This is a group of rare genetic diseases that are inherited in an autosomal recessive manner. With this pathology, the mechanisms responsible for regulating muscle activity change to varying degrees, which leads to dysfunction of the latter. Despite the low incidence, congenital myasthenic syndromes are difficult to detect in the early stages and treat effectively. Therefore, this group of diseases is currently of great interest to doctors and is under close supervision by scientists.
What are the causes of myasthenia gravis?
The disease can be congenital or acquired. The congenital form is caused by a mutation in the genes of certain proteins involved in the process of contraction of muscle fibers. In most cases, when the disease manifests itself between the ages of one and 17 years, disorders are detected in the thymus gland, which is the main organ of the human immune system. Treatment requires surgery to remove it. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3206364/ Maria F. Finnis and Sandeep Jayawant Juvenile Myasthenia Gravis: A Paediatric Perspective // Autoimmune Dis. 2011; 2011: 404101
The acquired form often develops against the background of stress, dysfunction of the immune system, and viruses. Of the total number of patients with this form, children account for 1-3%.
Discussion
The peculiarity of this clinical observation was the severe course of the disease, as well as the rapid progression of symptoms against the background of the absence of specific changes according to the results of additional research methods. During the examination of the patient, a differential diagnosis was made with neoplastic syndrome of the brain and spinal cord, multiple sclerosis, infectious lesions of the central nervous system, and Guillain-Barre syndrome.
Changes in the general blood test and increased levels of procalcitonin indicate the presence of an inflammatory process in the body, but are not specific signs. The acute onset of the disease with the appearance of neurological disorders, the absence of cerebral symptoms, intoxication syndrome, changes in the cerebrospinal fluid, as well as the development of apnea without previous signs of respiratory failure - these features indicated the absence of an infectious lesion of the central nervous system. MRI allowed us to exclude structural changes in the cervical spinal cord, infectious and demyelinating processes. CT scan of the mediastinal organs with intravenous contrast excluded thymoma, the presence of which may be one of the reasons for the development of the autoimmune process in myasthenia gravis. The absence of specific changes in the results of stimulation ENMG also did not allow us to reliably confirm the diagnosis.
Currently in Russia, the diagnosis and treatment of children with myasthenia gravis is carried out in accordance with the clinical recommendations of the Union of Pediatricians of Russia 2021. Considering that the disease is based on an autoimmune process, drugs with an immunosuppressive effect are used in treatment: glucocorticosteroids, cytostatics, immunoglobulins in high doses . However, long-term treatment with these drugs is unacceptable due to significant side effects (excess body weight, leukopenia, osteoporosis, behavioral disorders, etc.), so they are used to stabilize the condition in the acute period. Thus, the drugs of choice for long-term therapy are choline esterase inhibitors - pyridostigmine bromide and neostigmine methyl sulfate, which are contraindicated under the age of 18 years and are prescribed strictly with the consent of the patient or his official representatives.
In the presented clinical observation, intravenous administration of class G immunoglobulins and high doses of glucocorticosteroids made it possible to stabilize the patient’s condition, and the prescription of specific therapy accelerated his recovery and significantly improved the quality of life after discharge from the hospital.
Course and characteristics of the disease
If the mother has myasthenia gravis, then there is a 10-20% chance of having a child with this disease. However, myasthenic syndrome in this case has a transient form (lasts from several days to 1.5 months).
In newborns, the disease manifests itself as follows:
- faint cry;
- muscle hypotonia;
- difficulty sucking and breathing.
The following may also develop:
- prolapse (ptosis) of one of the organs;
- impaired eye movement;
- anemia;
- inhibition of deep reflexes;
- difficulty swallowing.
Congenital myasthenia in young children can provoke the following types of disorders:
- general muscle weakness with impaired breathing and cardiac function, as well as without evidence of manifestations;
- local muscle weakness (face and pharynx without and with breathing problems; eyes);
- musculoskeletal weakness with or without breathing problems.
Myasthenia gravis is classified according to several criteria:
- age of the patient (neonatal, juvenile, adult disease);
- presence of antibodies (seropositive, seronegative);
- clinical picture (transient with complete regression, non-progressive for several years, progressive, malignant with a rapid increase in disorders);
- degree of violations (general, local);
- severity of the course (mild, moderate, severe);
- completeness of recovery after the introduction of antibodies (complete, incomplete, low);
- the presence of deterioration of vital body functions.
