Hippocampal sclerosis or Ammon's horn sclerosis, or medial temporal sclerosis is a set of changes characterized by a decrease in the volume of nervous tissue and loss of neurons in the medial temporal lobe. Clinically, hippocampal sclerosis manifests itself as epilepsy, often uncontrollable with medications, but in a significant number of cases curable with surgery.
The very first macroscopic description of a densified and reduced volume of the hippocampus in patients with epilepsy was made in 1825 by Bouchet and Cazauvieilh. In 1880, Sommer first described the microscopic picture of the sclerotic hippocampus in epilepsy, including noting that the loss of neurons in the hippocampus is segmental in nature, and the greatest loss of neurons occurs in the Sommer sector or CA1 segment of the hippocampus. A clinical description of epileptic seizures in patients with temporal lobe pathology was made by Hughlings Jackson in 1885, and in 1935 Stauder identified a connection between FH and the clinic of temporal lobe epilepsy. Sano and Malamud in 1953 confirmed the connection of hippocampal sclerosis with electroencephalographic signs of temporal lobe epilepsy. In the 50s of the 20th century, with the development of epilepsy surgery, intravital diagnosis of FH became possible. This is how Penfield described the so-called incisural sclerosis - thickening of the hippocampus, amygdala, and uncus, which was noted intraoperatively during surgery for temporal lobe epilepsy. Falconer proposed temporal lobectomy (removal of the anterior 2/3 of the temporal lobe neocortex and medial structures) for the treatment of temporal lobe epilepsy, with the most common histological diagnosis in his series of patients being hippocampal sclerosis. Later, more selective surgical techniques were proposed, which consisted in removing only the medial structures of the temporal lobe.
Today, hippocampal sclerosis is the most common histological diagnosis in adult patients undergoing surgery for epilepsy. The hippocampus is located in the medial parts of the temporal lobe and consists of two bent strips of nervous tissue nested inside each other: the dentate gyrus and the hippocampus itself (Ammon's horn or cornu Ammonis (CA)). In histological terms, the hippocampal cortex belongs to the archicortex, represented by three layers of neurons. The outermost layer of the hippocampus, forming the medial wall of the temporal horn of the lateral ventricle, is called the alveus and is formed by axons emerging from the hippocampus. This is followed by the stratum oriens (represented by axons and interneurons), then the layer of pyramidal cells, which are the main cellular elements of the hippocampus, and finally the deepest layer of the stratum lacunosum and moleculare, represented by dendrites, axons and interneurons. Important for understanding the various types of damage to the horn of Ammon during its sclerosis is the division of the pyramidal layer into 4 sectors proposed by Lorente de No (CA1, CA2, CA3 and CA4). The most pronounced layer of pyramidal cells is located in the CA1 sector, which continues into the part of the parahippocampal gyrus called the subiculum. The CA4 layer is adjacent to the concave part of the dentate gyrus. The dentate gyrus is a C-shaped structure with three layers of cells: the outer molecular, middle granular and inner layer of polymorphic cells, which merge with the CA4 layer of the hippocampus.
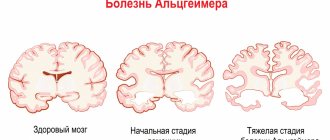
Structural changes in hippocampal sclerosis can vary from minimal, limited to one of its SA sectors, to severe, extending beyond the medial temporal lobe. The description of pathological changes in the structure of brain tissue in hippocampal sclerosis is distinguished by an exceptional variety of terms and the presence of several classifications with different concepts describing the same histological substrate.
Histological structure of the sclerosed hippocampus
Macroscopically, the sclerotic hippocampus is reduced in volume and dense, and among the main microscopic characteristics are a decrease in the number of pyramidal cells in various SA layers and a variable degree of gliosis. In the granular layer of the dentate gyrus, varying degrees of reduction in neuronal density may be observed, although in general its structure is more preserved compared to the SA layers. Also a distinctive histological feature is that the loss of neurons does not extend beyond the SA layers to the subiculum, which distinguishes hippocampal sclerosis from its atrophy during ischemic damage and neurodegenerative diseases. It was noted that loss of neurons in the pyramidal layer of the hippocampus can occur in several ways, which was the basis for the formation of the classification of this pathology. The most widely used classification of hippocampal sclerosis was created by the ILAE commission. In type 1 HS (severe or classic), neuronal loss is observed in all layers of the hippocampus; type 2 is characterized by loss of neurons predominantly in the CA1 layer; and in type 3 HS, only the CA4 layer is affected in the area of the transition to the dentate gyrus (so-called end folium sclerosis). In the literature, along with the term hippocampal sclerosis, a number of definitions often appear that emphasize that histological signs of the disturbed structure of brain tissue can extend beyond the hippocampus.
