A pinched nerve in the shoulder joint is a common problem. Many people confuse it with the inflammatory process, although these are two different neurological diseases that have similar symptoms. At the same time, experts note that if treatment is not timely, pinching can lead to the development of an inflammatory process. To avoid such a complication, you need to pay attention to the first symptoms and seek qualified help from a specialist.
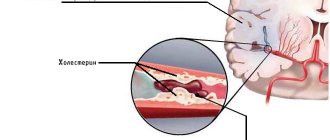
The nerve can become pinched when bone spurs begin to appear around the spinal disc. The discs act as some kind of “shock absorbers” between the vertebrae in the spinal column. Bone spurs are new bone formations. They begin to grow when the discs weaken significantly and wear out over time. As we age, the vertebrae become compressed and the discs become thinner. Bone spurs grow around the discs to strengthen them. However, this bone growth can put negative pressure on the nerve root in the spinal column.
Causes of pain in the shoulder joints
There are many reasons for the appearance of painful sensations. Pain in one or both shoulders can be a consequence of inflammation of the tendons, microtrauma of the articular cartilage, inflammatory-degenerative pathologies of the joints and cervicothoracic spine. The discomfort can be either minor or so intense that you cannot move your arm.
Among the causes that cause sharp or aching pain in the shoulder are:
- one-sided intense load for a long time;
- scoliosis, lordosis and other deviations in the normal position of the spine;
- physical inactivity.
In addition, pain can occur due to infections, inflammatory processes, hereditary predisposition, diseases of internal organs, and tumors.
In cases where the right shoulder hurts, the following pathologies may be present:
- Tendonitis is inflammation of tendons and soft tissues due to significant physical activity.
- Myositis - when the muscles of the shoulder joint are involved in the inflammatory process.
- Arthrosis is the destruction of articular cartilage.
- Arthritis is an inflammatory process in a joint due to infection, allergic reaction or autoimmune diseases.
- Osteochondrosis of the cervical spine.
- Bursitis is an inflammation of the joint capsule.
- Capsulitis is a pathological change affecting the joint capsule and synovium.
- Brachial nerve neuritis.
- Tuberculous lesion of the joint on the right.
- Humeroscapular periarthritis.
- Metastasis from a nearby tumor.
- Chondrosarcoma.
- Right-sided pneumonia.
Pain in the left shoulder joint is much less common, especially if the person is right-handed. Still, the load on the left hand is significantly less compared to the right. When your left shoulder hurts, the reasons may be the following:
- sprain;
- biceps tendinitis;
- intervertebral hernia in the cervical spine;
- calcification in the tendon;
- angina pectoris or myocardial infarction.
There are cases when the shoulder hurts when raising your arm. Here we can talk about pathologies such as:
- joint injuries;
- rheumatic lesion;
- rotator cuff tendinitis;
- tenosynovitis;
- tendobursitis and bursitis;
- myositis;
- hernia of the cervical spine.
The appearance of pain in the shoulder when trying to move the arm back indicates the presence of bursitis, radiculitis, tendinitis, spinal overload, arthrosis-arthritic joint damage, myocardial infarction.
Brachial plexus injuries
Damage to individual peripheral nerves and nerve plexuses.
In pediatric practice, lesions of the brachial plexus nerves are usually a consequence of pathological childbirth.
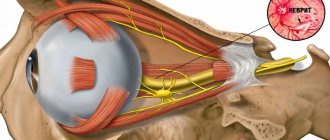
Plexus brachialis (brachial plexus)
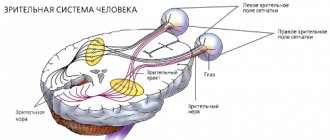
The brachial plexus is composed of fibers of the anterior branches of the 5th, 6th, 7th, 8th cervical, 1st, 2nd thoracic spinal nerves. The upper trunk (truncus superior) of the brachial plexus is formed from the C5 and C6 spinal nerves, the middle trunk (fruncus medius) is a continuation of the C7 spinal nerve, and the lower trunk (truncus inferior) is formed from the fusion of the C8 and TI-T2 spinal nerves. The listed trunks of the brachial plexus are located in the supraclavicular fossa.
