Kinds
Idiopathic brachial neuritis
Idiopathic brachial neuritis is a disorder of unknown etiology with an asymmetrical arrangement of the brachial plexus. It occurs in all age groups, but is more common between the third and seventh decades. Men are more often affected than women. Intervening events occurring days or weeks before the onset were noted in 28-83% of cases in various ways. Respiratory infections, influenza-like illnesses, immunizations, surgery, and emotional stress were common symptoms, with no triggers found in half of the cases. Idiopathic brachial neuritis is more common in men who engage in vigorous athletic activities such as wrestling, weight lifting, and gymnastics.
The pathophysiology of idiopathic brachial neuritis is not fully understood, and the disease is considered an immune-mediated disorder.
Idiopathic hypertrophic brachial neuritis
This disease is uncommon and tends to gradually affect the brachial plexus. The disease continues for several months or even years, and gradually progressive weakness and wasting of the segments affected by this disease is a key, but at the same time, often ignored symptom.
This disease differs from the above-described idiopathic brachial neuritis in its painless course, although some patients may have minor pain and weakness.
Hereditary neuralgic amyotrophy
Hereditary neuralgic amyotrophy is an autosomal dominant disorder characterized by repeated episodes of paralysis and sensory impairment of the affected limb, preceded by severe pain. Hereditary neuralgic amyotrophy is genetically linked to chromosome 17q25, where mutations in the septin-9 gene have been found. Hereditary neuralgic amyotrophy is a rare disease and its worldwide prevalence is unknown.
Onset of hereditary neuralgic amyotrophy occurs at birth or later in childhood, with a good prognosis for cure. However, individuals with hereditary neuralgic amyotrophy may have permanent residual neurological deficits after repeated attacks.
Neurogenic thoracic outlet syndrome
Neurogenic thoracic outlet syndrome is characterized by pain, paresthesia, and weakness of the upper extremities, which may be aggravated by raising the arms or frequent movements of the head and neck. This is usually seen in women.
Cancer-associated brachial plexiopathy
Brachial plexus involvement is a well-known complication of cancer. Pectoral plexopathy in such cases may be caused by metastatic spread or a consequence of radiation therapy for cancer.
Traumatic form of brachial plexopathy
Trauma is one of the most common causes of brachial plexopathy. These injuries usually result from a motorcycle or high-speed traffic accident, a fall from a significant height, or an impact. This can occur with penetrating trauma and gunshot wounds. This may be the result of iatrogenic trauma. In injured patients, the consequences should be carefully assessed. Determine the extent of head, neck and shoulder injuries. With open injuries, there may be damage to large blood vessels and lungs, in which case urgent surgical intervention is necessary.
Symptoms
With neuritis, the nerve fiber is damaged, and therefore the functions suffer, the main ones being sensitive, motor and trophic, therefore the following symptoms are clinically noted:
- In the phase of irritation of the nerve fiber: pain, burning, feeling of “crawling goosebumps”, feeling “as if many needles are being pricked”.
- In the phase of loss of functions: decreased muscle strength, muscle atrophy, decreased reflexes, decreased sensitivity, tissue atrophy including skin, subcutaneous fat, muscles, bone tissue.
Causes
These nerves can be damaged by stretching, pressure, or cutting. A strain can occur when the head and neck are forced away from the shoulder, such as during a fall from a motorcycle or sometimes a car accident. In more severe cases, the nerves may become torn from the spinal cord. Pressure can occur when the brachial plexus between the collarbone and the first rib is damaged, which can occur during a fracture or dislocation. Swelling in the area from excessive bleeding or damaged soft tissue can also lead to injury.
Signs of illness
Pinching of various nerves (in particular, axillary, radial and median) can occur. As practice shows, during diagnostic examinations it is often determined that the radial nerve has been affected. It belongs to the nerve trunks, consisting of a motor and sensory part.
When a nerve is pinched in the shoulder, the symptoms may differ slightly from patient to patient (depending on the cause that provoked the disease). However, there are common characteristic features. First of all, the person experiences severe pain. It can be of a different nature (for example, sharp or aching), and occur even at rest, when there is no additional load on the shoulder. As a rule, it continues for a long time.
In general, all clinical manifestations are divided into three main groups: acute, subacute and chronic. Acute signs are characteristic of compression, which arose against the background of traumatic influence. Most often they accompany a fracture, sprain or rupture of ligamentous tendon tissue. Subacute symptoms are characteristic of complex pathologies of the musculoskeletal system (for example, deforming osteoarthritis).
Chronic symptoms are associated with degenerative-dystrophic diseases of the spinal column (for example, in the presence of cervical osteochondrosis with radicular syndrome). They are distinguished by painful sensations of a dull nature. They are constantly present, but due to limited mobility, a person often does not pay attention to them.