Symptoms in children
The following manifestations of the disease are typical for children :
- organ ptosis;
- insufficient eye movement;
- decreased chewing function;
- double vision;
- violation of facial expressions;
- difficulty swallowing;
- unusual fatigue of the upper limbs, neck, pelvic muscles;
- fixed gaze, drooping eyelids, unusual facial expression;
- speech disorders;
- nasality.Source: M.L. Chukhlovina, N.P. Shabalov, N.V. Zinzerling Features of the pathogenesis, clinical picture and diagnosis of myasthenia gravis in childhood // Pediatrics, 2006, No. 3, pp. 90-94
Basically, the disease begins with one symptom, but others join it quite quickly. The first few months the process spreads to the entire body. There are also local forms, which are more severe in children than in adults.
The general form is characterized by involvement of the muscles of the trunk, neck, and limbs, rapid fatigue and weakness, which worsen after exercise.
Local forms are divided according to the affected areas:
- an eye disorder entails impaired eye movements, strabismus, one- or two-sided ptosis, double vision. These symptoms intensify in the evening and may decrease after rest;
- musculoskeletal and pharyngofacial disorder manifests itself in impaired cardiac and respiratory function;
- separately, the pharyngeal-facial form causes impaired facial expressions, weakness of the tongue, and laryngeal muscles, which is expressed in speech and swallowing disorders.
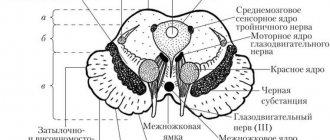
Mechanism of development of congenital myasthenic syndromes
Congenital myasthenic syndromes can develop as a result of presynaptic and postsynaptic defects. In the first case, the processes of synthesis and secretion of acetylcholine, the most important neurotransmitter, which ensures signal transmission from nerve endings to the muscle itself, change. With this mechanism, it is also possible to reduce the bubbles (vesicles) in which acetylcholine accumulates, which also leads to its insufficient release. Postsynaptic defects can lead to a deficiency of a specific enzyme (acetylcholinesterase), which is involved in the synthesis of acetylcholine. There may be a dysfunction or change in the structure of receptors that interact with the neurotransmitter.
Treatment of myasthenia in children
Conservative and radical methods are used to treat children. Conservative treatment includes the use of a number of drugs. They are selected individually based on the clinical picture and severity of the disease.
During surgery, the thymus gland is removed. It is this that causes myasthenia gravis in 70-80% of cases. This treatment is indicated for moderate or severe forms of the disease.
It is extremely important for parents to contact a specialist - a neurologist - as soon as possible for timely diagnosis and treatment. This is due to the fact that with a short duration of myasthenia gravis, the prognosis is much better than in the case when the disease lasts more than five years.
Some of the best pediatric doctors in St. Petersburg are ready to see you at the medical clinic. Make an appointment as soon as possible and your child will be healthy and happy.
Sources:
- M.L. Chukhlovina, N.P. Shabalov, N.V. Zinzerling. Features of the pathogenesis, clinical picture and diagnosis of myasthenia gravis in childhood // Pediatrics, 2006, No. 3, pp. 90-94.
- A.I. Smolin. Modern aspects of clinical practice and diagnosis of myasthenia gravis // Siberian Medical Journal, 2013, No. 3, pp. 12-15.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3206364/
Maria F. Finnis and Sandeep Jayawant. Juvenile Myasthenia Gravis: A Paediatric Perspective // Autoimmune Dis. 2011; 2011: 404101.
Pitsukha Svetlana Anatolyevna Clinic
Author of the article
Pitsukha Svetlana Anatolevna
Doctor of the highest qualification category
Specialty: neurologist
Experience: 24 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Clinical observation
Patient V., 13 years old. Three days before hospitalization, in the morning there were complaints of lethargy, weakness, and a feeling of a lump in the throat, due to which he could not swallow food. The next day, the parents contacted their local pediatrician. A diagnosis of “catarrhal tonsillitis” was made, antibacterial therapy was prescribed, but the condition worsened, speech disturbances appeared, the child stopped swallowing saliva and moving independently. The next day, due to an increase in symptoms, an ambulance team was called, and the patient was hospitalized in the city hospital in the department of anesthesiology and intensive care. Upon admission, the condition was severe due to neurological symptoms: severe muscle weakness, bulbar disorders. Conscious and reacts adequately to examination. Doesn't sit or walk independently. Quiet speech, bulbar dysarthria, dysphagia, drooling. An MRI of the brain did not reveal any pathology. The general blood test showed slight leukocytosis. The results of other examination methods (biochemical blood test, ECG, ultrasound of the abdominal organs, EchoCG) were unremarkable. For further treatment and examination, the patient was transferred to the neurological department of the State Autonomous Institution of the Children's Clinical Hospital, and due to the severity of his condition, he was placed in the intensive care unit.
