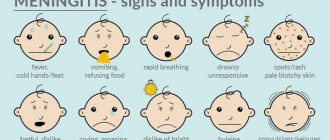
Symptoms
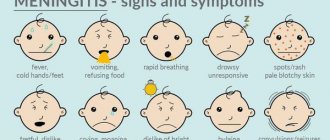
Clinical manifestations of meningitis in children are determined by the virulence of the pathogen, age and state of immunity. There are some differences in symptoms and treatment methods among different age groups. Pathological changes consist of a combination of syndromes: cerebral, infectious and meningeal.
The first signs of meningococcal infection
Menigococcal meningitis develops when meningococci enter the body. In 80% of cases, children under 10 years of age become ill.
It is characterized by sudden fever, bursting headache, which is accompanied by repeated vomiting, photophobia. The child becomes lethargic very quickly. There is a decrease in the threshold of sensitivity, when even a light touch causes severe pain; in infants it manifests itself as general anxiety. In the first hours of the disease, meningeal syndromes appear.
Meningococcal infection is characterized by a forced position, when a child, lying on his back or side, throws back his head and pulls his legs towards his stomach.
Symptoms of meningitis in young children appear gradually. The child becomes restless, emits a sharp cry, vomits, and convulsions occur. There is hyperthermia, a hemorrhagic rash, and a venous network is visible on the head. On examination, the large fontanel is tense and pulsating.
It is necessary to urgently seek medical help if a child has the following symptoms and signs against a background of fever:
- tension of the large fontanelle;
- involuntary muscle twitching;
- the nature of the cry has changed;
- photophobia;
- repeated vomiting;
- constriction of the pupils, squint;
- muscle atony.
In infants, often the only symptom of infection is a bulging or pulsating fontanel.
For pneumococcal pathogens
Pneumococcal meningitis is caused by pneumococci. It ranks second in incidence after meningococcal. More often diagnosed in children under 5 years of age.
The disease with a pneumococcal pathogen has several forms, which determine the first signs of meningitis in children.
To identify meningitis in a school-age child at the initial stage, you should pay attention to the following symptoms:
- occurs in an acute form;
- body temperature suddenly rises to 39-40 C;
- intoxication increases rapidly;
- consciousness is impaired;
- pale skin, cyanosis of the nasolabial triangle, shortness of breath, arrhythmia appear;
- the child reacts negatively to light and noise;
- meningococcal syndrome is weakly or incompletely expressed.
In children under one year of age, a recurrent form is often found. It is characterized by a gradual increase in toxicosis, retraction of the large fontanel. The liver and spleen enlarge, motor activity is impaired. Relapses last from 5 to 10 days, accompanied by periodic fever and deterioration.
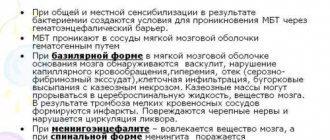
Tuberculous meningitis
Tuberculous meningitis is the most dangerous form of tuberculosis, which usually develops as a secondary process against the background of pulmonary tuberculosis.
The spread of infection occurs by hematogenous or lymphogenous route.
Pulmonary tuberculosis does not manifest itself in any way for a long time, which is why therapy is not carried out, and the risk of generalization of the infection increases. This risk is absent in children vaccinated in the maternity hospital with the BCG anti-tuberculosis vaccine.
Causes of meningitis in children
Children's meningitis can be primary (develop without previous signs of a pathological process caused by the corresponding pathogen) or secondary, when damage to the meninges is preceded by other manifestations of infection (mumps, measles, leptospirosis).
The following microorganisms can cause meningitis:
- bacteria (pneumococcus, meningococcus, Haemophilus influenzae and tuberculosis bacilli, spirochetes);
- viruses (enteroviruses of the Coxsackie-ECHO group, mumps and measles virus);
- chlamydia;
- mycoplasma;
- protozoa;
- mushrooms.
Meningitis most often affects children who belong to the following risk groups:
- premature;
- those born with intrauterine fetal hypoxia or as a result of difficult labor;
- with congenital or acquired immunodeficiency;
- who have undergone craniocerebral, spinal, vertebral trauma, neurosurgical operations and surgical interventions on the abdominal organs.
Children under 5 years of age are more likely to get meningitis. The risk of getting meningitis increases in children who attend preschool institutions and schoolchildren. Children who do not follow the rules of personal hygiene, swallow contaminated water when swimming in reservoirs, and eat food contaminated with rodent excrement are more likely to get sick. The causative agents of meningitis are transmitted by ixodid ticks.
There is a high risk of developing meningitis in children who have not been vaccinated against mumps, measles and rubella, or who have missed vaccinations with Haemophilus influenzae, meningococcus, or pneumococcal conjugate vaccines. When traveling to places dangerous for meningitis, children must be vaccinated no later than 2 weeks before the child’s departure.
