Neurologist
SEMENOVA
Olga
5 years experience
neurologist, head of the office for diagnostics and treatment of cognitive disorders
Make an appointment
A disease in which a person experiences a decrease in verbal and logical thinking and other speech perception disorders are manifested is called sensory aphasia. Unlike other forms, sensory is considered mild; the patient is not able to perceive individual words and short phrases in all cases. A person with this type of disorder hears, but not as expected; words sound as if they are in another language. Against this background, anxiety intensifies, and disorientation in space is possible.
Kinds
Depending on which brain area is affected, the following forms of aphasia are distinguished:
- Motor aphasia is associated with damage to Broca's area (lower parts of the premotor area of the left hemisphere). The pronunciation of words is impaired, although the ability to reproduce sounds and understand speech is preserved;
- Sensory aphasia affects Wernicke's center, which is located in the temporal lobe. In this case, the patient loses the ability to understand speech, while maintaining conversational function;
- Semantic aphasia is characterized by disruption of the parieto-temporo-occipital region. The ability to perceive complex word combinations connected by prepositions or conjunctions is lost;
- Amnestic aphasia - occurs due to damage to the parietotemporal zone. The patient understands speech, but cannot remember the name of some objects;
- Total aphasia is a complete loss of the ability to understand and reproduce speech.
How does sensory aphasia occur?
The reasons for the loss of the ability to speak connectedly lie in damage to the cortex of the temporal lobe of the brain. This may be a consequence:
- traumatic brain injuries;
- epilepsy;
- cerebral aneurysms;
- tumors;
- infections - encephalitis, meningitis and other diseases affecting the brain and its membranes;
- abscesses that arise as complications of otitis media or for other reasons;
- severe diseases accompanied by neurodegeneration or demyelination of nerve fibers;
- stroke.
The last two causes are extremely rare in children, but, unfortunately, they cannot be completely excluded.
Diagnostics
A neurologist diagnoses and treats aphasia.
- Initially, complaints and medical history are collected
- This is followed by a general neurological examination for the presence of external neurological abnormalities (drooping of the corner of the lips, deviation of the tongue when protruding, decreased tone of the limbs, etc.).
Additional diagnostic methods are prescribed:
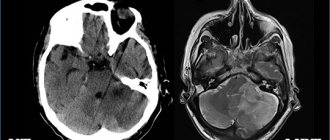
- Computed tomography and magnetic resonance imaging - help to establish the cause of the disorder through layer-by-layer examination of brain tissue;
- Electroencephalography – determines electrical activity in various parts of the brain;
- Magnetic resonance angiography is performed if there is a suspicion of vascular obstruction.
Bringing speech back
Correction of sensory aphasia primarily includes drug support - continued treatment of the disease that led to the speech disorder. The primary treating physician for such patients is a neurologist. Its task is not only to monitor the continuation of treatment, but also to monitor whether other neurological disorders develop, which may either be a consequence of a previous illness or injury, or arise for other reasons. The doctor decides which medications are used individually in each case. If you want to add something to your treatment (most often you want to add vitamins), be sure to discuss this with your doctor! Accurate implementation of the neurologist’s prescriptions is the basis for success in speech rehabilitation.
An important component of treating sensory aphasia is working with a speech therapist. It happens, especially in children, that speech is restored on its own, but no one can predict whether this will happen or not. Therefore, remedial training for sensory aphasia is an essential part of therapy. The speech therapist will teach parents what exercises to do at home and what to watch for so that rehabilitation goes faster and more successfully. The main task of relatives is to organize a comfortable environment for the patient and learn to communicate with him. The exercises that the speech therapist asks you to do at home will help with this. Don’t force things, the brain needs time to restore neural connections. It is extremely important to dose the load; overwork will not benefit the baby.
Our center’s specialists have extensive experience in restoring lost speech in children. They are familiar with methods that are recognized as effective by the global speech therapy community, and choose from a variety of methods those that will work best for a particular child. We achieve results whenever this is possible in principle - and in children it is possible to restore lost speech in most cases.