Damage to the entire brachial plexus causes flaccid atrophic paralysis and anesthesia of the upper limb with loss of the extensor-elbow, flexion-elbow and carporadial reflexes. With high lesions of the plexus, damage to the scapular muscles and the Claude Bernard-Horner symptom are added.
Damage to the C5-C6 spinal nerves or the upper trunk of the brachial plexus (Duchenne-Erb palsy) leads to loss of function of the axillary (m. deltoideus), musculocutaneous (mm. biceps, brachialis) and only partially radial (mm. brachioradialis, supinator) nerves . With radicular or very high lesions of the upper trunk, loss of function and scapular muscles (mm. supraspinatus, infmspinatus, subscapularis, serratus anterior) is associated. The ulnar-flexion reflexes are extinguished and the carporadial reflexes may be weakened.
Thus, upper paralysis is characterized by damage to the proximal part of the upper limb while the function of the hand and fingers is preserved. In this case, the distribution of the anesthetic zone occurs along the radicular (C5-C6) type on the outer surface of the shoulder and forearm.
Damage to the C8-T2 spinal nerves or the primary lower trunk of the brachial plexus (Dejerine-Klumpke palsy) causes complete loss of function of the ulnar, internal cutaneous nerves of the shoulder and forearm and partial damage to the median nerve and its lower leg.
The result is distal paralysis with predominant damage and atrophy of the small muscles of the flexors of the fingers and hand, the so-called lower plexus palsy. With a high lesion before discharge rr. communicantes (sympathetic fibers going to the eye), Horner's symptom is added. Sensitivity is impaired in a radicular (C8-T2) manner on the inner surface of the hand, forearm and shoulder.
Damage to the C7 spinal nerve or middle trunk plexus causes significant loss of function of the radial nerve and partially the median nerve.
The trunks of the brachial plexus are further divided into anterior and posterior branches. The anterior bundle (fasciculus lalemlis) is formed from the anterior branches of the upper and middle trunks (C5, C6, C7). From the anterior branches of the lower trunk (C8, T2) the internal bundle (fasciculus medialis) is formed. Finally, from all the posterior branches of the primary trunks (C5, C6, C7, C8, Tl, T2) the posterior bundle (fasciculus posterior) is formed. The names of the beams are determined by their location relative to a. axillaris.
The bundles of the brachial plexus are located in the subclavian fossa; further they form the actual nerves of the upper limb: external bundle - n. musculocutaneus and the upper leg of n. mediani; posterior bundle - n. axillaris et n. radialis and internal beam - n. ulnaris, lower leg n. mediani, nn. cutanei brachii et antebrachii medialis.
Damage to the external bundle of the brachial plexus causes complete disruption of the function of n. musculocutanei, partial - n. mediani (fibers of its upper leg, in particular m. pronator teres), and limited - n. radialis (mm. brachioradialis, supinator).
Thus, the similarity of the clinical picture of a lesion of the upper trunk of the brachial plexus and a lesion of the external bundle of the brachial plexus lies in the loss of the function of the musculocutaneous nerve in both cases and the limited loss of the function of the radial nerve.
The difference is that when the upper trunk of the brachial plexus is damaged, this combination also includes loss of function n. axillaris, which does not suffer when the external bundle of the brachial plexus is damaged, but in the latter case there is partial damage to n. mediani.
Lesions of the internal bundle of the brachial plexus and lesions of the lower trunk of the brachial plexus give a similar clinical picture, i.e., a combination of lesions n. ulnaris, nn. cutanei brachii et antebrachii mediales and partial lesions i. mediani (its lower leg). Horner's symptom in this case, as with more distal lesions, is not observed.
Damage to the posterior bundle of the brachial plexus is characterized by a combination of lesions n. axillaris et n. radialis (except for preserved mm. brachioradialis, supinator). The similarity with the clinical picture of damage to the middle trunk of the brachial plexus is the same loss of function n. radialis. The difference is that when the middle trunk is damaged, the function n. axillaris is preserved, but instead the function of n. mediani, its upper leg.
Thus, the fibers of the lower trunk of the brachial plexus become part of the internal bundle, which causes the similarity of the clinical picture when they are affected. N. radialis suffers in its main function both when the middle trunk and the posterior bundle are damaged, but in the first case (middle trunk) - in combination with partial damage to n. mediani, and in the second (posterior bundle) - with lesion n. axillaris.
