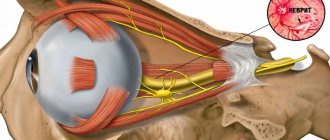
Pathology of the optic nerve associated with circulatory disorders in the intraorbital or intrabulbar region is called ischemic optic neuropathy. This disease is usually diagnosed between the ages of 40 and 60 (more often in men) and is characterized by sudden deterioration of vision, loss of visual fields, and monocular blindness.
Causes of ischemic neuropathy
There are two main forms of the disease - anterior and posterior neuropathies. The first form is caused by impaired blood flow and the subsequent development of ischemia of the scleral, choroidal and retinal parts of the optic nerve head; Posterior ischemic neuropathy is caused by a circulatory disorder in the posterior parts of the optic nerve, as well as narrowing of the carotid and vertebral arteries.
Blood flow may be disrupted as a result of functional pathologies (arterial spasm) or organic changes (sclerosis, thromboembolism). Thus, various factors can lead to the disease. Very often, ischemic optic neuropathy is observed against the background of diseases of the vascular system:
- hypertension;
- atherosclerosis;
- obliterating or nodular arteritis;
- thrombosis of great vessels, etc.
Often, pathology of the optic nerve develops in patients with diabetes mellitus, discopathy of the cervical spine, and anemia. Ischemic phenomena affecting the optic nerve are possible after injuries, operations, hemodialysis and anesthesia.
Causes and types of neuropathy
In 30% of cases, neuropathy is considered idiopathic (that is, arising from unknown causes).
Otherwise, the causes of the disease can be divided into internal and external.
Causes associated with various internal pathologies:
- endocrine diseases, of which diabetes mellitus accounts for about a third of all neuropathies;
- vitamin deficiency, especially deficiency of B vitamins;
- autoimmune diseases;
- multiple sclerosis;
- rheumatoid arthritis, etc.
External factors that provoke the development of neuropathy include:
- alcoholism (a common consequence is neuropathy of the lower extremities);
- injuries;
- intoxication;
- infections.
Often the cause of nerve damage is a hereditary factor. In such cases, the disease can develop independently, without any additional harmful effects.
Neuropathy is a very serious illness that requires qualified diagnosis and adequate treatment. If you are concerned about any of the symptoms listed below, consult a neurologist immediately!
Depending on the location of the disease, neuropathies of the upper, lower extremities and cranial nerves are distinguished, for example:
Facial nerve neuropathy
It can develop as a result of a traumatic brain injury, a viral infection, hypothermia, unsuccessful dental surgery, depression, pregnancy and childbirth, as well as due to a neoplasm. Signs of the disease are: weakening of the muscles on the side of the affected nerve, salivation and lacrimation, inability to completely close the eyelids.
Trigeminal neuropathy
Caused by various reasons (maxillofacial surgery, dentures, difficult childbirth, heredity) damage to the nerve endings of the gums, upper and lower lips, and chin. Patients complain of severe facial pain from the affected nerve, radiating to the upper and lower jaws, not relieved by analgesics. There is also discharge from one nostril, lacrimation and redness of the eye.
Radial nerve neuropathy
It often occurs against the background of so-called “sleep paralysis,” i.e. compression of the nerve due to incorrect position of the hand. Occurs in people who use drugs or alcohol. It also progresses with wrist fractures, bursitis or arthritis. It manifests itself as a violation of the dorsiflexion of the hand (the hand hangs), numbness of the thumb and index fingers, pain can occur on the outer surface of the forearm.
Median nerve neuropathy
Damage to this area of the upper limb can occur due to sprains, fractures, diabetes mellitus, rheumatism, gout, neoplasms, as well as in the event of nerve compression. It manifests itself as severe pain (as well as numbness and burning) in the forearm, shoulder, hand, thumb, index and middle fingers.
Ulnar nerve neuropathy
The cause of this disease may be traumatic (sprain, tear and rupture) or other damage to the ulnar nerve (for example, caused by bursitis, arthritis). It manifests itself as numbness of the first and half of the fourth fingers, a decrease in the volume of the hand, and a decrease in the range of movement.
Sciatic nerve neuropathy
It usually results from a serious injury or illness (knife or gunshot wound, fracture of the hip or pelvic bones, intervertebral hernia, oncology). It manifests itself as pain along the back of the thigh, lower leg, buttock from the side of the nerve lesion.
Neuropathy of the lower extremities
It can develop due to excessive physical overload, tumors in the pelvic area, hypothermia, and also due to the use of certain drugs. Symptoms: inability to bend forward, pain in the back of the thigh, numbness in the lower leg.
Peroneal nerve neuropathy
It occurs due to bruises, dislocations and other injuries, as well as due to curvature of the spine, carpal tunnel syndrome, and wearing narrow, uncomfortable shoes. Manifestations: inability to dorsiflex the foot, cock-like gait (the patient cannot bend the foot towards himself).