Treatment
Treatment of aphasia takes place in two stages. At the first stage, several options are possible:
- Surgical removal of tumors, hemorrhages, restoration of vascular patency;
- Drug treatment with antibacterial drugs, nootropics, angioprotectors;
- Rehabilitation therapy using exercise therapy and physiotherapy.
The second stage of treatment for the disease is sessions with a speech therapist. With its help, individual exercises are selected to correct speech function.
At the medical clinic, you can undergo aphasia treatment from a neurologist. Using modern equipment, our specialists will conduct a comprehensive examination, and then develop basic methods of treating the disease, with the help of which speech function will be restored. You can get detailed information and make an appointment at the reception or by phone.
How does sensory aphasia occur in childhood?
Sensory aphasia in children occurs quickly, but after eliminating the factor that damaged the brain, speech is also quickly restored, because it is easy for the child’s brain to develop new connections to replace the lost ones. It is worse if speech has not been restored several weeks after the event that led to its loss. In this case, the forecast becomes worse.
When diagnosing children, it is easy to confuse aphasia (loss of speech skills) with alalia (their immaturity). Anamnesis will help to distinguish between the conditions: were there any traumatic factors at what stage of the child’s development before them?
The procedure for correcting motor aphasia
Speech therapy correction of aphasia includes:
- practicing articular differentiations;
- classes aimed at improving pronunciation;
- development of vocabulary, classes to improve speech understanding;
- correction of speech coherence;
- getting rid of speech and writing defects.
For aphasia correction to be successful, it is important to develop auditory analysis skills from the very beginning. The child should be able to easily identify the necessary sounds and determine the positions in which they are located. The main task of correction is to revive the speech analyzer. Therefore, first of all, a speech therapist works with preserved sounds.
The next step is to restore the missing sounds. The acoustic, articular and graphic components of each sound are carefully studied. Classes are very useful, the essence of which is the combined (together with a speech therapist) repetition of speech series, for example, BA-PA, PA-BA, etc.
Later, as classes progress, words and phrases are formed from syllables. If the patient is already in school, then the aphasia correction course additionally includes exercises to improve writing skills, the entire oral cycle is repeated in writing. During written speech correction, each word is analyzed, broken down into sounds and letters, and exercises are given. For example, a child needs to find and restore a missing letter, answer a question in writing, complete a word, etc.
Motor aphasia
Motor aphasia is the most common. It occurs when Broca's speech motor center is damaged.
This form is characterized by complete or partial loss of the ability to speak.
A person with motor aphasia understands speech well. However, he cannot pronounce complex words and link them correctly into sentences. Most motor aphasics manage to pronounce random syllables and fragments of sentences. Usually the most frequently used words are saved. The patient is able to pronounce individual syllables and simple sentences; often inserted words appear in speech, for example “here”, “this”. A similar disorder is also known as embolphrasia (embolus - insertion, phrases - speech).
Most people with motor aphasia are not capable of spontaneous speech. As a result of damage to Broca's speech center, the trigger mechanism is disrupted and the person loses the ability to reproduce sounds, construct syllables, and words. But at the same time, most patients understand speech well.
Children with motor aphasia, as a rule, do not lose the ability to distinguish numbers and letters, and can add various words, their first name, and last name from a cut alphabet. Such children are aware of their problem and are usually very worried about it. Such children are very self-critical and aware of their own helplessness. They develop depression, which can worsen if the child is not understood.
Disinhibition of speech at the initial stages of aphasia development
The most effective method of eliminating aphasia and preventing the problem from worsening is to bring speech sequences to an automatic level by performing exercises such as singing, repeating phrases, finishing sentences, tongue twisters, etc.
When disinhibiting, the speech therapist completely pronounces the sentence to the last word, pronouncing only one syllable. The patient’s task is to finish the last word. First, the speech therapist examines the patient, determines what is easier for the patient, verbs, nouns, adjectives.
For example: the goat bleats, and the dog ... (barks); grass in the yard, firewood on the grass); Summer, sun, ... (heat); take matches, light... (fire).
