Causes of the disease
Most often, optic neuritis develops with multiple sclerosis and is its first manifestation. The basis of the inflammatory process in this case is demyelination, or destruction of the myelin sheath of the nerve. Damage to the optic nerve is also provoked by other autoimmune pathologies: systemic lupus erythematosus, Sjogren's syndrome.
Diseases associated with serum immunoglobulin G to myelin-oligodendrocyte glycoprotein (MOG-IgG), in particular acute disseminated encephalomyelitis, also lead to demyelination and, as a consequence, optic neuritis.
Axons and neurons of the optic nerve are destroyed not only as a result of demyelinating processes, but also against the background of other diseases. These include:
- inflammation of the eyeball and/or orbit;
- inflammatory diseases of the brain;
- infectious processes in the nasopharynx;
- sarcoidosis, granulomatosis;
- acute cerebrovascular accident;
- endocrine pathologies – thyrotoxicosis, diabetes mellitus;
- specific infections - tuberculosis, syphilis, influenza.
Optic neuritis can be a consequence of eye injury, traumatic brain injury, toxic damage - in most cases it is poisoning with methyl alcohol, lead, and sometimes helminthic infestations. May be provoked by complicated pregnancy.
Factors causing retrobulbar neuritis
Various problems provoke the development of abnormal vision impairment. Inflammation itself begins as a result of damage to the body by infectious diseases, chronic diseases caused by immunodeficiency. Etiological reasons include:
- Chronic stages of viral infections - the main causative agent is cytomegalovirus, which provokes the development of mononucleosis. The stable location of harmful agents causes deformations in immune properties. Due to the production of antibodies for one's own tissues, the process of autoimmune inflammation begins.
- Chronic infectious points - most often the anomaly is caused by unfavorable foci that are located nearby (for example, sinusitis, otitis media and others), much less often - by distant places (cystitis). The infection enters the nervous structure of the visual apparatus through blood transportation.
- Inflammatory phenomena in the orbit - provocateurs are inflammatory processes. Spread occurs in two ways: hematogenous and perineural, which causes damage to the retrobulbar perimeter of the nerve. Quite often, total optic neuritis is diagnosed.
Secondary progression of optic nerve disorder begins as a result of an anomaly that is localized in the cerebral region. The main etiofactors include the following diseases:
- Multiple sclerosis - selective damage to the myelin sheath of nerve fibers moves to the optical areas, which causes an inflammatory reaction. Neuritis of a retrobulbar nature is considered the initial stage in more than 65% of cases of disease.
- Brain tumors - when voluminous tumors form in the area of the chiasm glioma, objects in another place begin to actively pressure the optic chiasm, disrupting the process of blood circulation in the body and metabolism in tissues. As a result, the patient develops symptoms of neuritis.
- Neuroinfections - Lyme disease, neuroAIDS, tuberculous meningitis can provoke abnormalities in the retrobulbar zone. Inflammatory phenomena are associated with the entry of infectious microorganisms into the body. In some cases, the disease may appear due to intoxication. Exogenous lesions are caused by the influence of toxic chemicals, methyl alcohol, iodine substances. Toxins appear as a result of dysmetabolic processes, renal failure or during pregnancy.
Symptoms of optic neuritis
Symptoms vary depending on the type of disease: intrabulbar (papillitis) or retrobulbar neuritis.
Papillitis (intraocular, retrobulbar neuritis)
It is characterized by an acute onset with a rapid deterioration in visual acuity - from 1-2 hours to 1-2 days. In some cases, mild headache and pain when moving the eyes occur. With partial damage, visual acuity may be preserved, but scotomas appear - areas of partial or complete loss of the visual field, which can be central or paracentral, round or arch-like. There may be a narrowing of the boundaries of the visual field, a decrease in dark adaptation and color perception. Most often, symptoms of visual impairment disappear after 7-10 days; after 2-3 weeks (sometimes up to 5 weeks), vision is restored. Without treatment or with severe neuritis, optic nerve atrophy with complete loss of vision is possible.
Retrobulbar neuritis
It occurs in acute or chronic form. The acute form is more often characteristic of unilateral lesions, the chronic form - for bilateral ones.