The source of pathogens of childhood meningitis are sick people or bacteria carriers. Infectious agents can be transmitted by airborne droplets (with dust and saliva particles), contact (through dirty hands), waterborne, transmissible (through insect bites) and fecal-oral mechanisms. The entry points for infection are the mucous membranes of the upper respiratory tract and digestive organs. The causative agents of meningitis spread throughout the body in the following ways:
- hematogenous (through blood vessels);
- lymphogenous (lymph flow);
- geirogenic (with cerebrospinal fluid).
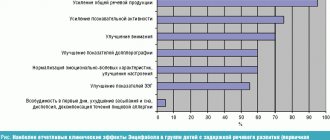
Meningitis in children is accompanied by the following pathological changes:
- increased production of cerebrospinal fluid;
- increased intracranial pressure and permeability of the blood-brain barrier;
- toxic damage to the brain substance;
- disorders of cerebral circulation, especially microcirculation;
- liquorodynamic disorder;
- hypoxia (insufficient oxygen supply) of the brain.
Eventually, swelling of the brain tissue develops. This is facilitated by the spread of the inflammatory process to the ventricles and brain matter, which is characteristic of purulent meningitis. With viral meningitis, cerebral edema is less pronounced, but the medulla is also involved in the pathological process. When the inflammatory process spreads to the brain, focal neurological symptoms appear.
Edema and swelling of the brain leads to its displacement with compression of the brain stem by the cerebellar tonsils. At the same time, the function of vital organs, especially breathing, is disrupted in children, which can lead to death. After suffering viral meningitis, most children do not develop complications. Children who have had bacterial meningitis may be retarded in mental development, and they sometimes develop impaired vision and hearing to the point of complete deafness.
How to recognize a viral infection?
Meningitis of viral etiology is seasonal, with outbreaks occurring in winter and spring. It is caused by various types of viruses: mumps, adenoviruses, enteroviruses and others.
In childhood, meningitis of mumps and enterovirus etiology is more common.
The main signs of meningitis in children 5 years old:
- temperature increase;
- stunnedness (slowing down of mental processes);
- strabismus;
- impaired movement of the eyeballs;
- convulsions.
With mumps meningitis, the clinical picture has features that make it possible to recognize the disease in a child. With this form of infection, the manifestations at different ages are somewhat different.
Hallucinations, delirium, weakness, impaired motor activity, fever are signs of meningitis in children 3 years of age and younger. There is also an increase in headaches and an enlargement of the salivary glands.
Pancreatitis, voluntary muscle movements, in boys, swelling of the scrotum, its redness are additional symptoms of meningitis in children 7-8 years old.
Typical symptoms of enterovirus infection are muscle pain, especially in the abdominal area, fever, herpetic rashes, bursting headache, and dyspeptic disorders. Simultaneously with the high temperature, redness of the face appears, with pallor of the nasolabial triangle, a polymorphic rash, symptoms of conjunctivitis, and hyperemia of the pharynx.
Meningeal signs
The meningeal symptom complex is based on muscular-tonic syndrome, which occurs due to irritation of the nerve receptors of the meninges. Main meningeal syndromes:
- Kernig. The patient lies on his back, the leg is bent at the knee at a right angle, due to strong muscle tension, it is impossible to completely straighten the limb.
- Bekhterev. It is determined by percussion of the zygomatic bone; when it is beaten, the facial muscles of the face contract, due to increased headaches.
- Mandonesi. Pressure on the eyeballs causes contraction of the facial muscles.
- Brudzinsky. The bottom symptom is that if you straighten one leg, the patient will involuntarily pull up the other limb. Upper – when trying to tilt the patient’s head to the chest, flexion of the lower extremities is observed.
- Lesage. Determined in infants. If the symptom is positive, the child, lifted by the armpits, pulls the legs towards the stomach and holds them in this position.
- Flatau. When the head is tilted forward, the pupil dilates.
- Stiffness of the neck muscles. The earliest and most permanent sign of the disease. When trying to raise the head of a patient lying on his back, a sharp resistance is felt, the action fails, or the upper part of the body rises.
The presence of meningeal signs is the main indication for lumbar puncture and cerebrospinal fluid assessment. But it doesn’t always mean meningitis; they are also typical for other infectious diseases!
Nature of the rash
A rash with meningitis in children usually appears in the fulminant form of the disease. It consists of small pinpoint hemorrhages that appear towards the end of the 1st and beginning of the 2nd day of illness. The earlier the rash appears, the more severe the disease. It occurs on the entire surface of the skin, but is more abundant on the buttocks, eyelids, back of the legs, and thighs.
The rash has the shape of stars protruding above the skin level and is dense to the touch. In mild forms of the disease, the rash lasts no more than 2 days; in severe forms, it persists for up to several weeks.
Additional diagnostic measures
During the diagnosis, a blood test and analysis of the separated elements of the skin rash are also carried out. If a specialist suspects the presence of secondary purulent meningitis, then an additional examination is prescribed, the purpose of which is to identify the primary infectious focus. For this, the patient is sent for consultation to a pulmonologist, otolaryngologist or therapist. Effective diagnostic measures here would be otoscopy, x-ray of the paranasal sinuses, and x-ray of the lungs.
