Multiple sclerosis (MS) is a chronic progressive disease of the nervous system of unknown etiology, characterized by the development of diffuse demyelination and axonal degeneration [1]. It is classified as a multifactorial disease. This term refers to the combined effects of external and genetic factors, leading to the development of chronic inflammatory, demyelinating and neurodegenerative processes. Among external factors, special attention is currently paid to three risk factors for the development of MS: vitamin D deficiency, Epstein-Barr viral infection and smoking [2, 3]. Vitamin D deficiency has long been discussed as a risk factor for MS, but interest in it has increased dramatically in recent years.
The name “vitamin D” is given to a group of substances represented by more than 10 structural analogues. The main ones are vitamin D2, or ergocalciferol, and vitamin D3, or cholecalciferol. Vitamin D enters the body in two ways: with food and as a result of synthesis in the skin under the influence of ultraviolet rays. Absorption of vitamin D from food occurs in the duodenum and jejunum in the presence of bile acids. In the skin, under the influence of sunlight or ultraviolet radiation, previtamin D3 is formed from 7-dehydrocholesterol, which is immediately converted into vitamin D3 (cholecalciferol) under the influence of heat. Vitamin D formed in the skin and received from the intestines binds to a specific vitamin D-binding protein, which transports it to places of further metabolism. Part of vitamin D is transported to fat and muscle tissue, where it is fixed, representing a reserve form, but the main amount is transferred to the liver. In the liver, with the help of the enzyme 25-hydroxylase, vitamins D2 and D3 are converted into 25-hydroxyvitamin D [25(OH) D3], or calcidiol, the main circulating form of vitamin D. Then in the kidneys, calcidiol is converted into the active metabolite 1 by the enzyme α-hydroxylase ,25-dihydroxyvitamin D3 (calcitriol). This metabolite is recognized by tissues containing specific vitamin D receptors (VDRs), which are present in the skin, bones, muscles, gonads, intestines, central nervous system (CNS), microglia, activated monocytes, B and T lymphocytes, and dendritic cells. Calcitriol differs in structure and action from typical vitamins and is more reminiscent of a steroid hormone.
The main source of vitamin D is its formation in the skin under the influence of solar radiation (80%) and only 20% comes from food or supplements [4]. It is believed that short-term (for 10-30 minutes) solar irradiation of the face and hands is equivalent to taking 200 IU of vitamin D. The level of vitamin D synthesis in the skin is affected by latitude, time of year and day, air pollution, cloudiness, melanin content in the skin, use sunscreens, age, degree of openness of clothing.
The formation of previtamin D3 depends on the angle of incidence of sunlight. An increase in the angle of incidence due to the low position of the sun above the horizon, cloudiness, and environmental pollution determines the predominance of radiation with a longer wavelength. As a consequence, fewer ultraviolet photons reach the skin surface and stimulate vitamin D synthesis. Vitamin D production is virtually absent early in the morning and late afternoon and throughout the day during several winter months at latitudes above 35°. Therefore, living in northern latitudes is a risk factor for vitamin D deficiency. Those individuals who avoid sunlight, regardless of latitude, are also at risk for vitamin D deficiency at any time of the year. An unexpectedly high incidence of vitamin D deficiency was found in Miami [5]. It turned out that dark-skinned people need longer sun exposure to synthesize the required amount of vitamin D, since the epidermis of their skin contains large amounts of melanin, which competes with 7-dehydrocholesterol for the absorption of ultraviolet photons. In aging skin, the content of 7-dehydrocholesterol decreases, which reduces the synthesis of vitamin D in older people [6]. At age 70, vitamin D synthesis decreases by 75%. In addition, limited mobility, decreased renal production of 1,25-dihydroxyvitamin D, and reduced intake of vitamin D-fortified foods make it difficult to adequately provide vitamin D to older adults.
The level of 7-dehydrocholesterol in the skin of obese individuals is no different from that of non-obese individuals. However, subcutaneous fat creates reserves of vitamin D, due to which it is insufficient in the circulation in obese people [7].