General symptoms:
- pain when moving the eyeballs and pressing on the eye;
- color vision disorders - decreased sensitivity of the eye to colors, shades quickly fade;
- a drop in visual acuity to the point of complete inability to distinguish objects;
- appearance of scotomas.
Depending on the form of retrobulbar neuritis, symptoms may vary. Axial neuritis is characterized by a combination of central scotoma with partial loss of visual fields and the appearance of peripheral defects in the visual field. In the peripheral form, the field of vision narrows along the entire perimeter - it is concentric in nature. The transversal form is characterized by a significant decrease in vision, up to blindness, scotomas merging with peripheral loss of visual fields.
What is retrobulbar neuritis?
Retrobulbar neuritis is an inflammatory disease that affects the optic nerve, located between the orbit and the visual area. If there is an anomaly, the patient experiences a decrease in the level of visual acuity, the occurrence of prolapses, minimization of boundaries, and painful sensations during motor reflexes with the eyeballs. As research methods, doctors use complex neurological and ophthalmological techniques. Therapeutic therapy is performed using antibacterial/antiviral medications, glucocorticosteroids, diuretics and neuroprotective drugs. In some cases, detoxification procedures and physical therapy are prescribed.
Classification and stages of disease development
Depending on the affected area:
- Intrabulbar (intraocular) neuritis, optic papillitis. This is an inflammation of the intraocular part (disc) of the optic nerve. More often develops in children.
- Retrobulbar neuritis. Damage to the nerve section lying between the eyeball and the optic chiasm. Forms of retrobulbar neuritisSource: Retrobulbar optic neuritis. Kukhtik S.Yu., Popova M.Yu., Tantsurova K.S. Bulletin of the Council of Young Scientists and Specialists of the Chelyabinsk Region, 2021: axial - a bundle of axons passing in the optic nerve is involved in the pathological process;
- peripheral - inflammation covers the nerve sheaths and spreads deep into the nerve trunk with the formation of a large amount of exudate under the sheaths;
- transversal - the process affects all layers of the optic nerve.
According to the etiology of the lesion:
- infectious:
- parainfectious (post-vaccination, after acute respiratory viral infections);
- demyelinating;
- ischemic;
- toxic;
- autoimmune.
According to the severity of the flow:
- spicy;
- chronic.
According to the prevalence of the lesion:
- mononeuritis – inflammation of one nerve (the vast majority of cases);
- polyneuritis – involvement of both optic nerves in the process (less than 1% of cases).
Description
Diseases of the optic nerve are divided into three main groups:
• inflammatory (neuritis); • vascular (optic nerve ischemia); • degenerative (atrophy);
There are descending (retrobulbar) neuritis, when the inflammatory process is localized on any part of the optic nerve from the chiasm to the eyeball, and ascending neuritis (papillitis), in which the intraocular and then the intraorbital part of the optic nerve is involved in the inflammatory process.
When the optic nerve is damaged, functional disorders always occur in the form of decreased central vision, narrowing of the visual field, and the formation of absolute or relative scotomas. Changes in the visual field to white and other colors are one of the early symptoms of optic nerve damage.
With severe damage to the fibers of the optic nerve, amaurotic immobility of the pupil is noted. The pupil of the blind eye is slightly wider than the pupil of the other seeing eye.
In this case, there is no direct and the indirect (friendly) reaction of the pupil to light remains. On the seeing eye, a direct, but no friendly reaction of the pupil to light is preserved. The reaction of the pupils to convergence is preserved.
According to the nature of the lesion and clinical manifestations, diseases of the optic nerve are divided into inflammatory (neuritis), vascular (optic nerve ischemia), specific (tuberculosis, syphilitic), toxic (dystrophic), tumor, associated with damage to the optic nerve, abnormalities of the optic nerve, lesions, associated with impaired circulation of cerebrospinal fluid in the optic nerve sheath (congestive disc), optic nerve atrophy.
To study the morphological and functional state of the optic nerves, clinical, electrophysiological and radiological research methods are used. Clinical methods include the study of visual acuity and field (perimetry, campimetry), contrast sensitivity, critical flicker fusion frequency, color perception, ophthalmoscopy (direct and reverse), ophthalmochromoscopy, as well as fluorescein angiography of the fundus, ultrasound examination of the eye and orbit, Dopplerography vessels of the internal carotid artery (ophthalmic and supratrochlear arteries).