Also, when disinhibiting, it is possible to achieve very good results using sayings. For example: you can’t even pull a fish out of ... (pond) without difficulty.
If such exercises cause difficulties for the patient, and more often than not, the song helps. The speech therapist begins to sing and when the patient begins to recognize the song, a smile spreads across his face.
Post-stroke aphasia: clinical picture, differential diagnosis, treatment
Speech disturbances are a common symptom of stroke (15–38%). They often lead to permanent disability, significantly complicate rehabilitation during the recovery period, reduce the quality of life of both the patients themselves and those around them, cause negative psycho-emotional reactions, and increase the economic costs of treatment. Compared to patients with stroke but without speech disorders, patients with post-stroke aphasia have a higher mortality rate and stay in hospital longer. Predictors of good recovery of speech function are mild to moderate severity of speech disorders in the acute period of stroke, the amount of brain damage (the smaller the ischemic focus, the higher the chances of recovery), young age, high Barthel index, and high level of education. In addition to the treatment of the underlying vascular disease, patients with speech disorders need systematic speech therapy sessions and medications in order to optimize cerebral neuroreparative processes.
Table. Types of aphasia
Aphasia is a disorder of a person’s higher mental functions, which consists of a loss or decrease in the ability to verbally communicate, including constructing one’s own speech utterance and/or understanding spoken speech. As a rule, patients with aphasia have pathology in both oral and written speech (reading, writing), and also have difficulties in using sign language and Braille (a dotted font for writing and reading for the blind).
Neuroanatomy of aphasia
Speech areas are a complex neurocognitive network located in the dominant hemisphere. In approximately 95% of people, the left hemisphere is dominant in speech, and in 5% of cases, either both hemispheres are involved in the innervation of speech, or the right hemisphere becomes dominant. Already at birth, in more than half of newborns, the cortex in Wernicke’s area and the angular gyrus in the left hemisphere is approximately 50% larger in volume than in the right [1]. If for some reason in very early childhood the left speech areas suffer, then the right hemisphere of the brain acquires signs of dominance [1].
Speech centers include the posterior parts of the left frontal lobe (Broca's area) and the left superior temporal gyrus (Wernicke's area), as well as connections between these areas. The motor program for speech utterance is formed in Broca's area. Broca's area projects directly to the neurons of the precentral gyrus, which innervate the muscles of the larynx and oral cavity. Wernicke's area is responsible for comparing auditory information with visual and kinesthetic images, which is necessary for understanding spoken speech. Comparison of information is provided by connections between Wernicke's area and the occipital and parietal cortex. Another cerebral region important for speech is the angular gyrus in the inferior parietal lobule, which is responsible for the perception of written speech and sign language.
In addition to the classical speech centers, other areas of the brain also play an important role in the formation of speech. These include the insula (important for articulation), zones of the frontal and temporal lobe (processing sentences), as well as zones of the occipital and parietal cortex of the brain (responsible for memory for the meanings of words) [2–5].
The subcortical nuclei of the brain also make a significant contribution to maintaining normal speech function. Diffusion-weighted and perfusion-weighted magnetic resonance imaging (MRI) of the brain in patients with ischemic damage to the basal ganglia and aphasia showed a secondary decrease in perfusion in the subcortical gray ganglia. However, the prognosis for subcortical aphasia is more favorable than for cortical damage [6]. In recent years, the role of cerebellar damage has also been actively discussed, since it can also lead to dysphasic disorders in the form of disturbances in the grammatical structure of speech [7].
Etiology of aphasia
The most common cause of aphasia is ischemic stroke. Less commonly, speech disorders are observed with hemorrhagic strokes, space-occupying brain lesions, infectious lesions (abscess, encephalitis), and traumatic brain injury. Rare cases of the development of aphasia in demyelinating diseases have been described [8, 9].
Transient aphasia can be observed with transient ischemic attacks, epilepsy, migraine. The presence of aphasia during a transient ischemic attack is one of the high risk factors for developing stroke in the coming days and weeks [10].