In accordance with the specifics of the lesion, experts note the following possible clinical manifestations:
- increased sweating (sweat increases during attacks of pain);
- crawling on the upper limbs and the area between the shoulder blades;
- a feeling of numbness in the thumb, index and middle fingers;
- restriction of movements in the joints of the hand after a night's sleep or a long rest;
- the appearance of involuntary muscle twitching;
- hyperemia and pallor of the skin;
- impaired skin sensitivity (pathological decrease in sensitivity) in the shoulder and forearm area.
The pathology does not pose a particular threat to the patient’s life, however, in the absence of proper therapy, the pathological process can progress to the point of muscle atrophy. Based on this, if the above-described signs are detected, you should not delay your visits to a neurologist.
Diagnostics
Many adult injuries will not recover on their own, and early evaluation by physicians who are experienced in treating these problems is important. Some injuries can heal over time or with quality therapy. Recovery time may be weeks or months. When the situation is unlikely to improve, several surgical techniques can be used to improve recovery.
To decide which injuries are most likely to resolve on their own, your doctor will rely on several exams of your arm and shoulder to check muscle strength and feeling in different areas. Additional tests such as MRI scans or CT/myelography may be used. A nerve conduction study/electromyogram, a test that measures electrical activity transmitted by nerves and muscles, may also be performed.
In some cases where nerve repair does not occur, tendon transfer surgery may be performed.
Clinical picture of some individual nerves
- Trigeminal nerve – pain is sharp, piercing, in series, along one or several branches of the nerve.
- Facial nerve – muscle weakness on one side of the face. It is difficult to close the eye, the corner of the mouth on the affected side is drooping. When liquid food or drink is taken, everything comes out of the mouth.
- Diaphragmatic – feeling of lack of air, shortness of breath, hiccups.
- Median – impaired flexion of the hand, fingers I, II and III and decreased sensitivity on the palmar surface.
- Ulnar – weakness of the flexors of the IV, V and partly III fingers, decreased sensitivity on the palmar surface of the above fingers.
- Radial – impaired extension of the hand and fingers, decreased sensitivity in half of the back of the hand (I and II fingers). It is difficult to move the thumb away.
- External cutaneous nerve of the thigh (Roth-Bernhardt disease) – pain, numbness and burning along the outer surface of the thigh.
- Femoral – impairment of leg extension at the knee joint and hip flexion. Pain and sensory disturbances on the lower 2/3 of the anterior surface of the thigh, the anterior inner surface of the lower leg.
- Sciatic – pain along the back of the thigh and lower leg, weakness of the flexors and extensors of the foot.
- Olfactory – anosmia on one side (lack of sense of smell). When a nerve is irritated, foreign odors may appear.
- Visual – decreased acuity and loss of visual fields. The phenomena of nerve irritation manifest themselves in the form of photopsia (sensation of light, flames, sparks, etc.).
- Oculomotor – drooping of the upper eyelid (ptosis), limited mobility of the eyeball, dilated pupil, diplopia (double vision).
- Block - restriction of the mobility of the eyeball downwards and outwards.
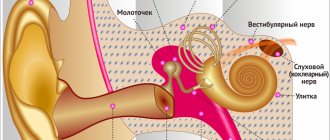
- Auditory – hearing loss, often accompanied by a feeling of noise or ringing in the ear.
- Glossopharyngeal - twitching pain in the tonsils, root of the tongue, pharynx and taste disturbances in the back third of the tongue, impaired salivation and swallowing.
- Wandering – manifested by disturbances in swallowing and speech. On the affected side, the soft palate is lowered, the uvula is deviated to the healthy side. There are also disturbances in the functioning of internal organs - bradycardia, shortness of breath, motility disorders of the esophagus, stomach and intestines (spasms), etc.
- Additional – difficulty turning the head in the healthy direction, the head is tilted towards the affected nerve, the shoulder is lowered.
- Tibial – the foot is extended, but the patient cannot bend it. Cannot stand on toes. Sensitivity is reduced along the back of the lower leg and on the sole.
- Peroneal – the impossibility of standing on the heels and straightening the foot, it hangs down. Sensitivity is reduced on the outer surface of the lower leg and the back of the foot.
- Intercostal nerves – pain in the intercostal space, often radiating into the chest, simulating pain in the heart, chest, lungs, and stomach. Often, pain in the paravertebral muscles is detected at the level of the thoracic spine.
Treatment
In most cases, treatment takes place on an outpatient basis, in severe situations - in a hospital. For plexopathy, anti-inflammatory therapy is carried out, painkillers, dehydrating drugs are used, and physiotherapeutic procedures are also prescribed. After the pain subsides, special exercises, massage, and a complex of vitamins are prescribed.
In more severe situations, surgical treatment is prescribed to eliminate the compression and restore the functionality of the plexus branches.