Thus, the term “mesial temporal sclerosis” takes into account the fact that, along with the hippocampus, atrophic and gliotic changes are observed in the amygdala and habenula. When analyzing the histological material obtained during surgery for temporal lobe epilepsy, it became obvious that sclerosis of the hippocampus is accompanied by pathohistological changes in the lateral neocortex of the temporal lobe. Thom proposed the term “temporal sclerosis”, which defines neuronal loss and gliosis in layers 2-3 of the temporal cortex. Quite often, heterotopic neurons are detected in the neocortex in the 1st layer of the cortex and white matter, which is referred to as “microdysgenesis.” In 2011, the ILAE Commission presented a new classification of focal cortical dysplasias, where a group of FCD type 3a was identified, when hippocampal sclerosis can be combined with dysplasia of the temporal lobe cortex in the form of a violation of its laminar structure, which in turn is classified as FCD type 1. Microdysgenesis, the role of which in epileptogenesis is not yet known, are classified as so-called small malformations of the cerebral cortex and, when identified with hippocampal sclerosis, the diagnosis is defined as FCD type 3a. Just like FCD 3a, a combination of temporal sclerosis and hippocampal sclerosis is considered. The concept of “dual pathology” is often encountered in the literature, when hippocampal sclerosis is combined with a potentially epileptogenic lesion of the neocortex, including outside the temporal lobe, for example, a tumor, vascular malformation, FCD type 2, Rassmussen’s encephalitis, gliotic scar. At the same time, the concept of “double pathology” does not include FCD type 3a. The terminology becomes even more complex, since the presence of two epileptogenic brain lesions, but without hippocampal sclerosis, is designated as double pathology.
To understand the connections between different parts of the hippocampus and the pathogenesis of HS, it is necessary to have an idea of the structure of the polysynaptic intrahippocampal pathway, which starts from the neurons of layer 2 of the entorhinal cortex (located in the anterior part of the parahippocampal gyrus and in the area of the uncus). The processes of these neurons form a perforant path, which goes through the subiculum of the parahippocampal gyrus into the dentate gyrus and contacts the dendrites of the cells of the granular layer. Neurons of the granular layer form mossy fibers that innervate CA3 and CA4 pyramidal neurons, which in turn contact the CA1 layer through lateral axons, the so-called Schaffer collaterals. Abnormal growth of mossy fibers instead of the SA layers into the dentate gyrus with the formation of excitatory synapses is considered one of the pathogenetic links in HS. From the above SA layers, axons enter the alveus and then into the fornix through the hippocampal fimbria. Taking into account the anatomical and functional connection between Ammon's horn, dentate gyrus, and subiculum, a number of authors have designated them the term “hippocampal formation.”