Function n. axillaris falls out both when the upper trunk and the posterior bundle are affected due to the corresponding transition of its fibers.
Finally, and. musculocutaneus suffers equally when the upper trunk and the external bundle are affected, but in the first case (upper trunk) - in combination with, n. axillaris, and in the second (lower fascicle) with partial damage to n.mediani.
Nerves arising from the brachial plexus.
- axillaris (axillary nerve ). The mixed nerve is composed of fibers of the C5, C6 and C7 spinal nerves, passing first as part of the upper trunk, then the posterior bundle of the plexus.
When the C5-C6 spinal nerves or the upper trunk of the brachial plexus (in the supraclavicular fossa) are damaged, as is observed with Erb's palsy, the nerve suffers in combination with n. musculocutaneus.
If the posterior bundle is damaged (in the subclavian fossa), the function n. axillaris is disrupted together with n. radialis.
The motor fibers of the nerve innervate m. deltoideus (et m. teres minor), sensitive - the skin of the outer surface of the shoulder (n. cutanei brachii lateralis).
When n. is affected. axillaris, there is atrophy of the deltoid muscle, the inability to raise the shoulder in the frontal plane to a horizontal line and impaired sensitivity on the skin of the outer surface of the shoulder.
- musculocutaneus (musculocutaneous nerve). The nerve is mixed and is also formed from fibers of the C5-C6-C7 spinal nerves, passing through first the upper trunk, then the external fascicle of the brachial plexus.
When the C5-Cb spinal nerves or the upper trunk of the plexus (in the supraclavicular fossa) are damaged, as happens with Duchenne-Erb's palsy, it suffers in combination with n. axillaris.
If the external bundle is damaged (in the subclavian fossa), loss of function n. musculocutaneus is observed in conjunction with partial damage to I. mediani, its upper leg (weakening of pronation and palmar flexion of the hand).
The motor fibers of the nerve innervate m. biceps brachii (as well as m. brachialis et m. coracobrachialis), and sensitive - the skin of the outer (radial) surface of the forearm (n. cutanei anlebrachii lateralis).
When n. is affected. musculocutanei, atrophy of m occurs. bicipitis, the flexion-elbow reflex fades and flexion of the forearm is significantly weakened (it is completely impossible in the pronation position, since in the supination position or the average between them, flexion in the elbow joint can be carried out due to the contraction of the m. brachioradialis, innervated by the n. radialis.
Sensitivity disorders are observed on the outer (radial) surface of the forearm.
- radialis (radial nerve ). The mixed nerve arises mainly from the fibers of the C7 spinal nerves (partly from C5, C6, C8 and T1), passing first as part of the middle trunk, then the posterior fascicle of the brachial plexus.
With damage to the C7 spinal nerves or the middle trunk, the main function of the nerve (except for the m.brachioradialis et m.supinator) is lost in combination with partial damage to the n.mediani, its upper leg (weakening of pronation and palmar flexion of the hand)
When the posterior bundle of the brachial plexus is damaged, the same basic functions of n. radialis, but in combination with damage to n. axillaris.
Motor fibers n. radialis innervates the extensors of the forearm (m. triceps et m. anconeus), hand (mm. extensores carpi radialis et carpi ulnares) and fingers (mm. extensores digitorum), the supinator of the forearm (m. supinator), the abductor pollicis muscle (m. abductor pollicis longus) and so on brachioradialis, which takes part in the flexion of the forearm. Sensitive fibers innervate the skin of the posterior surface of the shoulder (n. cutaneus brachii posterior), the dorsal surface of the forearm (n. cutaneus antebrachii dorsalis), the radial side of the dorsum of the hand and partially the first, second and sometimes third fingers.
With high damage n. radialis in the axillary fossa, in the upper third of the shoulder, paralysis of the extensors of the forearm, hand, main phalanges of the fingers, and the abductor pollicis muscle occurs; flexion of the forearm (m. brachioradialis) is weakened. The reflex from the m tendon fades away. triceps and the carporadial reflex is somewhat weakened (by turning off the contraction of the m. brachioradialis). Sensitivity is lost on the dorsal surface of the shoulder, forearm, and partly the hand and fingers. The zone of sensory disorders on the hand is often significantly reduced due to the overlap of the zone with the innervation of neighboring nerves. The joint-muscular feeling does not suffer. At lower levels of damage, the nerve function suffers to a limited extent, since the higher branches are preserved, which facilitates the tasks of topical diagnosis.
