Heart pain or spinal problems? Find out everything about your health!
"Novoklinik" does not treat pinched thoracic nerve! If you notice symptoms similar to those described in the article, contact your doctor.
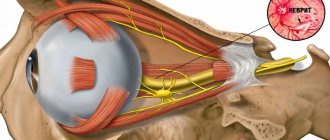
Compression of the spinal cord nerve roots by various structural elements of the spine - vertebrae, intervertebral discs and spinal muscles - is called pinched nerves.
Causes of the disease
In general, all reasons can be divided into two groups. Namely:
- Mechanical damage.
- Degenerative processes.
In the first case, it is enough to turn or bend over unsuccessfully to encounter manifestations of pinching. Also, sometimes pathology is provoked by excessive physical exertion and lack of dosage of work and rest. Degenerative processes include scoliosis, osteochondrosis and other diseases. They lead to disturbances in the structure of the vertebrae and the cartilage between them, accompanied by severe pain and a host of other manifestations.
Physical exercise
Symptoms of a pinched nerve in the thoracic spine can easily arise if, for example, you take on a load that is too heavy for you. You may experience pain if you lift a load too quickly or if you lift it incorrectly and put strain on your back.
Osteochondrosis
It is a dangerous disease, the manifestation of which is often a pinched nerve in the thoracic spine. The pathology causes the cartilage tissue between the vertebrae to wear out and become thinner, which significantly impairs shock absorption. Untimely treated osteochondrosis can lead not only to pinched nerves, but also to the occurrence of intervertebral hernia.
Sensitivity of nerves
The sensitivity of the nerves tends to change over time, and the position of the spine changes in the same way. There are cases when, with age, people experience various types of curvature of the spinal column, which provokes pinched nerves. To eliminate this condition, you will need to stop the displacement and strengthen your back muscles.
Intercostal neuralgia - clarifying the diagnosis
Intercostal neuralgia is sometimes confused with heart pain. Although it is not so difficult to distinguish them.
With intercostal neuralgia, the pain intensifies with deep inhalation or exhalation, or any other movement of the body, including coughing or sneezing, or during physical activity. Sometimes it’s painful and you can’t even take a deep breath - attacks of burning pain appear along the intercostal spaces (pain can only be felt on one side of the chest).
Heart pain with angina pectoris does not change with deep inhalation or exhalation, from a change in position or movement in the chest; usually relieved with nitroglycerin; may be accompanied by irregular pulse rhythm, a drop or increase in blood pressure.
With intercostal neuralgia, the pain may intensify with palpation - you can feel the direction of the pain along the nerve. Aching or paroxysmal pain, spreading along the trunk of the nerve or its branches, may be accompanied by other unpleasant sensations - burning, tingling, numbness. By the way, this is why intercostal neuralgia can cause pain not only in the heart area, but also under the shoulder blade, in the back, and lower back (they can sometimes be confused with kidney pain).
It is important to differentiate an attack of intercostal neuralgia and myocardial infarction, which can also cause severe pain that is not relieved by nitroglycerin. Therefore, if there is a sudden attack of pain in the heart area, you must definitely call an ambulance and have an electrocardiogram done, since a heart attack requires urgent medical attention.
Symptoms
The symptoms of this phenomenon can be either obvious or disguised as diseases of internal organs and other pathologies. Often, treatment for a pinched nerve in the thoracic spine is needed by people who have gone to the doctor with complaints about the heart, stomach and other internal organs, since the pain innervates them. It is worth knowing how a pinched nerve manifests itself in order to recognize the condition in time and consult a neurologist
.
Chest pain
Symptoms of pinching in the thoracic spine are often very similar to symptoms of an angina attack. The person complains about the following:
- there is severe pain and burning under the shoulder blade and in the chest;
- there is not enough air and you can’t breathe in completely;
- hands go numb;
- Cold sweat appears on the body.
To exclude the condition that occurs with angina pectoris, you can put two nitroglycerin tablets under your tongue. If you have heart problems, this remedy will eliminate them within 5 minutes, but if you have a pinched nerve, then the situation will not improve. In this case, there will be severe pain in the vertebral area.