Causes of hippocampal sclerosis
The central question of the etiology of FH is to clarify what occurs primarily: structural pathology of the hippocampus, which triggers chronic drug-resistant epilepsy, or, conversely, long-term pathological electrical activity leads to sclerosis over time. It is important to note that a significant proportion of patients with risk-related epilepsy associated with HS experience febrile seizures or other acute pathology of the central nervous system (trauma, anoxia, neuroinfection) in early childhood, which is referred to as initial precipitating damage. The acquired nature of HS is supported by those rare observations when this pathology occurs in one of the monozygotic twins, the second twin does not have sclerosis, and, therefore, the genetic factor is not paramount. However, hereditary familial forms of temporal lobe epilepsy (for example, a group of epilepsies associated with mutations in the SCN1a and SCN1b genes encoding sodium) indicate that a genetic factor also plays a role, causing hippocampal sclerosis in some of these patients without a history of febrile seizures . Speaking about the acquired nature of the disease, it should also be taken into account that not every type of seizure is associated with the development of FH: autopsy data indicate that long-term uncontrolled epilepsy with frequent generalized seizures does not lead to neuronal loss in the hippocampus, as does afebrile status epilepticus. On the other hand, febrile status epilepticus is accompanied by MRI evidence of hippocampal edema. The answer to the question of how often the status of febrile seizures in a child is realized in FH and drug-resistant epilepsy may be provided by the prospective study FEBSTAT. It has already been established that out of 226 children after febrile seizure status, 22 had MRI signs of hippocampal edema, most pronounced in the Sommer sector (CA1). Of these 22 patients, repeat MRI at various times was performed in 14; in 10 cases, signs of hippocampal sclerosis were detected. However, out of 226 children, epilepsy was diagnosed in only 16 patients and in most cases it was non-temporal epilepsy. That is, on the one hand, febrile status does not always lead to epilepsy with hippocampal sclerosis, on the other hand, the time interval between precipitating brain injury and the appearance of temporal lobe epilepsy can be more than 10 years, and the study does not yet have a follow-up of such a duration. Genetic studies also indicate that the etiology of FH is heterogeneous. Genome-wide association studies have shown that febrile seizures with hippocampal sclerosis may be a genetic syndrome, as they are associated with the presence of a specific allele of a single nucleotide sequence located near the sodium channel gene SCN1A. This association was not found for cases of epilepsy with FH without febrile seizures. The consensus opinion of epileptologists is that there is a certain initial genetic predisposition, which is realized in hippocampal sclerosis in the presence of a certain damaging factor (double hit hypothesis).
Prevention measures
In order to reduce the occurrence of seizures, you must constantly take anticonvulsant medications prescribed by your doctor, and you must also:
- maintaining a sleep schedule;
- following a diet that limits the consumption of liquid and salt, as well as salty, spicy and fried foods;
- avoiding alcohol intake;
- smoking cessation;
- avoid hypothermia and overheating;
- excluding coffee and tea.
By following these recommendations, you can minimize the risk of occurrence or exacerbation of the disease.
Pathogenesis of hippocampal sclerosis
Hippocamal sclerosis has two fundamental pathological characteristics: the first is a sharp decrease in the number of neurons and the second is hyperexcitability of the remaining nervous tissue. One of the key roles in epileptogenesis in HS is played by the sprouting of mossy fibers: abnormal axons of granular cells, instead of innervating the SA cells of the hippocampus, reinnervate the molecular neurons of the dentate gyrus through excitatory synapses, thus creating local electrical circuits capable of synchronizing and generating an epileptic seizure. An increase in the number of astrocytes, gliosis may also play a role in epileptogenesis, because altered astrocytes cannot sufficiently reuptake glutamate and potassium. Proinflammatory cytokines, such as IL-1β, IL 1, TNFa, can also act through the mechanism of increasing glutamate release and decreasing reuptake, GABA inhibition. In this regard, the role of herpes virus type 6, the DNA of which is found in the brain tissue of patients with temporal lobe epilepsy, is discussed in the pathogenesis of FH.
Clinic and diagnostics
The history of epilepsy due to hippocampal sclerosis is described mainly on the basis of numerous studies evaluating the effectiveness of surgical treatment of temporal lobe epilepsy. A frequent event in the anamnesis is an indication of an acute pathology of the central nervous system suffered in childhood (usually up to 5 years): febrile seizure status, neuroinfection, head injury. Stereotypical seizures begin between the ages of 6 and 16 years, and there may be a so-called latent period, which is determined by the time between the initial precipitating damage and the development of the first seizure. It is also not uncommon for situations when between the first seizure and the development of pharmacoresistance, a period passes, designated as “silent”. This feature of the course of the disease indicates its progressive nature. A characteristic cognitive deficit in FH may be memory loss, especially during uncontrolled attacks.