When the nerve is damaged, which is very common, at the level of the middle third of the shoulder, the function of extension of the forearm and the extension-ulnar reflex (m. triceps) are preserved and sensitivity in the shoulder is not impaired.
If the lower third of the shoulder is affected, the function of the m. brachioradialis and sensitivity on the dorsal surface of the forearm (n. cutaneus antebrachii dorsalis), since the corresponding branches extend from the main trunk of the nerve higher, in the middle third of the shoulder. When a nerve is damaged in the forearm, the function of n. brachioradialis et i. cutanei antebrachii dorsalis is usually preserved; loss is limited to damage to the extensors of the hand and fingers with sensory impairment only on the hand. With damage even lower, in the middle third of the forearm, loss of motor function can be even more limited; while extension of the hand is preserved, only extension of the main phalanges of the fingers may suffer.
When the radial nerve is damaged, weakness of the wrist extensors develops, and a typical falling or drooping hand occurs.
Among the numerous descriptions of samples or tests that determine movement disorders with damage to the radial nerve, the following can be noted:
- Inability to straighten the hand and fingers.
- Inability to abduct the thumb.
- When the hands are folded together with the fingers straightened, the fingers of the affected hand are not retracted, but the bent ones seem to “slide” along the palm of the healthy, abducted hand.
- ulnaris (ulnar nerve ). The nerve is mixed, made up of fibers of the C8-T1-T2 spinal nerves, passing through first the lower trunk, then the internal bundle of the brachial plexus.
With damage to the spinal nerves C8—T1—T2 of the lower trunk and the internal bundle of the brachial plexus, the function of the nerve suffers equally in combination with damage to the cutaneous internal nerves of the shoulder and forearm (nn. cutanei brachii et antebrachii mediates) and partial dysfunction of n. mediant, its lower leg (weakening of the tenor flexor muscles), which creates the clinical picture of Dejerine-Klumpke palsy.
The motor function of the nerve mainly consists of palmar flexion of the hand, flexion of fingers V, IV and partly III (mm. lumbricales, flexor digitorum profundus, interossei, flexor digiti V), adduction of the fingers, their spread (mm. interossei) and adduction of the thumb ( m. adductorpollicis); in addition, in the extension of the middle and terminal phalanges of the fingers (t. lumbricales. interossei).
With regard to the innervation of the movements of the 1st and 2nd fingers, the function of the ulnar nerve is associated with the function of the median nerve; the first has a predominant relation to the function of the 5th and 4th fingers; the median nerve to the function of the 2nd and 3rd fingers. Sensitive fibers innervate the skin of the ulnar edge of the hand, V and partially IV, and less often III fingers.
Complete damage to the ulnar nerve causes weakening of the palmar flexion of the hand (flexion is maintained partially due to the m. flexor carpi radialis et m. palmaris from the n. medianus), lack of flexion of the IV and V, and partly of the III fingers, the impossibility of bringing and spreading the fingers, especially the V and IV, inability to adduct the thumb.
Superficial sensitivity is usually impaired on the skin of the fifth and ulnar half of the fourth fingers and the corresponding ulnar surface of the hand.
The joint-muscular feeling is upset in the little finger. Pain with damage to the ulnar nerve is not uncommon, usually radiating to the little finger. Possible cyanosis, sweating disorders and a decrease in skin temperature in an area approximately coinciding with the area of sensory disorders. Atrophy of the muscles of the hand with damage to t. ulnaris appears clearly, depression of the interosseous spaces, especially the first, as well as a sharp flattening of the hypotenor are noticeable.
As a result of the defeat of mm. interossei et lumbricalis, the hand takes the form of a “clawed bird’s paw”; with hyperextension of the main phalanges, bending of the middle and terminal phalanges is observed, due to which the fingers take a claw-like position. This is especially pronounced in relation to the V and IV fingers. At the same time, the fingers are slightly separated, especially the IV and mainly V fingers.
Its first branches n. ulnaris radiates only to the forearm, so its lesion along the entire length to the elbow joint and the upper part of the forearm gives the same clinical picture.