Electrophysiological methods include the study of electrical sensitivity and lability of the optic nerve (ESiL) and recording of visual evoked potentials (VEP).
Radiological methods for studying the optic nerve include survey radiography of the skull and orbit (front and profile images), examination of the bony canal of the optic nerve, computed tomography and magnetic resonance imaging.
In case of optic nerve disease, comprehensive studies are required with consultation of a therapist, neurologist, otolaryngologist and other specialists.
INFLAMMATORY DISEASES OF THE OPTIC NERVE
There are more than two hundred different reasons that cause the clinical manifestations of optic neuritis. In the clinic, a rather conventional division of neuritis into two groups is accepted: intraocular intrabulbar (papillitis) and retrobulbar. Papillitis is characterized by a sharp disruption of the function of the papillary system of the blood-ophthalmic barrier. With an intrabulbar process (papillitis), the dynamics of the clinical picture are well determined ophthalmoscopically. With retrobulbar neuritis, the main thing in diagnosis is the symptoms of visual disturbances and their careful identification, and the ophthalmoscopic picture of the fundus can remain normal for quite a long time.
The main form of retrobulbar neuritis is axial (axial) neuritis, which affects the papillo-macular bundle. The leading symptom of axial neuritis is central scotoma, which manifests itself as a relative or absolute scotoma in white or only in red and green.
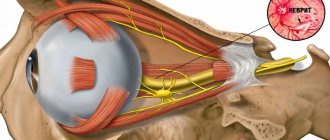
The optic disc is a small part of a closed system, which is the eyeball, in particular the eye cavity. The optic disc is the only part where it is possible to visually observe the condition of the anterior end of the optic nerve. Therefore, it is customary to divide inflammation of the optic nerve into:
- intrabulbar (papillitis);
- retrobulbar;
Retrobulbar inflammatory diseases of the optic nerve include ophthalmoscopically invisible processes in the initial stage of development.
Based on topographic location, they are distinguished:
- orbital;
- intracanalicular;
- intracranial lesions;
With papillitis, as a rule, a decrease in visual function is combined with ophthalmoscopically visible changes in the optic nerve head. With retrobulbar lesions of the optic nerve, it most often remains normal at the onset of the disease, but visual acuity and visual field suffer. And only subsequently, after a certain period of time, depending on the location of the damage to the optic nerve and the intensity of the damage, pathological manifestations appear on the disc. These manifestations are defined as characteristic signs visible ophthalmoscopically - inflammatory changes in the disc or only in the form of descending atrophy of its fibers.
The main signs of optic neuritis consist of the appearance of inflammatory exudate, edema, compression of nerve fibers by edema and the toxic effect of exudate on them. This is accompanied by small cell lymphoid infiltration and proliferation of neuroglia. In this case, the myelin sheaths and axial cylinders of the optic fibers undergo dystrophy, degeneration and subsequent atrophy. Human optic nerve fibers do not have any regenerative ability. After degeneration of the nerve fiber (axon), its mother retinal ganglion cell dies. When a diagnosis of optic neuritis is made, it is necessary to urgently use medications aimed at suppressing the inflammatory process in the area of damage to the optic nerve, reducing tissue edema and capillary permeability, limiting exudation, proliferation and destruction.
Treatment of patients with optic neuritis should be emergency in a hospital setting and directed against the underlying disease that caused the neuritis. In recent years, two stages have emerged in the tactics of treating neuritis: the first stage is immediate provision of assistance until the etiology of the process is clarified; the second stage is carrying out etiological treatment after identifying the cause of the disease.
Intrabulbar ascending neuritis (papillitis) of the optic nerve
The cause is brucellosis, syphilis, etc.), focal infections (tonsillitis, sinusitis, otitis, etc.), inflammatory processes in the inner membranes of the eye and orbit, general infectious diseases (blood diseases, gout, nephritis, etc.). With ascending neuritis, the intrabulbar part of the optic nerve (disc) is initially affected. Subsequently, as the inflammatory process spreads, the retrobulbar part of the optic nerve is affected.
