Infographic: the whole truth about meningitis
The colder it gets outside, the more often the classic “put on a hat or you’ll get meningitis” sounds. In reality, a hat has practically nothing to do with meningitis - no headdress can protect against a dangerous infectious disease. Let's figure out what you need to know about meningitis, and also find out what common misconceptions about this disease we encounter regularly.
What is meningitis?
Meningitis is an inflammatory process that affects the membranes of the spinal cord and/or brain. Inflammation is caused by pathogenic microorganisms - bacteria, viruses, fungi and even protozoa.
The most common (and least dangerous) is viral meningitis, which is often a complication of influenza, measles, mumps and other viral diseases. The peak of its distribution is late summer and autumn.
Meningitis - symptoms and treatment
The variety of pathogens and the individual characteristics of individuals in the human population also determine the fairly pronounced variability in the forms and manifestations of meningitis and the risk of infection for other people, so in this article we will focus on the most significant forms of diseases and their causative agents in social terms.
Meningococcal meningitis is always an acute (acute) disease. Caused by Wekselbaum's meningococcus (a gram-negative bacterium, unstable in the environment, at a temperature of 50 degrees Celsius it dies after 5 minutes, UV irradiation and 70% alcohol kill almost instantly). The source of the spread of infection is a sick person (including meningococcal nasopharyngitis) and a bacteria carrier; transmission occurs by airborne droplets.
The site of introduction (gate) is the mucous membrane of the nasopharynx. In the vast majority of cases, the infectious process does not develop or local forms of the disease develop. When meningococcus overcomes local anti-infective barriers, hematogenous spread of infection occurs and a generalized meningococcal infection occurs, including the development of meningococcal meningitis, which, in the absence of adequate treatment, ends in death in more than 50% of cases. In the pathogenesis of the disease, toxins that are released after the death of bacteria in the bloodstream and damage to the walls of blood vessels play a role, which leads to hemodynamic disturbances, hemorrhages in organs and profound metabolic disorders. Hyperirritation of the meninges occurs, the development of purulent inflammation of the tissue and a rapid increase in intracranial pressure. Often, due to edema and swelling of the brain tissue, the brain becomes wedged into the foramen magnum and the patient dies from respiratory paralysis.
The latent period of illness is from 2 to 10 days. The onset is acute (even more correctly, acute). In the first hours of the disease, there is a sharp increasing increase in body temperature to 38.5 degrees and above, severe lethargy, fatigue, pain in the periorbital region, loss of appetite, and a sharp headache. A characteristic sign of a headache is a constant increase in its intensity, diffuse pain without clear localization, bursting or pressing in nature, causing true agony for the patient. At the height of the headache, vomiting occurs without preceding nausea, which does not bring any relief. Sometimes in patients with a severe uncontrolled course, mainly in children in an unconscious state, there is an uncontrollable cry, accompanied by clasping the head with one’s hands - the so-called. “hydrocephalic cry” caused by a sharp increase in intracranial pressure. The appearance of the patients is etched in the memory - sharpening of facial features (Lafora’s symptom), meningeal posture on the 2-3rd day of the disease (still “coping dog”). Some patients develop hemorrhagic rashes on the body, resembling a star-shaped rash (an unfavorable sign). Over the course of 2-3 days, the severity of symptoms increases, hallucinations and delusions may appear. The degree of impairment of consciousness can vary from somnolence to coma; if untreated, death can occur at any time.
Tuberculous meningitis is a slowly developing pathology. It is mainly secondary, developing in the context of existing tuberculosis in other organs. It has several periods of development, consistently developing over a long time:
1. prodromal (up to 10 days, characterized by mild symptoms of general malaise)
2. sensorimotor irritation (from 8 to 15 days, the appearance of initial cerebral and weak meningeal manifestations)
3. paresis and paralysis (attracts attention from the 3rd week from the onset of the infectious process in the form of changes and loss of consciousness, difficulty swallowing, speech).