Problems with the gastrointestinal tract
A person who is experiencing digestive problems due to back pain may need to find out what the symptoms and treatment of pinched thoracic spine may be. A person may note:
- Pain in the intestines when trying to change position.
- Spasmodic pain in the abdomen.
- Stool disorders.
Such symptoms may indicate not only pinching, but also a more serious condition - prolapsed intervertebral hernia or displacement of the vertebrae.
Symptoms of intercostal neuralgia
By its nature, intercostal neuralgia is:
- irritation, pinching or inflammation of nerve endings in the intercostal space;
- or entrapment of the roots of the thoracic spinal nerves near the spinal column.
Basically, the pain with intercostal neuralgia is localized in the intercostal space, but pain can radiate along the pinched nerve - in the lower back, in the back, under the scapula. Spastic muscle contractions, redness or paleness of the skin, and loss of skin sensitivity in the area of the affected nerve may occur. The pain with intercostal neuralgia is very strong, burning, constant, without attacks
How to treat?
It is necessary to choose a treatment method depending on what preceded the pinched nerve in the thoracic spine. However, there are general rules for treating pinched nerve roots that will help you get rid of the unpleasant condition.
Drug treatment
If you go to the doctor with complaints of back pain and you are found to have an injury, you will be prescribed a list of medications. These will be:
- antispasmodics;
- drugs to improve blood circulation;
- medications for inflammation;
- vaso-strengthening.
Additionally, painkillers may be prescribed depending on the general condition of the patient. As soon as the condition improves, other treatment methods can be used.
Physiotherapy
Physiotherapy is combined with gymnastic exercises, which allow you to recover and prevent recurrent injuries in the future. If you are experiencing pinching in the thoracic spine, you may be prescribed physical therapy:
- ultrasonic;
- laser;
- electrical stimulation of muscle tissue.
However, all these treatment methods can be used only after the patient’s general condition has improved and pain has been relieved.
Surgical intervention
As a rule, during the treatment of pinched nerve tissue, surgical interventions are avoided. But they will be indicated in a number of cases when there is no improvement in the condition for a long time, and the situation is getting worse. Radical treatment methods will be indicated if:
- conservative treatment was not effective;
- the pain spread further;
- the muscles began to atrophy;
- complications have appeared that affect the functioning of internal organs;
- pathological processes occurred in the intervertebral discs.
In such a situation, in addition to surgically eliminating the cause of the pain, surgery may be necessary to enlarge the hole in the intervertebral disc. But most often, treatment with medications and exercises for severe pinching of the thoracic spine can achieve the desired result, and surgery is a last resort.
Treatment of a pinched intercostal nerve at home
In most cases, treatment of intercostal nerve pinching is carried out at home on an outpatient basis. Patients with serious life-threatening complications are admitted to the hospital.
Treatment for a pinched intercostal nerve should begin by contacting an experienced vertebrologist or neurologist. These doctors will make an accurate diagnosis and prescribe effective and safe treatment. In Moscow, you can make an appointment with a neurologist or vertebrologist at our manual therapy clinic. The first appointment is completely free for all patients.
We offer to treat pinched intercostal nerve using affordable and effective techniques, including:
- manual traction of the spinal column, which allows you to quickly and without pharmacological drugs remove pressure from the nerve fiber and increase the intervertebral spaces;
- osteopathy – improves microcirculation of blood and lymphatic fluid, starts the process of regeneration of damaged nerve fiber;
- massage – improves the condition of muscles, ligaments and tendons;
- reflexology – with the help of acupuncture, the body’s hidden reserves are activated and the regeneration process is launched;
- physiotherapy – improves metabolism at the cellular level;
- Therapeutic gymnastics and kinesiotherapy restore the mobility of the human body.
The course of treatment is always developed individually. We invite you to sign up for a free initial consultation with a doctor right now.