1 Massage
2 Massage
3 Acupuncture
Symptoms of ischemic neuropathy
Most often, this disease affects only one eye, but approximately 1/3 of patients may also experience problems of a bilateral nature. In some cases, the pathology affects the second eye after some time (usually within 2-5 years).
As a rule, the pathology appears suddenly - after a hot bath, physical activity, or even after sleep. Visual acuity drops sharply (sometimes only light perception is preserved, and with total nerve damage, blindness occurs). Vision may deteriorate within minutes. Vision deterioration may be preceded by blurred vision, pain behind the eyeball, or headaches.
The peculiarity of this disease is that during its development, peripheral vision is always impaired. In this case, scotomas, concentric narrowing of the visual fields, and loss in various segments (lower, nasal, temporal halves) may be observed.
The duration of acute ischemia is several weeks. Then the swelling of the optic nerve head gradually subsides, and the hemorrhages resolve. Optic disc atrophy persists, with varying degrees of severity. Visual defects also remain, but may be reduced.
Diagnostics
The presence of the median nerve is indicated by the following results of functional tests:
- with the palm pressed to the table, the patient cannot make scratching movements with the 2nd finger;
- when the affected hand is clenched into a fist, bending the first three fingers is most difficult;
- the patient is unable to place the little finger and thumb on the same plane.
Additionally, various electrophysiological procedures may be prescribed. In each individual case, the neurologist working with you at the Health Workshop clinic will draw up an individual list of required examinations.
Diagnosis of the disease
To identify the true cause of the problem, the patient is examined by specialists in various fields of medicine - ophthalmologist, neurologist, cardiologist, endocrinologist and others. A comprehensive examination is prescribed, the ophthalmological part of which consists of the following diagnostic measures:
- functional tests;
- examination of various structures of the eyeball;
- Ultrasound of the eye;
- angiography of retinal vessels;
- electrophysiological studies, etc.
A study of visual acuity demonstrates its significant decrease. The nature of the visual field defects will indicate damage to certain areas of the optic nerve. During ophthalmoscopy, the ophthalmologist will note an enlargement of the optic nerve head, its swelling and pallor. There are signs of vascular disorders (focal hemorrhages, narrowed or dilated veins), and exudate may accumulate.
Angiographic examination will reveal retinal angiosclerosis, uneven diameter of veins and arteries, fibrosis. Electrophysiological studies will show decreased functionality of the optic nerve.
Material and methods
The study included patients aged 18 years or older with CTS who underwent median nerve decompression at the wrist in 2016–2017. at the Clinic of Nervous Diseases named after. AND I. Kozhevnikov First Moscow State Medical University named after. THEM. Sechenov. The study included 85 patients (14 men and 71 women) aged from 36 to 84 years (mean age 62±10.6 years).
When collecting anamnesis, gender and age were recorded, the nature of the patient’s professional and other activities was analyzed, and the presence of concomitant diseases and medications taken were clarified. We analyzed the diagnosis and treatment prior to the patient's visit to the Clinic for Nervous Diseases. The general somatic and neurological status was assessed, and specific Tinel and Phalen tests were performed to determine compression of the median nerve. The Tinel test was considered positive if, during percussion in the projection of the median nerve in the area of the grooves of the wrist, irradiation of pain and tingling in the fingers occurred. The Phalen test was considered positive if paresthesia occurred in the fingers with maximum flexion of the hands at the wrist joints and raising the arms up for 1 minute [18].
Patients were surveyed using the Boston Carpal Tunnel Questionnaire (BCTQ), which allows assessing the severity of symptoms of the disease and functional deficit. The intensity of pain was assessed using a visual analogue scale (VAS). Among the instrumental examination methods, patients underwent ENMG of the upper extremities and ultrasound of the median nerves at the wrist level. The diagnosis was made based on patient complaints, clinical symptoms and results of instrumental studies.
Treatment of patients consisted of surgical decompression of the median nerve at the level of the wrist by completely cutting the transverse ligament.
Statistical data processing was performed using the Statistica 10.0 program
Prognosis and prevention
Despite timely and correctly prescribed treatment, the prognosis is most often unfavorable. Often there remains a strong decrease in visual function and persistent defects in the periphery of vision caused by atrophy of the optic nerves. An increase in visual acuity of only 0.1-0.2 can be achieved only in 50% of cases. If both eyes are affected at once, there is a high probability of developing low vision or complete blindness.
Prevention of ischemic optic neuropathy is important and involves the treatment of vascular and systemic diseases. A patient who has suffered ischemic optic neuropathy in only one eye urgently needs follow-up with an ophthalmologist with appropriate preventive therapy.
General information
Ischemic optic neuropathy is a disease of mature adults. It most often occurs in patients aged 40-60 years, and most often in men. This is a fairly dangerous condition for health, which can cause serious loss of vision, even complete blindness. Ischemic neuropathy is not an independent disease; it occurs as a manifestation of various processes in the body. The cause of neuropathy can be both ophthalmological problems and cardiac, neurological, rheumatological, hematological and endocrinological abnormalities.