The clinical picture depends on the severity of the inflammatory process. With mild inflammation, the optic disc is moderately hyperemic, its boundaries are unclear, the arteries and veins are somewhat dilated. A more pronounced inflammatory process is accompanied by a sharp hyperemia of the disc, its borders merge with the surrounding retina. Exudative foci appear in the peripapillary zone of the retina and multiple small hemorrhages, arteries and veins dilate moderately. Usually the disc does not proliferate with neuritis. The exception is cases of neuritis with edema.
The main distinguishing feature of optic nerve papillitis from a congestive disc is the lack of protrusion of the disc above the level of the surrounding retina. The appearance of even single small hemorrhages or exudative lesions in the tissue of the disc or surrounding retina is a sign of optic nerve papillitis.
Papillitis is characterized by early impairment of visual functions - decreased visual acuity and changes in the visual field.
Decreased visual acuity depends on the degree of inflammatory changes in the papillomacular bundle. Usually there is a narrowing of the boundaries of the visual field, which may be concentric or more significant in one of the areas. Central and paracentral scotomas appear. Narrowing of the peripheral boundaries of the visual field is often combined with scotomas. A sharp narrowing of the field of vision to red and impaired color perception are also characteristic. There is a decrease in electrical sensitivity and lability of the optic nerve. Dark adaptation is disrupted. When neuritis passes into the atrophy stage, the disc turns pale, the arteries narrow, exudate and hemorrhages resolve.
Treatment should be timely (early) in a hospital setting. Once the cause is identified, the underlying disease is treated. In cases of unclear etiology, broad-spectrum antibiotic therapy is indicated. Use ampiox 0.5 g 4 times a day for 5-7 days, ampicillin sodium salt 0.5 g 4 times a day for 5-7 days, cephaloridine (zeporin) 0.5 g 4 times a day for 5-7 days, gentamicin, netromycin. Fluoroquinolone drugs are also used - maxaquin, tarivid. Be sure to use vitamins: thiamine (B) and nicotinic acid (PP). A 2.5% solution of thiamine is administered intramuscularly, 1 ml daily, for a course of 20-30 injections, a 1% solution of nicotinic acid, 1 ml daily for 10-15 days. Vitamin B2 (riboflavin) is given orally, 0.005 g 2 times a day, ascorbic acid (vitamin C) 0.05 g 3 times a day (after meals). Dehydration therapy is indicated: 25% magnesium sulfate solution 10 ml is administered intramuscularly, 10% calcium chloride solution 10 ml is administered intravenously, diacarb 0.25 g is administered orally 2-3 times a day, after 3 days of administration, a break of 2 days is taken; indomethacin 0.025 g. Corticosteroids are used to reduce inflammation. Dexamethasone is given orally at 0.5 mg (0.0005 g), 4-6 tablets per day. After improvement of the condition, the dose is gradually reduced, leaving a maintenance dose of 0.5-1 mg (0.0005-0.001 g) per day for 2 doses after meals. A 0.4% solution of dexamethasone (dexazone) is administered retrobulbarically, 1 ml per day, for a course of 10-15 injections.
Retrobulbar descending optic neuritis
Significant difficulties arise in determining the etiology of retrobulbar neuritis. About half of them end up with an unknown cause. Retrobulbar neuritis often occurs with multiple sclerosis, neuromyelitis optica, and diseases of the paranasal sinuses. The most common causes of neuritis are basal leptomeningitis, multiple sclerosis, diseases of the paranasal sinuses, viral (influenza) infection, etc. Sometimes retrobulbar neuritis is the earliest sign of multiple sclerosis. The group of retrobulbar neuritis includes all descending neuritis (regardless of the condition of the optic nerve head). Compared to inflammation of the optic nerve head (papillitis), inflammation of the optic nerve trunk is observed much more often and manifests itself in the form of interstitial neuritis.
With retrobulbar neuritis, inflammation is localized in the optic nerve from the eyeball to the chiasm.
Cases of primary inflammation of the optic nerve in its orbital part are relatively rare.
Retrobulbar neuritis most often develops in one eye. The second eye gets sick some time after the first. Simultaneous disease of both eyes is rare. There are acute and chronic retrobulbar neuritis. Acute neuritis is characterized by pain behind the eyeballs, photophobia and a sharp decrease in visual acuity.
In a chronic course, the process increases slowly, visual acuity decreases gradually. Based on the state of visual functions (visual acuity and visual field), all descending neurites are divided into axial neurites (lesions of the papillomacular bundle), perineuritis and total neuritis.