The lesion in the region of the middle and lower thirds of the forearm leaves the innervation of mm intact. flexor carpi ulnaris et flexor digitorum profundus, due to which palmar flexion of the hand and flexion of the terminal phalanges of the V and IV fingers are not affected. But the degree of “clawedness” of the hand increases.
To determine movement disorders that occur when the ulnar nerve is damaged when the hand is clenched into a fist, the following basic tests are available:
- When the hand is clenched into a fist, fingers V and IV, and partly III, are not bent enough.
- Bending the terminal phalanx of the fifth finger or “scratching” the little finger on the table with the palm tightly fitting to it is not possible.
- It is impossible to adduct the fingers, especially V and IV.
- Thumb test: the patient stretches a strip of paper, grasping it with both hands between the bent index finger and straightened thumb; with damage to the ulnar nerve and, consequently, paralysis of the m. adductoris pollicis adduction of the thumb is impossible and the strip of paper is not held with the straightened thumb. In an effort to hold the paper, the patient bends the terminal phalanx of the thumb with the help of m. flexor pollicis, innervated by the median nerve.
- medianus (median nerve ). The mixed nerve is formed from fibers of the C5, C6, C7, C8 and T1 spinal nerves, passing mainly through the middle and lower trunks of the brachial plexus. Subsequently, the fibers of the median nerve pass in the external and internal bundles. The upper leg of the n. extending from the external bundle. mediani and from the internal bundle its lower leg merge, forming a loop of the median nerve.
When the C7 spinal nerve or the middle trunk of the brachial plexus is damaged, the function of the median nerve suffers partly as a result of weakening of wrist flexion (m. flexor carpi radialis), pronation (mm. pronalores) in combination with damage to the radial nerve.
Almost the same loss of function n. mediani occurs when the external bundle of the brachial plexus is damaged, into which the fibers of the upper peduncle of the nerve pass from the middle trunk, but in combination with damage to the musculocutaneous nerve.
With damage to the C8-T1 spinal nerves, the lower trunk and the internal bundle of the brachial plexus (Dejerine-Klumpke palsy), they suffer in combination with damage to n. ulnaris, n. cutanei brachii el anlebrachii medialis fibers n. medianus, which make up its lower leg (weakening of the flexors of the fingers and tenor muscles).
The motor function of the nerve mainly consists of pronation, palmar flexion of the hand due to contraction of m. flexor carpi radialis el m. palmaris longus flexion of fingers, mainly I, II and III (mm. lumbricales flexor digitorum sublimis el pmfundus, flexorpollicis), extension of the middle and terminal phalanges of II and III fingers.
Sensory fibers etc. mediani innervate the skin of the palmar surface of the I, II, III and radial half of the IV fingers, the corresponding part of the palm, as well as the skin of the rear of the terminal phalanges of these fingers.
When the median nerve is damaged, pronation suffers, palmar flexion of the hand is weakened (preserved only by the m. flexor carpi ulnaris from n. ulnaris), flexion of the I, II and III fingers and extension of the middle phalanges of the II and III fingers (mm. lumbricalis, inlerossei) are impaired. . Superficial sensitivity is impaired in the hand in an area free from the innervation of the ulnar and radial nerves. Articular-muscular sensation is always impaired in the terminal phalanx of the index, and often in the second finger. Muscle atrophy with damage to the median nerve is most pronounced in the tenor area. The resulting flattening of the palm and bringing the thumb close and in one plane to the index finger create a peculiar position of the hand, which is called “monkey”.
Pain when the median nerve is damaged, especially partial, is quite intense and often takes on a causal nature. In the latter case, the position of the hand may become bizarre. Vasomotor-secretory-trophic disorders are also common and characteristic of lesions of the median nerve: the skin, especially the 1st, 2nd and 3rd fingers, becomes bluish or pale in color; nails become “dull”, brittle and streaked; skin atrophy, thinning of fingers (especially II and III), sweating disorders, hyperkeratosis, hypertrichosis, ulcerations, etc. are observed. These disorders, as well as pain, are more pronounced with partial rather than complete damage to n. medianus.
Its first branches n. medianus, like n. ulnaris, radiates only to the forearm, so the clinical picture with high damage along the entire length from the axillary fossa to the upper parts of the forearm is the same.