Gradually progressive aphasia may also be a manifestation of a neurodegenerative disease. Most often, gradually progressive aphasia is associated with frontotemporal degeneration, less often with Alzheimer's disease or other dementing diseases. Moreover, in some cases, the clinical picture does not show any other cognitive and/or behavioral disorders for many years (the so-called primary progressive aphasia) [11–13].
Speech status study
To diagnose and analyze the characteristics of dysphasia, it is necessary to carefully listen to the patient’s speech, examine the understanding of spoken speech, reading and writing. You should pay attention to the number of words spoken per minute (speech fluency), unmotivated repetitions of individual words and phrases (perseverations), shortened phrases (less than five words), errors in the grammatical construction of statements (case endings, prepositions, conjunctions, word order in a sentence etc.) and/or difficulties in understanding grammatical structures. In addition, it is necessary to assess the ability to control the movements of articulatory muscles (speech praxis). To do this, you can ask the patient to repeat the phrase “artillery brigade” several times.
An important part of speech research is the assessment of its nominative function.
. The patient is shown certain objects and asked to name them, starting with familiar ones (for example, a spoon, pen, mug) and moving on to unusual ones (for example, a phonendoscope). Insufficiency of the nominative function of speech is noted in many aphasias, sometimes becoming one of the main manifestations of dysphasia.
Assessing oral language comprehension
is carried out by checking the execution of verbal commands, first simple and then complex (“close your eyes”, “show me two fingers”, “touch your left ear with your right hand”). We can then move on to explore understanding of more complex grammatical structures (“Are my brother’s father and my father’s brother the same person?” or “Is my aunt’s uncle a man or a woman?”). Final trials may reveal a lack of understanding, including in those who have followed simple verbal commands.
When checking the reading function
the patient is asked to read aloud a paragraph from a newspaper or magazine, assessing the correct pronunciation of the words. Comprehension of written language can be tested using written commands (eg, “take this piece of paper, fold it in half and place it on the floor” or “close your eyes”).
Letter evaluation
– the patient is asked to write any sentence. You can also dictate any text to the patient or offer to write the names of objects drawn in the pictures.
The above methods make it possible to diagnose dysphasia without leaving the patient’s bedside, which is of great importance in the acute period of stroke. When diagnosing speech disorders in a patient, it is necessary to examine them in more detail, analyze quantitative and qualitative features, and also evaluate other higher brain functions: attention, memory, praxis, visual-spatial orientation, etc.
Epidemiology and types of aphasia
According to the literature, aphasia is a common symptom of stroke (15–38%). Typically, the clinical picture also includes other symptoms of damage to the dominant hemisphere (right-sided hemiparesis, hemihypesthesia, hemianopsia) [14]. Let's look at the main types of aphasia (table).
Broca's aphasia (motor aphasia)
characterized by a violation of the construction of one’s own speech utterance, as well as the repetition of phrases. The patient's speech is laconic, poorly articulated, and characterized by auditory and verbal perseverations. The letter is broken. Comprehension of addressed speech may be incomplete in the first few days after acute cerebrovascular accident, but then quickly recovers. Motor aphasia develops as a result of acute ischemic stroke in the anterior branches of the left middle cerebral artery and is often combined with hemiparesis and hemihypesthesia.
Wernicke–Kozhevnikov aphasia (sensory aphasia)
characterized primarily by impaired understanding of oral and written speech. The patient’s own speech, as a rule, maintains normal tempo and intonation, but is meaningless, as it contains numerous replacements of syllables and words with similar ones in sound, but meaningless in meaning (literal and verbal paraphasias), as well as new unusual words (neologisms). With significant severity of these disorders, speech production takes on the character of so-called verbal okroshka. However, many patients are not aware of their defect. Sensory aphasia develops when the upper parts of the temporal lobe and the lower parts of the parietal lobe are damaged as a result of a stroke in the territory of the left middle cerebral artery. It is often combined with right upper quadrant hemianopia.
Total sensorimotor aphasia
– a set of symptoms of motor and sensory aphasia. Develops as a result of extensive strokes in the left middle cerebral artery, usually combined with hemiparesis, hemihypesthesia and hemianopsia. Rarely, encephalitis and late manifestations of neurodegenerative processes can be the cause of total aphasia.