With ophthalmoscopy at the onset of retrobulbar neuritis, the fundus may be normal. The optic disc is normal or more often hyperemic, its boundaries are unclear. Retrobulbar neuritis is characterized by a decrease in visual acuity and the detection of a central absolute scotoma in the field of view of white and colored objects. At the beginning of the disease, the scotoma is large in size; later, if visual acuity increases, the scotoma decreases, becomes relative, and disappears if the course of the disease is favorable. In some cases, the central scotoma turns into a paracentral annular scotoma. The contrast sensitivity of the organ of vision decreases. The disease can lead to descending atrophy of the optic nerve head. The blanching of the optic disc can vary in extent and intensity; blanching of its temporal half is more common (due to damage to the papillomacular bundle). Less commonly, with a diffuse atrophic process, uniform blanching of the entire disc is observed.
Treatment of retrobulbar neuritis depends on the etiology of the inflammatory process and is carried out according to the same principles as the treatment of patients with papillitis. The prognosis for retrobulbar neuritis is always serious and depends mainly on the etiology of the process and the form of the disease. With an acute process and timely rational treatment, the prognosis is often favorable. In chronic cases, the prognosis is worse.
VASCULAR DISEASES OF THE OPTIC NERVE
Acute obstruction of the arteries supplying the optic nerve
Vascular pathology of the optic nerve is one of the most difficult problems in ophthalmology due to the extreme complexity of the structural and functional structure and arteriovenous circulation in various parts of the optic nerve. There are two main forms of vascular lesions of the optic nerve: arterial and venous. Each of these forms can occur as an acute or chronic disease. Vascular diseases of the optic nerve belong to polyetiological disease processes.
The etiology of ischemia is thrombosis, embolism, stenosis and obliteration of blood vessels, prolonged spasms, disturbances in the rheological properties of blood, diabetes mellitus. These are mainly elderly patients with general vascular diseases, severe atherosclerosis and hypertension.
Pathogenesis: Pathogenesis is based on disturbances (reduction) of blood flow in the vessels supplying the optic nerve. Ischemic optic neuropathy is a deficiency of blood supply to nerve tissue, a decrease in the number of functioning capillaries, their closure, disruption of tissue metabolism, an increase in hypoxia and the appearance of under-oxidized metabolic products (lactic acid, pyruvate, etc.).
A. ANTERIOR ISCHEMIC NEUROPATHY OF THE OPTIC NERVE
In the pathogenesis of anterior ischemic optic neuropathy, the main factors are stenosis or occlusion of the arterial vessels supplying the optic nerve, and the resulting imbalance between the perfusion pressure in these vessels and the level of intraocular pressure. The main role is played by circulatory disorders in the system of the posterior short ciliary arteries. There is a rapid (within 1-2 days) decrease in vision down to light perception. Central scotomas appear in the field of view, more often the lower half of the field of vision falls out, less often sector-shaped loss are observed in the field of view. These changes occur more often in elderly patients due to spasm or are organic in nature (atherosclerosis, hypertension, endarteritis, etc.).
At the very beginning of the disease, the fundus of the eye may be unchanged, then on the 2nd day, ischemic edema of the optic disc and cotton wool-like edema of the retina around it appear. The arteries are narrowed, in places in the edematous retina (in the area of the disk or around it) they are not identified. The macula area is unchanged. Subsequently, the swelling of the optic disc decreases, and the disc becomes paler. By the end of the 2-3rd week of the disease, atrophy of the optic nerve of varying severity occurs. Due to the rapid deterioration of visual acuity, early treatment is necessary.
The diagnosis of anterior ischemic neuropathy is facilitated by Doppler ultrasound detection (in approximately 40% of cases) of stenotic lesions of the carotid arteries; using laser Doppler ultrasound, it is possible to determine capillary circulation disorders in the optic nerve head.
Treatment: Urgent hospitalization. Immediately after diagnosis, vasodilators, thrombolytic drugs and anticoagulants are prescribed. Give a nitroglycerin tablet (0.0005 g). Intravenous injection of 5-10 ml of 2.4% solution of aminophylline along with 10-20 ml of 40% glucose solution daily, 2-4 ml of 2% solution of no-shpa (slowly!), 15% solution of xanthinol nicotinate (complamin) - 2 ml 1-2 times a day (injected very slowly, the patient is in a lying position). Retrobulbar administration of 0.3-0.5 ml of 0.4% dexazone solution, 700-1000 units of heparin, 0.3-0.5 ml of 1% emoxypine solution is indicated.