When n. is affected. mediani in the middle third of the forearm, in which the branches extending to mm. pronator leres, flexor carpi radialis, palmaris longus flexor sublimis, the functions of pronation, palmar flexion of the hand and flexion of the middle phalanges are not affected. With lower nerve lesions, the function of flexion of the terminal phalanges of the I, II and III fingers may also be preserved.
The main tests to determine movement disorders arising from damage to the median nerve are the following:
- When squeezing the hand and fist, fingers I, II and partly III do not bend
- Bending the terminal phalanges of the thumb and index fingers is impossible, as is scratching the index finger on the table with the hand tightly fitting to it.
- During the thumb test, the patient cannot hold a strip of paper with a bent thumb and will hold it by adducting with a straightened thumb (mm. adductor policis from retained n. ulnaris).
- cutaneus brachii medialis (cutaneous internal nerve of the shoulder ). A sensory nerve, the fibers of which arise from C8, T1, partly from T2 spinal nerves and pass through first the lower trunk, then the internal bundle of the brachial plexus and innervate the skin of the inner surface of the shoulder. When it is damaged, sensory disturbances and pain in the shoulder area occur.
- cntaneus antibrachii medialis (cutaneous internal nerve of the forearm). Sensory nerve. Innervates the skin of the inner surface of the forearm. It is formed from the C8-T2 spinal nerves.
When the nerve is damaged, sensory disturbances occur, and possibly pain in the forearm area.
Isolated lesions of these nerves are rare. Their damage is often included in the clinical picture of damage to the lower trunk or internal bundles of the brachial plexus or is observed in combination with damage to other nerves of the limb.
The main challenge that must be resolved to select appropriate treatment is to determine the level of damage as accurately and early as possible.
Indications for neurosurgical operations are clinical signs of severe upper and total paralysis, Horner's syndrome, relaxation of the diaphragm, lack of restoration of motor and sensory functions of the upper limb in infants. The most optimal age of patients for neurosurgical operations is the first year of life. For operations on the brachial plexus, the transverse supraclavicular approach and its modifications, as well as the transclavicular one, are used. The methods of choice for neurosurgical operations are external and internal neurolysis, plastic surgery and suture of nerves, neurotization
A comparison of groups of children treated only conservatively and with the use of neurosurgery showed that the latter significantly improves outcomes.
Symptoms of the disease
Shoulder pain manifests itself in different ways depending on the cause. Acute is typical in case of injury. When a bruise, dislocation or sprain occurs, the patient experiences discomfort that increases when moving the upper limb. When a fracture occurs, it becomes impossible to move the arm.
Unbearable pain radiating to the neck and upper back is observed with capsulitis. In addition to pain, there is an inability to move the arm back or raise it. Severe pain also occurs with brachial neuritis and arthritis. The first is characterized by the absence of signs of inflammation in the joint; in the second case, swelling of the soft tissues and limited range of motion are noticeable.
Aching pain in the shoulder may be a sign of osteochondrosis of the cervicothoracic spine. Often the symptom is accompanied by numbness of the hand, burning and tingling sensation in the fingers. Aching pain is also observed with deforming arthrosis, but in this case, along with discomfort, a person notes stiffness of movement and swelling in the shoulder joint in the morning, crunching and clicking when bending/extending the arm. With the gradual destruction of cartilage, lifting heavy objects or active movement provokes increased pain.
Constant pain for several weeks is characteristic of bursitis, when the inflammatory process develops in the periarticular bursa. The disease is accompanied by the formation of a compaction, upon pressing on which a fluid transfusion is felt.
Causes
These nerves can be damaged by stretching, pressure, or cutting. A strain can occur when the head and neck are forced away from the shoulder, such as during a fall from a motorcycle or sometimes a car accident. In more severe cases, the nerves may become torn from the spinal cord. Pressure can occur when the brachial plexus between the collarbone and the first rib is damaged, which can occur during a fracture or dislocation. Swelling in the area from excessive bleeding or damaged soft tissue can also lead to injury.
Diagnosis of pathology
Naturally, when there is discomfort, the question inevitably arises: what to do if your shoulder hurts? Don't wait for the symptoms to go away on their own. It is imperative to consult a doctor, whose specialization will depend on the cause of the disease and the general condition of the patient.