Diagnosis of epilepsy caused by hippocampal sclerosis is based on three main principles. The first is a detailed analysis of the sequence of symptoms in an epileptic attack or semiology, which depends on which areas of the brain the epileptic activity spreads to. The second is the analysis of EEG data and their comparison with the semiology of the attack and the third is the identification of epileptogenic lesions on MRI. Speaking about the semiology of an attack in temporal lobe epilepsy associated with HS, it is necessary to remember that, firstly, each of the symptoms individually is not specific, although there is a typical pattern in the course of an attack. Secondly, symptoms in a seizure appear when epileptic activity spreads to parts of the brain associated with the hippocampus, which itself does not produce clinical manifestations. The characteristic onset of a temporal lobe attack is an aura in the form of a rising sensation in the abdomen. Fear or anxiety is also possible if the amygdala is involved at the beginning of an attack. At the beginning of the attack, there may be a feeling of “already seen” (déjà vu). An alarming diagnostic aura is an aura in the form of dizziness or noise, which may indicate an extrahippocampal onset of an attack. The preserved ability to name objects and speak during an attack is an important lateralizing sign of damage to the non-dominant hemisphere. The change in consciousness is accompanied by a cessation of activity, while the patient has a frozen gaze with eyes wide open (staring). The next symptom after the aura and cessation of activity are automated actions: oroalimentary automatisms with chewing, smacking lips. Dystonia in the hand also often occurs on the contralateral side of the sclerosed hippocampus, which is associated with the spread of epiactivity to the basal ganglia and manual automatisms also appearing in the form of fingering objects with the hand in the ipsilateral hand. Among the lateralizing symptoms, postictal paresis, which indicates involvement of the contralateral hemisphere, and postictal aphasia with damage to the dominant hemisphere are important. These symptoms must be considered in the context of EEG data.
The basis of electroclinical diagnosis for hippocampal sclerosis is videoEEG monitoring, which consists of simultaneous video recording of an epileptic seizure and electrical activity of the brain. VideoEEG monitoring solves several problems: 1. It allows you to exclude pseudo-seizures and non-epileptic paroxysms, including when they are combined with actual epilepsy 2. It allows for a detailed assessment of the semiology of the attack and its comparison with the dynamics of seizure epiactivity: its lateralization and regional localization, 3 Long-term recording makes it possible to clarify the lateralization and localization of interictal activity. The most successful option in terms of a favorable outcome of epilepsy surgery is the coincidence of lateralizing and localizing symptoms in an attack with the data of the ictal and interictal EEG and MRI picture. A pressing issue in presurgical evaluation is how long videoEEG monitoring should be carried out. It is known that the probability of registering a paroxysm on a 30-minute EEG with a frequency of attacks once a week is about 1%, and long-term videoEEG monitoring with an average duration of 7 days does not reveal interictal activity in 19% of patients. An acute question in the presurgical examination for temporal lobe epilepsy concerns the required duration of video-EEG monitoring: is it a strict requirement to record ictal events on the EEG or can the decision about surgery be made based on the analysis of interictal activity. A number of epileptologists believe that with a characteristic clinical picture and history of the disease, the presence of hippocampal sclerosis on MRI, registration of an ictal event is not necessary when there is more than 90% lateralization of interictal epiactivity in the temporal region on the affected side on MRI. In most cases, the resolution of the scalp EEG is sufficient to correctly lateralize the seizure onset zone in temporal lobe epilepsy and, in the context of seizure semiology and MRI data consistent with it, to determine a surgical treatment strategy.
MRI diagnosis of hippocampal sclerosis is the next fundamental stage of presurgical examination and should be performed according to an epileptological protocol, the main characteristics of which include small slice thickness and high magnetic field strength. The optimal condition for epileptological MRI is the interaction between the epileptologist and the radiologist, when the planning of the study is carried out taking into account the expected localization of the epileptogenic zone. Hippocampal sclerosis on MRI has characteristic signs: a decrease in the volume of the hippocampus and disruption of the structure of the SA layers, a hyperintense signal in T2 and FLAIR mode. Atrophic changes are often detected in the ipsilateral amygdala, pole of the temporal lobe, fornix, and mammillary body. The purpose of high-resolution MRI also includes the detection of other epileptogenic pathology of the brain located outside the hippocampus, i.e., dual pathology, for example, focal cortical dysplasia, which makes a non-epileptological MRI study insufficient for making a decision about surgery, even if it reveals signs of hippocampal sclerosis.