Vitamin D levels are also affected by decreased bioavailability as a result of malabsorption, increased catabolism (when using anticonvulsants, glucocorticosteroids), decreased synthesis of 25-hydroxyvitamin D as a result of liver failure, loss of 25-hydroxyvitamin D in nephrotic syndrome, decreased synthesis of 1,25-dihydroxyvitamin D for chronic renal failure. A decrease in estrogen levels affects the activity of the enzyme α-hydroxylase, which leads to a decrease in the level of 1,25(OH)2D3 in postmenopause. Finally, women have generally lower vitamin D levels than men [8, 9]. During pregnancy and lactation, their need for vitamin D increases and is rarely compensated.
To date, debate continues regarding the optimal level of vitamin D in blood serum. Most experts believe that levels above 30 ng/mL (75 nmol/L) are adequate [10–12]. Existing recommendations declare that a serum vitamin D level of at least 75-90 nmol/L is necessary not only to optimize the metabolism of calcium and phosphorus, but also to prevent certain autoimmune diseases [13, 14]. Hypovitaminosis D is defined when the level of 25(OH)D3 in the blood serum is below 75 nmol/l (30 ng/ml), D-vitamin deficiency - at 50 nmol/l (20 ng/ml), and D-deficiency - at a level below 25 nmol/l (10 ng/ml). It is less clear what the upper level of vitamin D should be. According to the literature, a level of 150 to 200 ng/ml (375-500 nmol/l) can be considered safe [10].
In the absence of metabolic bone diseases such as rickets, osteomalacia, or osteoporosis, vitamin D deficiency is asymptomatic. Numerous studies show that the average vitamin D level in adult populations in all temperate countries where these studies were conducted is below the optimal value. For example, in the USA - 60 nmol/l (cohort of 18,558 people from 2000 to 2004) [15], 61 nmol/l - in France (cohort of 1,579 people) and in Canada [16, 17], 51 nmol/l l - in Great Britain [18]. In northern countries, vitamin D levels are even lower - for example, in Finland it was 44 nmol/l in summer and 24 nmol/l in winter (220 young men) [19]. In Russia, the first studies confirmed the presence of vitamin D deficiency both in children and adolescents (Yakutsk, Moscow, Vladivostok) and in the elderly (Moscow, Yekaterinburg) [20].
Vitamin D is the most important regulator of phosphorus-calcium metabolism, providing the necessary level of these elements for adequate osteogenesis. Calcitriol deficiency causes calcium malabsorption. A decrease in the level of calcium in the blood plasma and a decrease in the level of the active metabolite of vitamin D causes proliferation of parathyroid cells and an increase in the secretion of parathyroid hormone. Secondary hyperparathyroidism entails osteoclastic bone resorption, disruption of the processes of remodeling and mineralization of bone tissue, a decrease in its density and changes in bone architecture, which in turn leads to osteoporosis and an increased risk of fractures.
In addition to its well-known effects on calcium and phosphorus metabolism, vitamin D has other important effects, especially its anti-inflammatory, antiproliferative, and immunomodulatory effects. Considering the pathogenesis of MS, the following effects of vitamin D on the immune system may be of particular interest: the ability to modulate the differentiation and functional activity of antigen-presenting cells, thereby reducing the activity of potentially autoaggressive T lymphocytes [21-23], the ability to inhibit B-cell proliferation and T cell differentiation [24, 25], the ability to switch cytokine responses from pro-inflammatory Th1/Th17 to anti-inflammatory Th2 [26, 27], and finally, a mechanism to promote regulatory T cell differentiation and natural killer cell function [28, 29] . There is also evidence of the neuroprotective effect of vitamin D [30].
Other studies raise the question of genetic regulation of vitamin D metabolism in patients with MS. Of course, genetic factors influence vitamin D metabolism, which is regulated by more than 200 genes. The effects of calcitriol on the immune system may also be due to specific genes. Related to this is the suggestion that genes related to vitamin D synthesis may influence the risk of MS. Recently, it was shown that gene expression of the HLA-DRB1*1501 allele is modulated by vitamin D [31]. It has also been shown that the absence of functional variants in the CYP27B1
, which encodes an enzyme that converts 25(OH)D3 to its active form, is associated with an increased risk of MS [32].