During the development of papilledema, patients must be prescribed thiazide 0.05 g once a day before meals for 5-7 days followed by a break of 3-4 days, furosemide 0.04 g once a day, brinaldix 0 .02 g once a day, 50% glycerol solution at the rate of 1-1.5 g/kg, ethacrynic acid 0.05 g. Treatment is continued for 1.5-2 months. Patients should be consulted by a therapist and a neurologist
B. POSTERIOR ISCHEMIC NEUROPATHY OF THE OPTIC NERVE
Posterior ischemic optic neuropathy occurs mainly in older people and occurs against the background of general (systemic) diseases, such as hypertension, atherosclerosis, diabetes mellitus, collagenosis, etc. As with anterior ischemic neuropathy, the main factor in the development of this disease is the narrowing , stenosis, spasm or occlusion of the arterial vessels supplying the posterior parts of the optic nerve. Doppler ultrasound in such patients often reveals stenosis of the internal and common carotid arteries.
The disease begins acutely. Patients complain of a sharp decrease in visual acuity. Various defects are detected in the field of view: sectoral loss mainly in the inferior nasal region, concentric narrowing of the fields. Ophthalmoscopic examination during this period does not reveal any changes in the optic nerve head.
The diagnosis of the disease is helped by electrophysiological studies that reveal a decrease in electrical sensitivity and lability of the optic nerve and an increase in the travel time of the nerve impulse along the visual pathway.
Doppler studies of the carotid, ophthalmic and supratrochlear arteries often reveal changes in blood flow parameters in these vessels. After 4-6 weeks, blanching of the optic disc begins to appear in the sector that corresponds to the missing area in the field of view. Then simple descending atrophy of the optic nerve gradually develops. Excavation of the optic nerve head is not detected in this pathology.
This pathology presents great difficulties for early diagnosis. It is much less common than anterior ischemic neuropathy. In this case, the venous circulation in the optic nerve is disrupted to one degree or another. This process is in the vast majority of cases one-sided.
Treatment is similar to that for anterior ischemic neuropathy. Despite the treatment, visual acuity often remains low, and persistent defects are determined in the field of vision of patients - absolute scotomas.
Diagnosis of the disease
As a rule, patients who have the first symptoms of optic neuritis turn to an ophthalmologist. The disease is considered an interdisciplinary pathology; an ophthalmologist or neurologist must take part in its treatment. If neuritis develops against the background of other pathologies, it is necessary to clarify the diagnosis and carry out specific therapy for the primary diseases. Source: Visualization of the optic nerve in the diagnosis and monitoring of retrobulbar neuritis. Yuryeva T.N., Burlakova E.V., Khudonogov A.A., Ayueva E.K., Sukharchuk O.V. Acta Biomedica Scientifica, 2011. p. 133-136. Then the appropriate specialists are involved in the treatment - an immunologist, an otolaryngologist, an infectious disease specialist, a phthisiatrician.
The first step in diagnosing optic neuritis is collecting anamnesis, external examination of the patient, and palpation. During the medical history, the doctor will clarify the presence of concomitant pathologies, the time of onset of the disease, what complaints the patient has (pain, decreased visual acuity, changes in color perception, the appearance of “blind” spots), how quickly the symptoms developed and how severe they are, whether one eye or both is affected.
External examination and palpation may often not provide additional data. Pain, forward displacement of the eyeball, and limitation of its movements may occur with retrobulbar neuritis, but are not obligatory.
Next, the doctor proceeds to an ophthalmological examination. It includes:
- determination of visual acuity;
- the study of color perception is carried out using Rabkin’s polychromatic tables;
- study of pupil reaction to light;
- measurement of intraocular pressure, which can be a symptom of glaucoma and other diseases that provoke the development of neuritis;
- biomicroscopy – examination of the anterior segment of the eye to exclude its pathology;
- ophthalmoscopy (examination of the fundus of the eye) after instillation of drops that dilate the pupil;
- computer examination of visual fields at 120 points;
- study of visual fields using kinetic perimetry.