Differential diagnosis is carried out with viral meningitis, subarachnoid hemorrhage, meningism, which is also observed in typhus, leptospirosis and severe cases of influenza.
How does it manifest in newborns?
Many parents are interested in the question of how meningitis manifests itself in infants, because they cannot make complaints, and the disease is dangerous and poses a threat to life.
Meningitis in newborns is accompanied by characteristic symptoms:
- dyspepsia;
- monotonous scream;
- hyperexcitability;
- frequent regurgitation;
- twitching of hands and chin;
- vomit;
- throwing back the head;
- loss of appetite;
- low-grade fever;
- increased muscle tone.
The same symptoms occur after severe birth injuries and hypoxia, so an accurate diagnosis is made only after examining the cerebrospinal fluid.
The disease in newborns and children in the first months of life occurs with severe intoxication, muscle hypotonia, respiratory failure, and repeated convulsions are possible.
Can it be determined during the incubation period?
The incubation period for bacterial meningitis lasts 2–7 days, for a viral infection it lasts 2–4 days. In infants it may be less than a day. Its duration largely depends on the state of the child’s immunity; the stronger it is, the longer there are no clinical manifestations.
It is very difficult to determine the disease during this period. Clinical manifestations are very vague or completely absent. But parents should pay attention to changes in the child’s behavior: sudden drowsiness, lethargy, increasing headache, nausea, loss of appetite - may be the first signals of a dangerous infection.
Treatment
If meningitis is suspected, urgent hospitalization to the infectious diseases department is indicated.
For bacterial meningitis, treatment includes:
- antibacterial therapy;
- anticonvulsants;
- non-steroidal anti-inflammatory drugs;
- detoxification therapy;
- antihistamines;
- corticosteroid hormones.
Treatment of meningitis of viral etiology does not require antibiotics. Recombinant interferon, acyclovir, and immunomodulators are used. Infusion and desensitizing therapy are also carried out. After receiving the results of bacteriological culture, therapy is adjusted depending on the pathogen.
The duration of treatment depends on the clinical course of the infection. For meningococcal meningitis, antibiotic therapy lasts 6-10 days, for other etiologies 8-14 days. Treatment begins with intravenous administration of antibiotics and continues until the temperature drops persistently, then switches to oral administration or intramuscular injections of drugs.
MRI for meningitis, what does it show?
The result of magnetic resonance imaging is a series of monochrome images of the brain matter, taken layer by layer in increments of 1 mm. The images alternate between dark and light areas of varying degrees of intensity. The shade transitions correspond to the contours of the internal fabrics. Knowledge of anatomy and experience in the field of radiology allows the doctor to distinguish one anatomical structures from others, assess the compliance of their boundaries and sizes with the norm.
With meningitis, inflammation develops in the meninges, accompanied by thickening of the latter, disturbances in the flow of cerebrospinal fluid, exudation, widening of the furrows and interhemispheric fissure and other nonspecific changes. A scan with contrast shows characteristic staining of areas of inflammation and pathological effusion. MRI after meningitis provides information about the presence or absence of complications and allows one to assess the completeness of the restoration of brain tissue.
Consequences
Severe consequences of meningitis are more often recorded in young children and with delayed treatment.
If the diagnosis is not made on time and therapy is delayed, dangerous complications develop: sepsis, endocarditis, pneumonia, abscess or cerebral edema.
The most common consequences of meningitis suffered in childhood:
- hydrocephalus;
- mental retardation;
- epileptic seizures;
- paresis;
- decreased or loss of hearing;
- damage to the cranial nerves.
Even with a successful outcome, after discharge the child experiences asthenoneurotic conditions: sleep disturbance, anxiety, headaches, memory loss, fatigue.
Prognosis of purulent meningitis
According to statistics, about 15% of all cases of purulent meningitis are fatal. If the diagnosis was made in a timely manner and treatment was started urgently, then the prognosis of the disease will be favorable.
It should be said that after a person has had purulent meningitis, he may develop asthenia with characteristic liquor-dynamic disturbances and inherent hearing loss of a sensorineural nature. Also, in some cases, subtle focal symptoms may be observed.
Such severe complications after suffering purulent meningitis, such as complete deafness, hydrocephalus, amaurosis, dementia or epilepsy, are very rare today.
Prevention measures
Prevention of meningitis depends on the etiology. Patients are urgently hospitalized and isolated. Persons in contact with the sick person are examined for carriage and observed for 10 days.
To prevent a dangerous disease, immunization is carried out. There are several vaccines, both foreign and Russian. For example, the imported vaccine against pneumococcal meningitis “Prevenar” is approved for children from 3 months of age. Well tolerated and does not cause side effects. After completing the full course of vaccination, by the age of two years the child develops stable immunity.
Vaccinations against meningococcal infection are carried out with the Russian vaccine from 1.5 years, and the American vaccine from 2 years.
Vaccination is not included in the scheduled vaccination calendar; it is carried out according to indications or at the personal request of the parents.