The first hypotheses about the possible connection of MS with vitamin D deficiency arose from observations that confirmed that the risk of developing MS is associated with the latitude of residence [33, 34]. The prevalence of MS increases with distance from the equator. There is a hypothesis that latitude influences the risk of MS through the level of sun exposure and serum levels of vitamin D. However, recent studies show that the “latitude gradient” is being erased, which can be explained by a number of reasons, including better diagnosis of MS, changes in lifestyle, improved sanitary living conditions [35]. Most of the findings about the beneficial role of vitamin D in MS come from the fact that the risk of MS and its activity are associated with the time of year. As shown in a number of studies, people born in the spring have a significantly higher risk of developing MS than those born in the fall [36-39]. This can be partly explained by the fact that in the first case, most of the pregnancy took place during the period of low insolation (October - March), and in the second case, during the period of high insolation (April - September). Based on a study of 136 cases and 272 controls in Tasmania, the risk of MS was found to be lower in those who spent more time in the sun during holidays and weekends during childhood than in those who were protected from sun exposure ( p
<0.01) [40]. An inverse correlation between MS risk and past exposure to insolation has also been found in other studies [41, 42]. Finally, 79 pairs of monozygotic twins, one of whom had MS, were examined in the United States. Both twins differed only in the degree of sun exposure in childhood. Twins without MS had significantly more exposure to sun in the past [43]. However, all of these studies regarding the relationship between the level of insolation received in childhood and adolescence and the risk of MS in the future have a number of limitations. First, retrospective assessment of the duration of insolation in the past is difficult [36]. Also, when studying the level of insolation, it is necessary to remember that the relationship between the amount of vitamin D formed and the level of insolation is not direct. In addition, there is evidence that insolation has an immunomodulatory effect independent of vitamin D [44, 45].
Only one study has directly analyzed MS risk based on serum vitamin D3 levels in healthy individuals several years before their MS onset [46]. They studied 257 cases of MS among young American soldiers who had at least one blood serum sample taken before the onset of neurological symptoms. The control group consisted of 514 people. Whites were divided into 5 subgroups based on serum vitamin D levels: the subgroup with the highest vitamin D levels (99–152 nmol/L) had a significantly lower risk of MS than the subgroup with the lowest levels (15–63 nmol/L). , p
<0.01). For whites, the risk of MS decreased by 41% for every 50 nmol/L increase in vitamin D levels (OR=0.59; 95% CI 0.36-0.97). No statistically significant differences were obtained for the black group.
The study concluded that high vitamin D levels are associated with a lower risk of MS in white people. Based on this study, A. Ascherio and K. Munger [3] believe that almost ⅓ of MS cases can be avoided if serum vitamin D levels are maintained at around 100 nmol/L during childhood and adolescence. One of the latest studies suggests that vitamin D levels in utero
, which is entirely dependent on maternal vitamin D levels, influences the risk of subsequently developing MS [47]. A Canadian study of children experiencing a first demyelinating episode found that the risk of developing definite MS over the next 3 years was inversely and independently correlated with 25(OH)D3 levels [48].
Other studies have looked at vitamin D levels directly in MS patients. According to various researchers, the prevalence of vitamin D hypovitaminosis in patients with MS ranges from 17.0 to 86.7% [49, 50].
Thus, a relatively old American study showed that 80 hospitalized women with MS (average EDSS score 7.2) had a very low average level of 25-hydroxyvitamin D, but the low physical activity of these patients could to some extent explain the results [ 49]. At the same time, a number of studies have not found a statistically significant difference in the serum level of 25(OH)D3 in MS patients and controls. Thus, in a Finnish study of a group of 40 patients at the onset of MS, there was no difference in 25(OH)D3 levels between them and 40 control subjects if the samples were studied in winter. However, patients with MS had significantly lower levels of 25(OH)D3 in the period from June to September [51]. In another study, also conducted in Finland, vitamin D deficiency was detected with the same frequency (50%) in the patient group and in the control group. At the same time, seasonal variations in 25(OH)D3 were similar in patients and controls, but vitamin D levels were lower in patients during MS exacerbations [52].
In 2008, 267 MS patients were examined in the Netherlands. 25(OH)D3 levels were significantly lower in progressive forms of MS compared to relapsing-remitting MS. The same study showed that low 25(OH)D3 levels are associated with high EDSS scores [53]. However, it should be added that although a number of researchers have found an inverse correlation between vitamin D levels and disability scores on the EDSS scale, nevertheless, a significant proportion of patients with vitamin D deficiency have slight disability [54]. Although disability, reducing the ability to go outside, along with the systematic avoidance of heat and sun by these patients, can increase hypovitaminosis D.