From the life history:
grew and developed according to his age. There was no allergic history and there were no operations. In August 2008, he received a closed head injury, was treated as an outpatient, and suffered from headaches. An MRI of the brain in 2021 revealed a retrocerebellar arachnoid cyst, and an MRI of the cervical spine showed asymmetry of the vertebral arteries. A neurosurgeon was consulted and conservative treatment was recommended. He was often bothered by headaches and fatigue, for which he repeatedly underwent inpatient treatment in the neurological department at his place of residence.
On admission:
the condition is serious, the consciousness is clear, the position is passive. The skin is clean, moderately pale. Body temperature 36.7 °C. The chest corresponds to the constitution. Breathing is spontaneous, carried out in all departments, there is no wheezing. The respiratory rate is 22 per minute. Heart sounds are clear, rhythmic, heart rate 98 per minute. The abdomen is freely accessible to palpation. Parenchymal organs are not enlarged. Urinating on the catheter.
Neurological status:
consciousness is clear. Oriented in space, time, self. Speech is dysarthric, voice is quiet and muffled. Palpebral fissures D=S, pupils D=S. The photoreaction is direct and live, reverse is live. There is limited upward movement of the left eyeball. The face is symmetrical. Dysphagia, dysarthria, hypersalivation. The pharyngeal reflex is weakened. Temperature and tactile sensitivity are not impaired. Tendon reflexes from the upper extremities D=S, high, from the lower extremities D=S, lively. Muscle tone: diffuse muscle hypotonia. Muscle strength is reduced to 2 points in the upper and lower extremities. Holds his head, does not sit up from a lying position on his own, does not sit, does not stand, does not walk. Active movements in the hands are preserved, more so in the left. Pathological Babinski foot reflex on both sides.
Diagnosis on admission:
myasthenia gravis, generalized form, progressive course. Space-occupying lesion of the brainstem, cervical spinal cord? Multiple sclerosis?
A comprehensive examination of the patient was carried out.
Laboratory test data upon admission: leukocytosis 16.4×109/l, thrombocytosis 325×109/l, ESR 22 mm/h, increased fibrinogen level to 4.49 g/l, C-reactive protein to 18.7 mg/l , procalcitonin up to 0.3 ng/ml. Over time, there was a decrease in leukocytosis to 12.0 × 109/l, thrombocytosis to 254 × 109/l, a decrease in ESR to 17 mm/h, and a decrease in fibrinogen levels to 4.29 g/l. Enzyme immunoassay showed class G antibodies to the Epstein-Barr virus: positivity index 21.3. Class M antibodies to the capsid antigen of the Epstein-Barr virus were not detected. An analysis of the cerebrospinal fluid was performed: colorless, transparent, protein 0.213 g/l, glucose 4.3 mmol/l, chlorine 105.0 mmol/l, cytosis 4 cells in 11 mm3, Pandi test negative. Results of a microscopic examination: against the background of a small number of red blood cells, single neutrophils and lymphocytes are found.
X-ray of the chest organs: no evidence of an active process in the lungs was revealed.
Computed tomography (CT) of the chest organs with intravenous contrast: in a series of images of the chest organs with a slice thickness of 1.25 mm, the visible parts of the skeleton are not changed. The great vessels are not changed. The anatomy of the tracheobronchial tree is not disturbed. Pneumatization of the lungs is uneven: the central and peripheral interstitium of the middle lobe is thickened (645 HU), the left lung is emphysematously swollen (-890 HU). There are no focal or infiltrative shadows in the lungs. There is no fluid in the pleural cavities. The walls of the bronchi are not thickened, the lumen of the bronchi is not expanded or deformed. The interlobar pleura is not thickened. The mediastinum is located in the midline. A probe is marked in the esophagus. Lymph nodes are not enlarged. The heart has a normal configuration and normal size. The liver is enlarged: craniocaudal size 201.5 mm. Conclusion: uneven pneumatization of the lungs.