Dynamic aphasia (transcortical motor aphasia)
is largely reminiscent of Broca's motor aphasia. There is a violation of the initiation of speech activity, perseveration and grammatical errors occur, while the understanding of addressed speech does not suffer. The main difference between dynamic aphasia and motor aphasia is preserved repeated speech: the patient can repeat words and phrases after the doctor. Typically, dynamic aphasia develops with a heart attack in the territory of the left anterior cerebral artery.
Transcortical sensory aphasia
is characterized by a violation of the understanding of addressed speech, which resembles Wernicke–Kozhevnikov aphasia, but the severity of these disorders is somewhat lesser. The patients’ own speech is fluent, but lacks content, and verbal paraphasia may be observed. However, unlike Wernicke's aphasia, repeated speech is preserved in transcortical sensory aphasia. Patients may also read aloud, but without understanding the meaning of what they read. Transcortical sensory aphasia develops with damage to the temporo-occipital or temporo-parietal areas adjacent to Wernicke's area as a result of a stroke, and can be combined with hemianopsia.
Transcortical mixed aphasia
– patients have signs of transcortical motor and sensory aphasia, but the ability to repeat words and phrases after the doctor remains intact. Understanding of written and spoken language also deteriorates significantly. Occurs when there is damage in the anterior and posterior cerebral arteries during repeated cerebral embolisms, infarctions in areas of adjacent blood supply associated with systemic circulatory disorders, such as acute heart failure.
Amnestic aphasia
– patients with amnestic aphasia cannot name a word or object, but they can describe the meaning and functions of the object. Spontaneous speech is characterized by pauses, word substitutions, and paraphasias are possible. Repetition of words and understanding of oral speech are not impaired. Amnestic aphasia has been described with damage to various anatomical areas, including the basal temporal lobe, anterior temporal lobe, temporo-parieto-occipital junction, and inferior parietal lobe.
Alexia without agraphia
– patients can write, but not read. Understanding of oral speech is intact, spontaneous speech is not affected. It develops when the left occipital lobe and splenium of the corpus callosum are damaged during an ischemic stroke in the territory of the left posterior cerebral artery [15].
Differential diagnosis
In most cases, in patients with risk factors for stroke (in old age, in the presence of arterial hypertension, diabetes mellitus, hypercholesterolemia, concomitant cardiac pathology, atrial fibrillation, etc.) with the acute development of neurovascular syndrome, characteristic of damage to the middle and/or posterior cerebral artery dominant hemisphere, the diagnosis of ischemic stroke is not in doubt. Neuroimaging methods are used to verify the diagnosis.
Impaired understanding of speech and speaking, reminiscent of dysphasia, can develop with acute dysmetabolic encephalopathy (delirium)
. In this case, difficulties often arise in understanding the spoken speech; the patient does not follow commands. Grammatical errors and paraphasia appear in the patient’s own speech. Signs of a confused state of consciousness, the presence of hallucinations, tremors, psychomotor agitation and delirium help in diagnosis.
Akinetic mutism
develops when the medial frontal region is damaged. In such patients, there is an absence or extreme paucity of spontaneous speech, poor execution of commands, a decrease in motor reactions, and signs of catatonia (waxy flexibility).
Patients suffering from depression
, may avoid communicating with others. They do not look the doctor in the eyes, they lie with their faces turned away from the people around them. In this case, anamnesis collected from the patient’s relatives and/or loved ones plays an important role in the differential diagnosis.
If the patient has episodes of transient aphasia
The differential diagnosis is made between
transient ischemic attack and epilepsy
. 24-hour electroencephalographic monitoring, angiography of cerebral vessels, and duplex scanning of the brachiocephalic arteries are performed.
Aphasias with gradual onset and slow progression, especially in middle-aged and elderly people, require a differential diagnosis between neurodegenerative diseases and brain space-occupying lesions
. In this case, an MRI of the brain is indicated.