J. Corrale et al. [55] conducted a study of vitamin D levels in 132 patients with different types of MS and stage of the disease and 60 controls. All subjects lived in Buenos Aires (Argentina) at latitude 34 in the southern hemisphere. The level of 25(OH)D3 was significantly lower in patients with relapsing-remitting MS (47.3±9.0 ng/ml in remission and 38.5±8.7 ng/ml in exacerbation) than in healthy controls (61.2±5.6 ng/ml). It was also demonstrated that during the period of exacerbation the level of vitamin D was significantly lower than in the remission stage. In patients with primary progressive MS, vitamin D levels did not differ from those in the control group and amounted to 52.2±6.5 ng/ml. The authors explain this difference in vitamin D levels in relapsing-remitting and primary progressive MS by the features of the pathogenesis and morphology of these two fundamentally different forms of MS.
A study of vitamin D levels in MS patients in Russia using the example of the Sverdlovsk region also established a high incidence of vitamin D hypovitaminosis both among MS patients and healthy volunteers. However, in patients with MS, vitamin D deficiency was more common and more pronounced. The magnitude of the decrease in 25(OH)D3 levels did not correlate with any of the MS characteristics studied, but was more pronounced in younger patients. There was a tendency for vitamin D3 concentrations to decrease during MS exacerbations [56].
As is known, depression and fatigue are common symptoms in MS; they are also associated with hypovitaminosis D. A study of depression and fatigue in 59 MS patients was conducted in the Netherlands in 2010 [57]. Vitamin D levels were negatively correlated with depression levels ( r
=–0.326,
p
=0.006). No such correlation was found for fatigue. The authors conclude that vitamin D deficiency may contribute to the presence of depressive symptoms in MS, although this requires confirmation.
Recent studies demonstrate a clear connection between MS activity and vitamin D concentrations. Thus, 2 studies showed that each increase in 25(OH)D3 levels by 10 nmol/l led to a decrease in the frequency of exacerbations by 11.0 and 13.7%, respectively [58, 59]. Another study [60] found that for every doubling of serum vitamin D levels, the incidence of exacerbations decreased by 27.0%.
When studying the level of vitamin D in the cerebrospinal fluid in patients and controls, no significant differences were obtained, and no differences were found in studies in the stages of remission and exacerbation [61].
Experimental studies show that vitamin D prevents the development of experimental autoimmune encephalomyelitis and markedly improves clinical symptoms in affected mice [62–65]. However, this effect is more pronounced in females, possibly due to the enhanced effect of vitamin D by estrogens [66].
To date, several clinical studies have been conducted on the use of vitamin D in the treatment of MS, although the quality of some of them is questionable.
In one of the early studies, P. Goldberg et al. [67], using vitamin D (5000 IU per day in the form of cod liver oil) in 16 patients for 2 years, noted a 60% reduction in the frequency of MS exacerbations. A Canadian study demonstrated the use of high doses of vitamin D3 (cholecalciferol, 14,000 units per day) over a long period (6 months - 1 year) without the development of hypercalcemia or other significant side effects, despite achieving vitamin D3 levels of about 400 nmol/L. After 1 year of such treatment, there was a 41% reduction in the number of exacerbations and a significant improvement in the EDSS scale in treated patients [68].
Two recently published randomized, double-blind, placebo-controlled studies conducted in Finland [69] and Norway [70] using 20,000 IU vitamin D per week gave conflicting results. In a Finnish study, the mean 25(OH)D3 value in patients receiving vitamin D for 1 year in addition to interferon β increased to 110 nmol/L, and patients in the drug group had significantly fewer Gd-accumulating lesions. At the same time, there was a tendency to reduce the accumulation of disability and improve walking parameters. The annual rate of exacerbations was the same in both the drug and placebo groups.
In a 96-week Norwegian study, there was no difference between the groups in the annual frequency of exacerbations, EDSS, and MSFC scales, although the median D3 concentration in the group receiving vitamin therapy reached 121 nmol/l.
Due to the rather uncertain results of clinical studies published to date, it is impossible to answer the question of whether vitamin D can be used to treat MS. Well-designed clinical studies are currently underway that may help clarify this issue. Regarding the safety of high doses of vitamin D, this data already exists. Treatment of MS patients with high doses of vitamin D is safe [71–73].