Prevention
In order not to think about how to remove pinching in the thoracic spine, prevent pathology. Maintain good posture, keep your weight under control, lift weights correctly - do not bend over, but squat. If your work involves a computer or long periods of sitting at a desk, do exercises and breaks. In addition, you need to monitor your diet, adequate intake of vitamins and minerals, basic physical activity, and lead the healthiest lifestyle possible. In this case, it will be possible to maintain the health of the spine even in old age.
Treatment of intercostal neuralgia
Treatment of intercostal neuralgia usually consists of two stages. First, it is necessary to relieve the pain that accompanies intercostal neuralgia, then it is necessary to treat the disease that caused the nerve injury.
In the first week of the disease, it is better to observe bed rest for 1-3 days, preferably lying on a hard surface; it is best to place a shield under the mattress. To relieve pain, painkillers are prescribed, usually from the NSAID group, which not only relieve pain, but also have an anti-inflammatory effect. In addition, muscle relaxants are prescribed to relieve muscle spasms and sedatives. B vitamins (B1, B6, B12) are recommended - they help restore damaged nerve structures. During attacks, light, dry heat helps.
After the acute symptoms have been relieved, it is necessary to carry out a diagnosis and determine the cause that caused the attack of intercostal neuralgia. If this is any general disease (infectious, cold, allergic, diabetes, nervous system disease, depression), it is necessary to treat it.
If intercostal neuralgia is caused by a disease of the spine, that is, it is of a vertebrogenic nature, comprehensive treatment of the spine is recommended. To restore the correct physiological position of the thoracic and cervical spine in cases of intercostal neuralgia, courses of therapeutic massage, manual therapy, and physical therapy are conducted.
Physiotherapy, acupuncture, and laser therapy provide good results for vertebrogenic intercostal neuralgia. To prevent the disease from becoming chronic with frequent attacks, you need to reduce physical activity, not abuse alcohol, and avoid stressful situations if possible.
In the first week of the disease, it is better to observe bed rest for 1-3 days, preferably lying on a hard surface; it is best to place a shield under the mattress. During attacks, light, dry heat helps.
To relieve pain, take painkillers and sedatives. Physiotherapy, acupuncture, and laser therapy provide good results for intercostal neuralgia. It is advisable to take B vitamins (B1, B6, B12). To prevent the disease from becoming chronic with frequent attacks, you need to reduce physical activity, not abuse alcohol, and avoid stressful situations if possible.
To restore the correct physiological position of the thoracic and cervical spine in cases of intercostal neuralgia, courses of therapeutic massage, manual therapy, and physical therapy are conducted.
If conservative treatment does not help, then surgical treatment is performed (for example, osteochondrosis or disc herniation, which cause attacks of intercostal neuralgia).
Complications
The insidiousness of intercostal neuralgia is that its symptoms can be confused with many other diseases. Sometimes the patient is in no hurry to get an appointment and begins to treat intercostal neuralgia with ointments, tablets or herbs. For any form of the disease, even mild, the patient must be examined by a doctor. In no case should you independently diagnose yourself and prescribe treatment - the lack of medical intervention for serious diseases mistakenly mistaken for intercostal neuralgia can cost the patient’s life.
After identifying the cause of the disease, the doctor will prescribe adequate treatment to minimize the risk of complications.
The main complication of intercostal neuralgia is the transition of the disease to a chronic form with frequent exacerbations.
Anterior cutaneous nerve entrapment syndrome as a cause of abdominal pain
Abdominal pain or abdominal pain is a common reason for patients seeking medical help. Over a 5-year follow-up period, up to half of individuals experience abdominal pain.
There are several types of abdominal pain:
1) visceral - associated with damage to internal organs, most often the digestive organs. It is characterized by unclear localization, i.e. the pain zone only approximately corresponds to the affected zone. This pain is often associated with eating, defecation, etc.
2) parietal - occurs when the parietal peritoneum is involved in the process of inflammation. The pain is usually clearly localized, sharp, cutting, stabbing, and is accompanied by symptoms of peritoneal irritation.
3) referred pain - occurs when several zones are innervated by one segment of the spinal cord. For example, abdominal pain can occur with myocardial infarction.
4) projection pain - occurs when nerves are damaged, and the place of pain perception corresponds to the zone innervated by this nerve.