Decoding the results
After all the images are received, the doctor’s task is to correctly interpret them and make a diagnosis. Using magnetic resonance imaging, you can find out the exact dimensions of a given part of the brain and identify even minimal changes in the structures of the hippocampus and neighboring areas. Detailed photographs of this area of the brain of the organ give your doctor the opportunity to determine the diagnosis and treatment tactics.
We recommend seeking medical help as soon as the first warning signs appear. Be healthy!
MRI anatomy of normal and sclerotic hippocampus
A-T2 coronal section: sclerosis of the right hippocampus, a decrease in its volume is determined, the absence of internal structure compared to the left hippocampus. B – the same section with explanations. The red line outlines the hippocampi (a decrease in the volume of the right hippocampus is visible), and the blue line outlines the subiculum on the left. The yellow line in the center of the hippocampus is drawn along the deep part of the hippocampal sulcus (in Figure A, this sulcus is not identified in the right hippocampus). FG – fusiform gyrus, ITG – inferior temporal gyrus. C – FLAIR coronal section showing decreased volume and hyperintense signal from the right hippocampus.
A fundamental point in understanding the electrophysiology of medial temporal lobe epilepsy is the fact that the scalp EEG itself does not reveal epiactivity in the hippocampus, which has been demonstrated in numerous studies using intracerebral electrodes, i.e. for the appearance of epiactivity on the scalp EEG in the temporal region, its distribution is required from the hippocampus to the adjacent temporal lobe cortex. At the same time, the main clinical manifestations of an attack in medial temporal lobe epilepsy are associated with the spread of epiactivity outside the hippocampus: déjà vu is associated with excitation of the entorhinal cortex, a feeling of fear - with the amygdala, abdominal aura - with the insula, oroalimentary automatisms with the insula and frontal operculum, dystonia in the contralateral arm - with the spread of excitation to the ipsilateral basal ganglia. These anatomical and electrophysiological features may cause the patient to have seizures that are very similar to temporal paroxysms, but actually have an extrahippocampal and extratemporal onset. As experience in the surgical treatment of temporal lobe epilepsy accumulated, it became obvious that removal of the medial structures of the temporal lobe makes it possible to get rid of seizures completely in 50–90% of patients, but in some cases the frequency of seizures does not change at all. Data from studies of electrical activity of the brain using intracerebral electrodes and analysis of unsuccessful surgical outcomes have shown that in some cases the reason for the persistence of seizures after removal of the SG is the presence of a larger epileptogenic zone that extends beyond the hippocampus. Brain regions anatomically and functionally associated with the hippocampus, such as the insula, orbitofrontal cortex, parietal operculum, and the junction of the parietal temporal occipital lobe, can generate seizures similar in clinical and EEG picture to temporal paroxysms. The concept of “temporal lobe epilepsy plus” (preferably temporo-peresylvian (Patrick really doesn’t like plus)) has been proposed to describe situations where hippocampal sclerosis exists along with the extratemporal seizure initiation zone. In this regard, it is important to determine the indications for invasive EEG studies in temporal lobe epilepsy caused by hippocampal sclerosis. Warning symptoms are a taste aura, an aura in the form of vertigo, and noise. Interictal epiactivity is most often localized bilaterally in the temporal regions or in the precentral region. Ictal epiactivity in temporal plus forms is more often observed in the anterior frontal, temporoparietal and precentral areas. Differential diagnosis of temporal lobe epilepsy from temporal lobe epilepsy plus, carried out by a qualified epileptologist, is key in planning surgical intervention and predicting treatment outcome.
Contraindications
Before diagnostics, you should make sure that you have no contraindications to MRI.
Magnetic resonance imaging is not performed in the following cases:
- The presence of a pacemaker or metal structures in the body (non-removable type).
- Women do not undergo MRI during the first trimester of pregnancy; diagnosis can only be carried out as prescribed by a doctor.
- Magnetic resonance imaging in a closed tomograph is not performed if you are afraid of closed spaces.
- It is not recommended to do an MRI if there are serious abnormalities in the functioning of the nervous system or psyche.
If there is a need to use a contrast agent, you should ensure that:
- An allergic reaction to the drug used.
- Kidney or liver failure.
- Pregnancy and lactation.