Treatment and prognosis of post-stroke aphasia
Speech disorders significantly disable patients, reduce the quality of life of both themselves and those around them, interfere with full neurorehabilitation, and increase the economic costs of treatment. In addition, patients with post-stroke aphasia, compared with patients with stroke but without speech disorders, have higher mortality rates and stay in hospital longer [16].
The degree of speech restoration depends primarily on the location and extent of damage to the brain. For example, sensorimotor aphasia as a result of ischemic stroke of the cardioembolic type, usually in combination with right-sided hemiparesis and hemihypesthesia, has a less favorable prognosis than motor aphasia as a result of a stroke in the anterior cortical branches of the middle cerebral artery [17].
Predictors of good recovery of speech function are young age, high Barthel index, high level of education and hemorrhagic nature of the stroke [17].
Management of a patient with aphasia involves, in addition to treating the underlying vascular disease, systematic speech therapy exercises [17–19]. They are carried out by patients independently under the supervision of relatives. The clinical effectiveness of speech rehabilitation has been assessed in a number of studies [20, 21]. It has been shown that the specific method of speech therapy correction is not of fundamental importance, while the frequency and intensity of classes significantly influence the prognosis [22, 23]. Speech therapy exercises must be started already in the acute phase of a stroke and continued throughout the entire recovery period, as long as the patient continues to have speech disorders. Currently, computer programs and applications for phones and tablets have been developed that allow the patient to communicate with others and independently perform speech exercises.
Restoration of speech in the first months after a stroke is associated with reperfusion of the corresponding cortical centers, activation of adjacent cortical areas and homologous brain areas in the contralateral hemisphere. This is evidenced by studies using diffusion-weighted and perfusion MRI methods [24, 25].
Drug therapy in patients with aphasia should be aimed at metabolic support of neuroreparative processes and improvement of cerebral blood flow.
To date, several randomized, double-blind studies of medications for post-stroke aphasia have been conducted. The effectiveness of bromocriptine [26] and amphetamine [27] has not been proven, and a meta-analysis of clinical studies of piracetam indicated a rather modest effect of this drug [28]. There is little clinical experience with the use of anticholinesterase inhibitors such as donepezil and galantamine, but their clinical effectiveness requires further study [29, 30].
Currently, the use of citicoline in patients with post-stroke aphasia seems promising. Citicoline (Ceraxon) is an endogenous mononucleotide containing ribose, cytosine, pyrophosphate and choline in its chemical structure. Being a necessary intermediate substance in the synthesis of structural phospholipids of the cytoplasmic and mitochondrial membranes of neurons, citicoline restores their integrity during ischemic damage. A number of experimental studies have shown that citicoline inhibits the enzyme phospholipase A2, normalizes energy processes in mitochondria, restoring the functioning of membrane sodium-potassium and mitochondrial adenosine triphosphatases. In addition, it enhances the activity of antioxidant systems, thereby providing a neuroprotective effect and preventing the processes of oxidative stress and apoptosis. Another mechanism of action of Ceraxon is to replenish cerebral acetylcholinergic deficiency, which is of great importance for metabolic support of cognitive activity in general. Finally, this drug affects dopamine and glutamatergic neurotransmission. Citicoline has a pleiotropic effect, also due to its influence on neurorepair processes, which play a key role in restoring lost functions [31]. A number of experiments demonstrated the effect of the drug on the processes of neuroglial activation, enhancement of post-ischemic neurogenesis, angiogenesis and neuroplasticity [32, 33]. It has been established that citicoline reduces the volume of brain damage during experimental ischemia and hypoxia, increases learning ability and has a beneficial effect on memory in experimental animals with age-related changes in the brain.
In clinical studies, Ceraxon improved functional recovery and accelerated rehabilitation of patients with ischemic stroke [34]. Currently, the effectiveness of citicoline in post-stroke cognitive and motor disorders has been shown [35, 36]. Moreover, the drug is characterized by a satisfactory safety and tolerability profile. The positive effect of the drug on speech disorders in patients after stroke has not been separately assessed. However, it can be assumed that the neuroregenerative properties of Ceraxon and its effects in the cognitive sphere will contribute to the improvement of speech functions due to the close relationship of these disorders.