This article will discuss one of the diseases that is characterized by projection pain, namely anterior cutaneous nerve entrapment syndrome . It is also called rectus abdominis syndrome. In the English-language medical literature, the term ACNES is used (anterior cutaneous nerve entrapment syndrome, which translated into Russian means anterior cutaneous nerve entrapment syndrome), which we will use further in this article.
ACNES is one of the common causes of abdominal pain that remains unrecognized. On average, the prevalence of this syndrome is 1:1800-2000. In adolescents, one out of eight cases of chronic abdominal pain is caused by anterior cutaneous nerve entrapment syndrome. Up to 2% of cases of patients visiting a hospital emergency room with acute abdominal pain are caused by ACNES.
Pathogenesis of ACNES.
In ACNES, the lower thoracoabdominal intercostal nerves (Th8-Th12) are involved in the pathological process. They pass between the internal oblique and transverse abdominis muscles to the point where they reach the rectus abdominis muscles. Here the nerves turn to enter the rectus abdominis channels. It is assumed that compression of the nerves in the rotation zone is the leading mechanism for the development of ACNES. Pinching occurs due to muscle contraction, which can cause additional compression of the nerve, its ischemia, and, as a result, leads to severe pain.
Clinical picture of ACNES.
Pain (dull or sharp) is usually localized in a certain area - along the edge of the rectus abdominis muscle in the umbilical region or in the right hypochondrium. The pain is usually chronic, constant or frequent, less often in the form of individual episodes. The area of pain in most cases can be easily identified by palpation in the painful area. In rare cases, when the ilioinguinal and iliohypogastric nerves (Th12-L1) are pinched, the pain may have an atypical localization: in the iliac region and groin. Localization of pain in the right hypochondrium can simulate an attack of biliary colic.
The pain may vary depending on the person's posture, worsening when lying on the side of pain or sitting. Pain sensations are reduced when lying on your back. Coughing, laughing, bumpy driving, running, wearing tight belts and corsets, as well as exercise lead to increased abdominal pain.
Diagnosis of ACNES.
Diagnostic criteria for anterior cutaneous nerve entrapment syndrome include the following:
1) Unilateral localized pain in the abdominal wall lasting at least 1 month;
2) The presence of a unilateral painful area (“trigger point”) on the anterior abdominal wall measuring about 2 cm2, detected by pressing the index finger along the lateral border of the rectus abdominis muscle;
3) Positive Carnett's sign. Carnett's sign, named after the scientist who described it in 1926, involves the examiner identifying the exact location of maximum tenderness on the abdominal wall and asking the patient to elevate the head and/or torso with the arms crossed over the chest. Increased pain or persistent pain during this movement indicates that the cause of the pain is located in the abdominal wall (positive Carnett's sign). On the contrary, a negative Carnett symptom indicates another cause of pain (for example, pathology of the internal organs);
4) Positive “pinch” test: when fingers grasp a fold of skin and subcutaneous tissue, local pain is detected;
5) A change in the tactile sensitivity of the skin in response to a light touch and/or a change in the temperature sensitivity of the skin with a decrease in the perception of cold in the area of the most severe pain;
6) Normal laboratory data (no signs of inflammation or infection) in the absence of a surgical cause of pain;
7) Absence of pathology according to imaging studies (including ultrasound, computed tomography);
 A temporary reduction in pain by at least 50% after injection of a local anesthetic (usually lidocaine) at the trigger point.
A temporary reduction in pain by at least 50% after injection of a local anesthetic (usually lidocaine) at the trigger point.
Differential diagnosis of ACNES
The differential diagnosis includes various diseases in order to exclude other causes of chronic abdominal pain. The examination may reveal cicatricial changes in the skin, causing irritation and pinching of nerves, as well as hernias of the anterior abdominal wall (including those with signs of pinching).
In most cases, a thorough clinical and laboratory examination is required to exclude pathology of the abdominal organs.