Thus, numerous studies show that the majority of patients with MS have vitamin D deficiency. An association has been identified between vitamin D deficiency and disease process activity. Further research is needed to definitively prove the link between vitamin D levels in the body and the risk of developing MS. Although the effect of vitamin D in the treatment of MS is currently unproven, from a purely medical point of view it cannot be ignored that vitamin D deficiency is generally detrimental to the health of these patients. Although there are no practical recommendations, it is nevertheless advisable to screen individuals at risk for MS for vitamin D levels in their blood serum. In case of vitamin D deficiency, its level should be increased to 30-40 ng/ml (75-100 nmol/l).
The relationship between vitamin D and multiple sclerosis
The exact causes of multiple sclerosis (MS) are not yet fully understood. Recently, however, there are increasing indications that vitamin D deficiency may be a key factor in the development of multiple sclerosis. New therapies have also shown that multiple sclerosis can be significantly improved with high doses of vitamin D and even reversed.
In this article, we want to look at the relationship between vitamin D and multiple sclerosis from different perspectives:
- Vitamin D connection with MS: sun, ultraviolet radiation and vitamin D levels;
- Therapeutic success with vitamin D;
- Mechanisms of action of vitamin D in MS;
- Coimbra Protocol.
Sun damage and multiple sclerosis
Exposure to ultraviolet radiation in childhood and adolescence may be a decisive factor for the development of MS.
A Tasmanian study concluded that sun exposure in children aged 6 to 15 years, in particular, significantly reduces the risk of multiple sclerosis.
Studies of identical twins have shown that the risk of multiple sclerosis decreases markedly with increasing sun exposure during childhood. This also proves that genetic factors may not be solely responsible for multiple sclerosis. Other studies have failed to find age-related associations with MS.
How far the effects of ultraviolet radiation can go was examined in studies that showed a strong link between the season of pregnancy and the incidence of multiple sclerosis in old age. Spring births (i.e. fall and winter pregnancies) have a significantly higher risk of developing MS. A possible mechanism of action is also known: vitamin D deficiency in the mother during pregnancy significantly changes the structure of the child's brain. The observed changes may occur in many MS patients, but this does not prove a cause-and-effect relationship.
In summary, studies have shown that good UV coverage significantly reduces the risk of multiple sclerosis, but periods of UV deficiency significantly increase the risk.
It is not yet clear whether time in the womb and during childhood is critical. However, today it is more likely that long-term ultraviolet deficiency is always a risk factor.
Vitamin D levels and multiple sclerosis
Analyzing the relationship between multiple sclerosis and vitamin D levels is more complex than one might expect. In principle, MS patients often have noticeably low levels of vitamin D. However, this is not so significant because there may be reverse causation - for example, because sufferers spend less time outdoors.
In addition, it is sometimes suggested that vitamin D levels play a major role in childhood and adolescence, and that, in general, longer periods of insufficient vitamin D intake are critical. Random measurements of vitamin D levels in later life are only reproducible and therefore don't have much meaning in this context.
Thus, the exact relationship between MS and vitamin D levels can be confirmed without a doubt by long-term studies with regular measurement of vitamin D levels. Such studies do not exist, to our knowledge.
A related study found that blood donor databases demonstrated a strong association of vitamin D levels in young adulthood with late-onset MS.
High levels of vitamin D at a young age reduce the risk of developing MS by an impressive 84-97%.
Some studies have also shown similar figures for vitamin D levels between mothers and young children.
Vitamin D levels and progression of multiple sclerosis
As it turned out, vitamin D levels affect not only the development, but also the course of multiple sclerosis. Several studies have shown that the higher the vitamin D level, the less frequent and safer the relapses were. At 10 ng/ml serum 25-OH-vitamin D, the relapse rate was reduced by up to 30 percent.
Vitamin D levels can also predict the occurrence and severity of new lesions on MRI, as a 2012 study found: Vitamin D levels were inversely associated with MS activity on MRI. The higher the vitamin D level, the lower the MS activity.
These results strongly support a causal role for vitamin D, which should now be explored through intervention studies, i.e. treating MS patients with vitamin D.