If the pain appears after a fall or bruise, then contact a traumatologist. Osteochondrosis and neuritis are treated by a neurologist, a surgeon and a rheumatologist eliminate the consequences of arthrosis, arthritis and tendonitis.
When painful sensations are accompanied by a general deterioration in well-being, it is recommended to consult a therapist, oncologist, cardiologist or gastroenterologist. Indeed, sometimes pain is reflected when there is a discrepancy between the localization of discomfort and the location of damaged organs or tissues. It is very important to diagnose in time, because shoulder pain can appear due to myocardial infarction, pneumonia, pleurisy, pancreatitis, cholecystitis, and neoplasms in the chest.
For diagnostic purposes, the doctor may prescribe the following types of examinations:
- X-ray of the shoulder or entire upper limb;
- Ultrasound of the shoulder joint;
- MRI of the joint and/or spine;
- ECG.
In addition, you may need to take a general blood test, as well as biochemistry and sexually transmitted infections. The patient is also prescribed fluorography and fibrogastroduodenoscopy.
Treatment for pain in the shoulder joint
When complaining of pain in the shoulder, the specialist prescribes comprehensive treatment. Therapy includes:
- Local and general anesthesia. Can be achieved using medications or physiotherapeutic methods, acupuncture, etc.
- Eliminating the root cause of pain. Manual therapy, osteopathy, PRP therapy and Kinesitherapy help with this.
- Symptomatic therapy. They use products to relieve swelling of soft tissues, hyperemia of the skin, and reduce temperature.
- Rehabilitation treatment. This includes kinesitherapy.
During the rehabilitation period, physical therapy and physiotherapeutic treatment are widely used to restore joint mobility. In advanced cases and in the absence of effect from conservative therapy, surgical treatment is possible.
The article was reviewed by traumatologist-orthopedist V.Yu. Bogdanov.
Treatment
In most cases, treatment takes place on an outpatient basis, in severe situations - in a hospital. For plexopathy, anti-inflammatory therapy is carried out, painkillers, dehydrating drugs are used, and physiotherapeutic procedures are also prescribed. After the pain subsides, special exercises, massage, and a complex of vitamins are prescribed.
In more severe situations, surgical treatment is prescribed to eliminate the compression and restore the functionality of the plexus branches.
Cost of treating shoulder pain in our Center
| Services list | Price |
| Initial consultation with a kinesiotherapist | 1600 |
| Interim consultation with a kinesiotherapist | for free |
| Session with a kinesiotherapist (1 patient) | 3900 |
| Individual lessons with a personal trainer | 2700 |
| Subscription for 1 month of training in the gym on simulators | 10 000 |
| Subscription for 6 months of gym training | 45 000 |
| Physiotherapist consultations | 1600 |
| Physiotherapist consultations during the cycle | for free |
| UVT 1 procedure | 2000 |
| HIVAMAT up to 15 min./1 body unit | 2200 |
| HIVAMAT up to 15 min./2 body units | 3200 |
| Appointment with an orthopedist-traumatologist | 1600 |
| Intra-Articular PRP Injection | 6500 |
| Massage of one upper limb (15 min.) | 2200 |
| Massage of two upper limbs (30 min.) | 3000 |
| Kinesio taping | 1100 |
| Complex taping (joints) 1 zone | 1600 |
| Complex taping (joints) 2 zones | 2200 |
Contact us
Call now
8 (495) 803-27-45
Make an appointment through our service
Make an appointment
Treatment process at the Innovation Center
Our Innovative Clinic has created excellent conditions for the diagnosis and treatment of pain in the shoulder joints of various types and origins. After finding out the causes of the pathology, the doctor will select tactics and methods of treatment. We practice using the following techniques:
- Acupuncture.
- Manual therapy.
- Kinesitherapy.
- Osteopathy.
- Massotherapy.
- Physiotherapy.
We achieve excellent results using shock wave therapy and Hiwamat therapy. The course of treatment is carried out under the supervision of a doctor, whose efforts are aimed not only at relieving unpleasant symptoms, but also at eliminating the cause of discomfort. The professionalism of our specialists and an individual approach will help you completely get rid of the problem, and if this is not possible, then avoid complications and achieve stable remission. This is confirmed by a large number of reviews about the work of our center and doctors both on our website in the Reviews section and on other sites on the Internet.