Differential diagnosis with functional diseases of the digestive system, for example, irritable bowel syndrome (IBS) and functional abdominal pain, seems more difficult. Since there are no special research methods to diagnose these diseases, the doctor has to focus on typical clinical manifestations. Even ex juvantibus diagnosis (a diagnosis based on an assessment of the results of treatment) does not help, since therapy is not effective in all patients with IBS. The ACNES Questionnaire was developed to help differentiate functional bowel pain from pain caused by anterior cutaneous nerve entrapment syndrome. An index value of more than 10 points makes the diagnosis of functional abdominal pain unlikely.
ACNES therapy.
Treatment of anterior cutaneous nerve entrapment syndrome includes several approaches:
1) Systemic therapy - the use of non-steroidal anti-inflammatory drugs, weak opioid analgesics (tramadol), paracetamol, antiepileptic drugs (gabapentin) and antidepressants (amitriptyline). Unfortunately, therapy with these drugs, which often helps with other types of neuropathic pain, is usually ineffective in the case of ACNES.
2) Local therapy:
A. Trigger point injections. The trigger point in ACNES is the site of a pinched nerve, so injection of a local anesthetic into this area has both a therapeutic and (in complex cases) diagnostic effect. A 1% solution of lidocaine (10 ml) with or without the addition of steroid hormones is usually used as an anesthetic. The effect of treatment is defined as a reduction in pain severity by 50% or more, and the duration of the effect usually exceeds the half-life of the drug. The addition of steroid hormones may result in more durable pain relief, possibly due to their anti-inflammatory effects and attenuation of nerve excitation. However, their use is often associated with side effects, mainly abdominal muscle atrophy and systemic adverse reactions.
The blind method of administering anesthetic may result in an incorrect injection zone, as a result of which the use of ultrasound guidance has recently been recommended. The use of an ultrasound machine allows lidocaine to be injected precisely into the affected area, avoiding complications (entry into the abdominal cavity).
B. Chemical neurolysis. The literature describes the effect of 96% ethyl alcohol or 5-6% phenol solution for chemical destruction of pinched nerve fibers. However, there is no data on the long-term effectiveness and safety of this method.
B. Radiofrequency ablation is the treatment of nerves or nerve ganglia with high-frequency electrical impulses.
D. Ultrasound-guided injection of botulinum toxin into the trigger zone has been studied as an alternative technique, but there is no data on the long-term effectiveness of this method.
3) Surgery:
A. Laparoscopic anterior neurectomy - removal of a section of a pinched nerve.
B. Using a reinforcing polytetrafluoroethylene mesh over the problem area to prevent compression of the nerve.
Reasons for appearance
The pain may occur intermittently. Sometimes it is a regular spasm, and in some cases it is attacks of pain. Also, unpleasant feelings can begin during inhalation and exhalation, sudden body movements, such as coughing or sneezing. Doctors distinguish between primary and secondary causes of intercostal neuralgia.
Primary:
- problems with the spine. This may be loss of elasticity of the intervertebral discs, infection or inflammation in the roots and joints of the vertebra;
- incorrect posture. Also one of the primary reasons, it occurs in most people who lead an inactive lifestyle, constantly sit in one position, and slouch;
- rib fractures. This includes deformation of the thoracic region, its pathology or tumor.
Secondary causes include:
- hypothermia of the human body;
- long periods of sitting in drafts;
- infectious diseases associated with the lungs: pneumonia, tracheobronchitis;
- heart disease: myocardial infarction, ischemia, dissecting aortic aneurysm;
- problems with the mammary glands in women, such as swelling or inflammation;
- improper functioning of the gastrointestinal tract. For example, peptic ulcer, pancreatitis.
But the main and most common cause of intercostal neurosis is stress. People who are constantly stressed experience stiffness in their movements and muscle spasms. That is why any sudden movement causes pain and can provoke intercostal neuralgia.
Causes of pathology
The reasons for the development of neuralgia can be different: inflammatory processes, injuries, bacteria and viruses, poisoning with drugs and various substances, autoimmune diseases, circulatory disorders in the vessels supplying the nerve.
- infections such as shingles, Lyme disease, or HIV
- pressure on bone nerves, blood vessels or tumors
- kidney disease or diabetes
- age