Conclusion
When treating patients with aphasia, regular speech therapy sessions and long-term drug therapy are required, aimed at metabolic support of neuroreparative processes and improvement of cerebral blood flow.
Communication Guide
You can and should communicate with people with aphasia. Patients retain some communicative abilities that need to be activated through communication, without allowing them to “fade away.” Those who suffer from a severe form of aphasia retain the ability to understand the meaning of what is said (although not every word individually). Often the patient may not understand what is being said to him because he does not remember the meaning of individual words or forgets the beginning of a phrase.
How to communicate with people with aphasia:
- sit down and catch the person's eye
- if you are afraid of communication, you should start with simple topics, for example, tell how your day was in the simplest terms, then you need to ask a simple question
- It’s better to speak at a slow pace, focusing your voice on key words in the text
- You can do the following practice: write down the key words of the future conversation on paper, then repeat what was said and show the paper to the patient. This will be his cue for conversation.
- use not only the spoken word to communicate, but also writing, drawings, gestures, and pointing at objects. Forgive a person to do the same, let him use a dictionary if it will be easier to communicate
- if the patient is trying to convey some idea to you, determine who he is talking about, what exactly happened and in what place
- it is important to be able to ask leading questions
- do not ask questions that require monosyllabic answers
- be patient, because communication with a person with aphasia is far from easy, but it is necessary
Dialogical work
Our main work in the correction of aphasia is dialogic speech.
Scheme of work in this direction:
- the patient repeats the prepared answer phrase;
- the speech therapist prompts the first one or two syllables, and the patient must complete the word or phrase;
- the patient must select one or more words from those spoken by the speech therapist;
- the patient must answer the speech therapist’s question without prompting.
Remember, aphasia is treatable. If in adults the recovery process is difficult and takes a lot of time, then in children aphasia is treated quite quickly and effectively. The use of effective techniques, songs, and negotiation exercises significantly accelerates the patient’s process of developing coherent speech.
Our speech pathologists and speech pathologists conduct speech therapy classes in Almaty for the correction of aphasia in both adults and children. If you need help or advice, please contact us!
Like a child!
Speech is a complex process in which different areas of the cerebral cortex actively interact. Thus, Wernicke's area is responsible for understanding; signals are formed in Broca's area, which ultimately turn into words and phrases. The role of auditory and visual analyzers is important. When a person talks, the whole brain is actively working. It establishes connections, for example, between the image of a spoon and the word that denotes this object. It is these connections that are destroyed in patients with amnestic aphasia. This is the difference between patients of the NeuroSpectrum Center for Pediatric Speech Neurology and Rehabilitation, who are being treated for amnestic aphasia, and healthy children. The normal process of forming connections goes by itself, and if connections are destroyed, their restoration requires outside help. Fortunately, children's brains are plastic, and it is easier to help our patients than adults and especially older people.
Clinical manifestations
Symptoms of amnestic aphasia develop slowly, and therefore the patient himself and his loved ones may not be aware of the disease for a long time. The periodic inability to name an object is often associated with a person's age, which leads to a late diagnosis. The main clinical manifestations include the following clinical signs:
- a person cannot name an object, however, he can easily describe its external characteristics and purpose;
- due to the difficulty of selecting the names of things, the patient’s speech is slow and has a large number of pauses (the opposite situation may be observed - fluent speech with frequent errors in the use of words);
- repetition of the same words and phrases (typically a large number of descriptive constructions and paraphrases);
- the number of nouns decreases (most often, speech consists of adjectives that describe an object);
- speech is logical and grammatically correct;
- reading and writing skills do not suffer and remain at the same level;
- the pronunciation of sounds and their combinations does not change;
- articulation changes are not detected.
Amnestic aphasia is characterized by the inability to retain the name of an object. As a result, the patient uses complex descriptive constructions consisting mainly of adjectives. It is this feature of speech that allows one to suspect a disease and seek medical help.