ability to detect fatigue after sleep deprivation by assessing stabilometric parameters. The researchers found a significant deterioration in postural control with sleep restriction. The authors believe that the use of posturography for excessive daytime sleepiness may be a promising screening method for diagnosing fatigue [2].
Similar results were obtained in a study by J. Ma et al. (2009). The purpose of the work was to determine the early stages of fatigue using posturography. The authors examined volunteers whose average age was 20.7 years before and after 24-hour sleep deprivation. The results showed that posturographic scores after sleep deprivation were significantly worse than the results obtained before [4].
It can be assumed that improved sleep may be accompanied by improved balance scores. The most common sleep disorder, especially in old age, is chronic insomnia. There is no data in the literature on the effect of sleep disorders on the stabilometric indicators of the elderly, as well as on changes in balance indicators against the background of improved sleep with successful correction of insomnia.
Cognitive behavioral therapy (CBT-I) is recognized as the method of choice in the treatment of chronic insomnia, and it would be logical to start treating our patient with it.
CBT-I involves discussing sleep hygiene with the patient, identifying dysfunctional sleep beliefs, and discussing and applying techniques to limit external stimulation to improve sleep. The CBT-I course usually includes six sessions with the patient once a week and is conducted by a certified specialist. In Russia, unfortunately, there are only a few specialists, most often psychotherapists who know this method, and for us at that time they turned out to be inaccessible.
In this regard, to treat sleep disorders in this patient, we used another approach, which also has a significant evidence base: treatment with the Z-group hypnotic drug zopiclone. The use of Somnol for 10 days was accompanied by an improvement in sleep quality and stabilometric indicators.
Since initially one of the patient’s leading complaints was a constant feeling of dizziness and instability when walking, a preliminary study included a neurovestibular examination and posturography. No dysfunction of the peripheral vestibular apparatus was identified. According to stabilography, signs of postural instability were established, caused by weakening control of maintaining balance at the level of frontal-subcortical-stem interactions and emotional-affective disorders.
Successful correction of sleep disturbance was confirmed using the ITI and PICS scales. Against this background, we also observed an improvement in balance indicators - length, area of the statokinesiogram and the speed of movement of the center of pressure with open and closed eyes. We assume that this effect is due to an improvement in cortical-subcortical-stem interactions against the background of a decrease in the severity of insomnia, as well as a positive effect on the emotional sphere.
In this case, there was no possible negative effect of the drug Somnol on balance, which could be expected based on the literature data. This may be due to the fact that zopiclone itself does not have such a negative effect or the effect of normalizing sleep exceeded the negative effect of the drug. The additional anxiolytic effect of zopiclone, which distinguishes it from other Z-drugs, should also be taken into account. However, often an increased level of anxiety can be accompanied by an increase in the tension of postural control and a decrease in the area of the statokinesiogram, while the length of the statokinesiogram increases or remains within normal values [18].
Conclusion
Of course, one or even a few clinical observations is not enough to prove the positive impact of improving sleep in older people on their postural functions. This requires controlled clinical studies using more accurate quantitative methods for assessing sleep status (polysomnography). Nevertheless, our clinical experience allows us to assert that in many cases, refusal to use sleeping pills in older people is not justified, and in each individual case the doctor should independently weigh the risks and benefits of prescribing such treatment, in particular when using zopiclone drugs.
Indications
The instructions indicate that zopiclone tablets help with non-organic insomnia. This means that the use of the drug is justified for insomnia caused by stress, neuroses, fatigue, physical discomfort, changes in normal lifestyle (the need to spend the night in an unfamiliar place, hospitalization, business trip).
Sometimes the drug is taken for chronic insomnia, but only as a temporary measure. It eliminates insomnia while the effects of the main treatment have not yet occurred. For example, antidepressants or psychotherapy usually begin to work within 2-3 weeks of use. But while waiting for the effect, the patient needs to sleep somehow! Zopiclone helps ensure this.
Action
The medicine has a fairly strong hypnotic and sedative effect. This happens because it enhances the effect of gamma-aminobutyric acid, the so-called inhibitory transmitter, on nerve cells. Signal transmission between nerve cells slows down.
Express test:
Assess how you feel during the day to determine the severity of your sleep problems
In general, this mechanism is somewhat reminiscent of the action of phenazepam - which is known to be a very strong brain suppressant. The difference is that zopiclone acts more selectively, practically does not affect the respiratory center and inhibits only those structures that are responsible for sleep and wakefulness.
The pills affect sleep as follows:
Shortens the period of falling asleep by an average of 40-50%;
Reduce the number of night awakenings;
Makes sleep better quality, bringing a feeling of vigor;
Unlike “old” sleeping pills, zopiclone does not change the stage of sleep, so sleep after taking it is as close to natural as possible.
Special instructions for the use of Zopiclone
The use of zopiclone should be avoided during pregnancy and breastfeeding. Patients taking zopiclone should refrain from performing potentially hazardous activities that require increased alertness. Abrupt cessation of treatment does not cause the development of withdrawal syndrome. During treatment, you should avoid drinking alcohol and taking depressant psychotropic drugs. In cases of use of zopiclone for myasthenia gravis, strict neurological monitoring must be ensured due to the possible increase in muscle weakness.