Ultrasound examination of the abdominal organs and kidneys: without features.
Electrocardiography: the electrical axis of the heart is vertical. Severe sinus bradyarrhythmia 88–59 beats/min. Impaired conduction through the system of the right bundle branch. Syndrome of early repolarization of the ventricular myocardium. Load on the left atrium and left ventricle.
Echocardioscopy: the cavity of the left ventricle is moderately enlarged. Myocardial contractility is preserved. Ejection fraction 68%. The pulmonary artery is dilated with 1st degree regurgitation. Tricuspid valve prolapse with 1st degree regurgitation. Mitral valve prolapse of the 1st degree with regurgitation of the 1st degree. Diagonal trabecula in the cavity of the left ventricle.
Magnetic resonance imaging of the cervical spine: on a series of T1 and T2 weighted MRI scans, lordosis was preserved in three projections. The relationship in the atlanto-axial joint is not disturbed. The height of the intervertebral discs in the studied area was preserved, the signals from the cervical discs on T2 were not changed. No dorsal disc herniations were detected. The lumen of the spinal canal is normal, the spinal cord is structural, the signal from it (by T1 and T2) is not changed. The shape and size of the vertebral bodies are normal, the MR signal from the bone marrow is not changed. Conclusion: no data were obtained for pathological changes in the cervical spine.
Stimulation ENMG was performed: no signs of neuromuscular transmission disorders were detected. Antibodies to AChR were not detected. A drug test with proserin was performed: the result was weakly positive.
The child was consulted by specialists.
Ophthalmologist: when examining the fundus of both eyes, the optic disc is pink, slightly paler on the nasal side, a narrow myopic cone, clear contours. The vessels are not changed. In the macular zone and on the periphery there is no pathology. Endocrinologist: at the time of the examination there was no evidence of pathology from the endocrine system. Cardiologist: cardiac dysplasia - 1st degree mitral valve prolapse, 1st degree tricuspid valve prolapse, shortened PQ phenomenon. Nephrologist: no signs of kidney damage. Geneticist: myasthenia gravis, generalized form, progressive course. Over time, he was consulted twice with an infectious disease specialist: an infectious lesion of the central nervous system was excluded.
Taking into account the clinical picture and the results of additional research methods, a diagnosis was made: myasthenia gravis, generalized form, progressive course. Antibacterial therapy and hormonal therapy with dexamethasone (0.64 mg/kg/day) were started. On the 4th day of hospitalization, negative dynamics were noted in the form of complete loss of active movements in the limbs and speech. When changing body position, spontaneous breathing stopped, and therefore the child was transferred to mechanical ventilation.
Therapy with high doses of intravenous prednisolone (6 mg/kg/day) was continued, intravenous human immunoglobulin was administered at a course dose of 0.4 mg/kg/course, and he also received neuroprotective and antibacterial therapy. On the 12th day of hospitalization, positive dynamics were noted in the form of an increase in the range of movements in the feet and left hand. On the 16th day, the child was extubated and humidified oxygen was supplied through a face mask. Breathing is spontaneous and adequate. The range of movements has increased: he writes with his left hand, turns over in bed. From the 20th day the child speaks and holds objects in his hands. On the 25th day, movements in the knee joints and the act of swallowing were restored, and the position of the head changed. Swallows food and liquid independently in small portions, food is digested. On the 28th day, due to positive dynamics, he was transferred from the intensive care unit to the neurological department. Treatment continued with high doses of methylprednisolone (2.5 mg/kg/day) intravenously. From the 30th day, with the consent of the mother, pyridostigmine bromide in tablet form was introduced into therapy at a starting dosage of 0.1 mg/kg/day, followed by an increase to 1 mg/kg/day in 3 doses. During treatment, the act of chewing and swallowing improved, speech became more intelligible, he began to sit with support, and walk with support from both hands. On the 45th day of hospitalization, the child was transferred for further rehabilitation to sanatorium treatment. At a follow-up examination with a neurologist after 6 months. against the background of continuous use of pyridostigmine bromide, complete restoration of motor and speech skills was noted without any adverse reactions to the drug.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a neurologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Prescription of treatment regimen (for a period of 1 month) | 2700 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Transcranial duplex scanning (TCDS) of cerebral vessels | 3600 rub. |