Initially, a moderate increase in body temperature appears without pronounced jumps and rises, quite tolerable headaches of low intensity, well relieved by taking analgesics. In the future, headaches intensify, nausea and vomiting become involved. An invariable sign of tuberculous meningitis is a rise in temperature, fever, and the numbers and duration can vary from subfebrile to hectic values. Gradually, from the end of the second week, symptoms of disorientation and stupor appear and slowly increase, ending in deep “congestion” of the patient, stupor and coma. Dysfunction of the pelvic organs and abdominal pain develop. Meningeal symptoms also gradually develop, and truly classic symptoms (the “pointing dog” position) develop only in advanced cases.
Herpetic meningitis is most often caused by herpes simplex viruses types 1 and 2, the chickenpox virus and develops against a background of weakening of the body due to acute respiratory viral infections or serious immunosuppression, incl. AIDS. It is divided into primary (when the process develops during initial infection with the virus) and secondary (reactivation of the infection against the background of decreased immunity). Always an acute disease, the primary manifestations depend on the previous premorbid background. More often, against the background of acute respiratory viral infections, herpetic rashes of the perioral area and genital organs, a severe headache of a diffuse nature occurs, increasing over time, and vomiting, which does not bring relief. All this can occur against the background of a moderate or high increase in body temperature and mild meningeal symptoms. Brain damage is often associated; in such cases, mental disorders (often aggression), hallucinations, disorientation, and generalized convulsions occur within 3-4 days. With proper treatment, the prognosis is usually quite favorable; in the absence of adequate treatment in conditions of impaired immunological resistance, death or persistent residual effects are possible [2].
Relationship with sinusitis. If left untreated, sinusitis can cause the bones in the sinuses to melt. Through them, pus enters the meninges, and meningitis develops.
Diagnosis of meningitis
The diagnosis of meningitis can be made based on the results of additional studies - laboratory and instrumental:
- detailed blood test;
- fundus examination;
- X-ray examination of the skull;
- heart electrocardiograms;
- electroencephalography;
- computer and magnetic resonance imaging.
To confirm the diagnosis of meningitis, doctors use bacteriological examination of mucus from the nasopharynx and cerebrospinal fluid. During bacterioscopic examination of cerebrospinal fluid, smears are stained with Gram or methylene blue. To exclude fungal meningitis, the specimen containing cerebrospinal fluid is stained with ink. Laboratory assistants isolate a pure culture on media with the addition of normal horse serum or cattle serum and identify it by biochemical activity and antigenic structure.
In case of viral meningitis, in preparations prepared with Gram staining and ink, it is impossible to identify the causative agent of the infection. Cultivation of bacteria and fungi also gives negative results. By culturing cellular material with standard laboratory cell lines, a pathogen serologically identical to the measles virus can be isolated. Rubella virus is isolated using the co-cultivation method.
To identify oligoclonal immunoglobulins, the method of agarose gel electrophoresis or isoelectric focusing of cerebrospinal fluid gamma globulins is used. Immunoglobulins appear in a number of viral infections. As a result of immunological studies, viral antigens or antibodies are detected in the cerebrospinal fluid, and the nucleic acid of the virus is detected using the polymerase chain reaction method. The enzyme immunoassay method detects pathogen antigens in feces, urine or saliva. Express methods allow you to quickly and early determine the presence of the herpes simplex virus antigen in the cerebrospinal fluid and blood or the DNA of the virus (using the polymerase chain reaction method).
CSF cytosis in meningitis
Analysis of cerebrospinal fluid allows not only to confirm the diagnosis, but also to differentiate purulent and serous meningitis, identify the causative agent of the disease, determine the degree of intoxication, and also makes it possible to monitor the effectiveness of treatment.
Bacteriological examination of cerebrospinal fluid in the case of tuberculous meningitis may give a false negative result. Detection of tubercle bacilli in the cerebrospinal fluid depends on the thoroughness of the research. At the Yusupov Hospital, all diagnostic procedures are performed using modern medical equipment and the use of new drugs and techniques. The results of studies conducted at the Yusupov Hospital are reliable and as informative as possible.