Multiple sclerosis and the sun: geographical distribution
A link between vitamin D and multiple sclerosis has long been suspected. This theory was first created in the 70s. Today there is a lot of evidence for this theory.
The starting point was the observation that the incidence of MS spreads across latitude and UV index: the incidence of multiple sclerosis increases from the equator to the two poles. This corresponds to the intensity of sunlight and, therefore, to the body's supply of vitamin D. The frequency of new cases and relapses increases in the dark season.
This theory was made even more plausible by observing that the geographic distribution of MS there was lower than predicted, where fish intake - and therefore vitamin D - was particularly high. Migration from northern to more southern areas has also been shown to significantly reduce the risk of multiple sclerosis.
Causes of multiple sclerosis
The exact origin of multiple sclerosis is not yet known. It is generally believed that a combination of several factors causes a disease outbreak. These include, in particular:
- Genetics;
- Vitamin D level;
- Infectious diseases (for example, Eppstein-Barr virus).
MS is an autoimmune disease in which the body's immune system attacks its own tissues. Almost all of the genes that have been studied in connection with an increased risk of MS affect the immune system. The strongest correlation is shown by the HLA genotype of HLA-DRB1.
Other central factors—vitamin D and infections—influence the immune system, so immune dysregulation is now considered a fundamental mechanism in multiple sclerosis.
It is also often assumed that the above-mentioned developmental factors took effect many years before the onset of multiple sclerosis. Most cases of multiple sclerosis occur at a young age, so some researchers suspect that the disease begins in childhood or adolescence.
Thus, genetic predisposition in combination with various other factors appears to cause multiple sclerosis. The current thesis is that vitamin D levels are critical in this context.
What is multiple sclerosis?
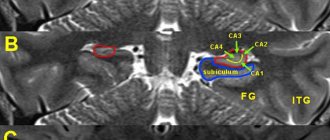
MS is a chronic inflammatory disease that affects the central nervous system. The nerve-protective layer myelin (also: “medullary sheath”) is attacked, resulting in partial or complete loss of nerve function. Symptoms can occur almost anywhere, depending on where in the central nervous system MS becomes noticeable.
Multiple sclerosis is an autoimmune disease characterized by multiple, diffuse, inflammatory demyelination in the white matter of the brain and spinal cord, which is caused by the body's own defense cells attacking the myelin sheaths of nerve cells. Active foci of inflammation in the brain and nervous system are also shown by corresponding plaques in imaging procedures (magnetic resonance imaging).
Proof of the UV theory
Finally, evidence for the UV theory was provided by a 2011 study that used ultraviolet values measured by satellites to show that the higher the level of sunlight, the lower the incidence of MS. The real UV index predicted MS incidence even 20 times more accurately than by latitude alone. UV-induced skin aging, a marker of lifetime sun exposure, also strongly predicts the risk of multiple sclerosis.
Thus, the connection between multiple sclerosis and exposure to ultraviolet radiation has been proven. However, this has not clarified whether vitamin D produced by ultraviolet radiation or other effects of ultraviolet radiation, independent of vitamin D, are responsible for this relationship. To do this, a direct link between MS and vitamin D levels must be proven.
Can Vitamin D Treat Multiple Sclerosis?
A key question for people with multiple sclerosis is whether vitamin D can help with multiple sclerosis.
At the same time, it is definitely known that vitamin D has a preventive function: the risk of multiple sclerosis increases with a decrease in vitamin D intake, and the severity of symptoms decreases with increasing vitamin D levels.
The therapeutic use of vitamin D has been very promising in research, but has generally been only partially successful. Only a very high dose protocol (the Coimbra protocol) was able to achieve complete remission of MS with vitamin D.
The purpose of this article is to track the progress of vitamin D research in MS and provide a comprehensive picture of the current state of research (2018).
It is important!
- Numerous studies support the causative role of vitamin D in MS;
- Vitamin D can relieve symptoms of multiple sclerosis and even stop them;
- Good results can only be achieved with doses of 14,000 IU per day;
- Patients with MS require individualized vitamin D dosage adjustments and very high vitamin D levels;
- An alternative treatment concept achieved with vitamin D has a 95% success rate in reversing multiple sclerosis with high doses of vitamin D.
- In addition to vitamin D, other nutrients play an important role in MS.