How is meningitis treated?
At the Yusupov Hospital, patients can receive a full range of medical services for the detection and treatment of meningitis, rehabilitation after illness and prevention. Patients with meningitis can contact the neurologist clinic of the Yusupov Hospital every day for 24 hours to receive emergency care.
When patients are admitted to the Yusupov Hospital, a comprehensive diagnosis is carried out, including a number of examinations to identify the causes of meningitis, collection of complaints and symptoms. Patients with meningitis need inpatient treatment, so the Yusupov Hospital has created comfortable living conditions and ensures interaction with qualified personnel.
Consequences of meningitis
Since men are less likely to consult a doctor in a timely manner and more often than women suffer from cerebrospinal meningitis, they often develop complications during the illness. Mild complications include headaches when the weather changes or overwork, slight decreases in hearing, concentration, and memory. Depending on the severity of meningitis and the timeliness of seeking medical attention, the following complications may develop:
- a sharp decrease in visual acuity;
- stuttering;
- strabismus;
- significant hearing loss;
- decreased intelligence;
- dropsy of the brain;
- epilepsy;
- mental disorder;
- development of schizophrenia;
- dementia.
The patient may fall into a coma, he may develop paralysis, and with complicated meningitis, death is possible.
The Yusupov Hospital effectively diagnoses the disease. The patient undergoes examination at the hospital's diagnostic center, which is equipped with modern equipment from leading global manufacturers. You can make an appointment with a doctor by calling the Yusupov Hospital.
Symptoms of meningitis in children
The clinical picture of meningitis in children depends on the type of pathogen. In all cases of childhood meningitis, general symptoms predominate, which are united by the concept of “meningeal” syndrome. Meningitis in children often begins acutely rather than gradually. Typically, the symptoms of meningitis are preceded by general signs of an infectious disease: fever, weakness, pain in the joints and muscles. With meningococcal infection, hemorrhagic rashes appear in children, with pneumococcal infection - signs of rhinitis, pneumonia, otitis, with mumps - damage to the salivary glands, with enterovirus infection - dyspeptic disorders and catarrhal phenomena.
Meningeal syndrome has the following symptoms:
- rigidity or stiffness of the neck muscles due to a pathological increase in their tone;
- Kernig's symptom - the patient is unable to fully straighten a previously bent leg at a right angle at the knee and hip joints;
- Brudzinski's symptom: upper - when the patient tilts his head to the chin and lies on his back, the lower limbs automatically bend, lower - if the patient bends one leg at the knee joint, the second limb bends automatically;
- hyperesthesia – increased sensitivity to painful, auditory, olfactory and tactile stimuli, intolerance to bright light;
- local complete or partial paralysis.
Children develop the following signs of meningitis:
- Lesage's symptom - when the baby is taken by the armpits, he presses his legs to his tummy, which cannot be straightened (typical for children under one year old);
- “tripod” symptom – a child, sitting on a flat surface with his legs extended forward, bends his legs or leans back;
- bulging fontanelle;
- Filatov's symptom - when the baby tilts his head quickly or sharply, his pupils dilate.
In children under three years of age, it is extremely rare to have all the signs of meningeal syndrome. Symptoms of meningitis in children 7-8 years old do not differ from signs of the disease in adults. The temperature during meningitis in children rises to 41-42o. Children are bothered by a severe headache that spreads throughout the head. They cry, sometimes screaming.
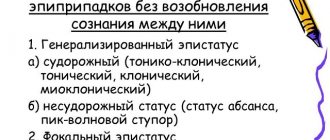
From the first days of the disease, small dark cherry pinpoint rashes appear on the child’s body. In the presence of severe meningococcal infection, the elements of the hemorrhagic rash merge, and large spots or bruises may appear. The child's consciousness is impaired, convulsions and epileptic seizures develop. Children are worried about nausea, continuous vomiting, not associated with food intake, which does not bring relief.