To clarify the diagnosis, the following methods are used:
- electrophysiological diagnostics - study of the threshold of electrical sensitivity of the retina and visual evoked potentials;
- ultrasound examination of the eyes, MRI of the orbit of the eye and brain;
- coherence tomography of the optic nerve;
- fluorescein angiography of the retina.
Laboratory diagnostics:
- general blood analysis;
- blood for HIV, syphilis, rheumatoid factor;
- blood culture for sterility;
- PCR studies;
- histological, immunochemical analysis.
If the patient has concomitant diseases, he is prescribed consultations with specialists.
Mechanism of occurrence
When examining the visual department, one can understand that the nerve contains a large number of fibers (more than a million), which begin their journey from the retina and end in the subcortical ganglia of the eye. Various forms of pathogens can cause serious disorders, for example: ischemia, inflammation and tissue destruction. As a result, the patient experiences detrimental changes that affect the functions of transmitting information from the retinal receptors that receive the external image.
The clinical picture appears as a decrease in the level of vision, impaired color perception, and loss of boundaries. If you ignore the doctor’s recommendations or completely refuse treatment, the patient begins to experience irreversible abnormalities that fill the cavities with connective tissue growths. The last stage of the disease leads to complete loss of visual abilities.
Treatment of optic neuritis
Treatment must be carried out in a hospital setting; it should begin as early as possible, in order to avoid the disease becoming chronic and developing complications. Source: Modern view on the problem of optic neuritis (systematic review). Krivosheeva M.S., Ioileva E.E. Saratov Scientific and Medical Journal, 2021. p. 602-605. For patients with optic neuritis, diet No. 15 is indicated - a general table, in the absence of indications for other types of therapeutic diets.
The basis of treatment is etiotropic therapy aimed at eliminating the primary disease that caused optic neuritis. Until the etiology of the disease is clarified, remedies are used to reduce the symptoms of inflammation, remove swelling, allergic manifestations, and improve metabolism. For this purpose:
- glucocorticosteroid drugs, if they are intolerant - non-steroidal anti-inflammatory drugs (prescribed in rare cases);
- antibacterial or antiviral therapy;
- antifungal agents to prevent fungal infection due to a long course of antibiotics;
- detoxification therapy – intravenous drip administration of saline solutions;
- antihistamines;
- diuretics;
- products that improve microcirculation;
- neuroprotectors;
- vitamins.
In addition to medications, physical therapy may be used to treat optic neuritis.
With papillitis, as well as the infectious-toxic etiology of the disease, the prognosis is more favorable than with other types of optic neuritis - in 75-90% of cases, with proper treatment, vision is completely restored. When the optic nerve is damaged due to autoimmune, demyelinating diseases, collagenosis, sarcoidosis, and specific infections, relapses often occur, incomplete restoration of vision, and nerve atrophy is possible. Source: Results of treatment of optic neuritis. Latypova E.A. Saratov Scientific and Medical Journal, 2021. p. 875-879.
Types of neuritis
There are different types of symptoms, which depend solely on the location of the lesion (central or peripheral lobe). In neurology, retrobulbar neuritis is divided into three classes:
- Axial - a common form of inflammatory reaction, localized only in the axial fascicle, characterized by a sharp decrease in central visual acuity and the appearance of scotomas.
- Peripheral - originates in peripheral structures, accompanied by the formation of intrathecal fluid, which provokes pain. A narrowing of the optical fields is characteristic.
- Transversal - a detrimental anomaly progresses in the periphery or axial region and then reaches the diameter of the nerve center. The patient is completely blind.
Another area of division of retrobulbar neuritis depends on the variability of the course:
- Acute form - manifests itself in the rapid loss of visual acuity. Most often it is diagnosed in the primary version of the lesion, which is typical for young people.
- Chronic form - symptoms have a gradual scale of increase, which are caused by a cerebral disorder. Patients experience some periods of remission or exacerbation. There is a possibility of the acute form becoming chronic.
Disease prevention
To prevent optic neuritis, it is recommended to give up bad habits, promptly treat infectious diseases, avoid eye and head injuries, and visit specialized doctors in the presence of chronic pathologies.
Article sources:
- Retrobulbar optic neuritis. Kukhtik S.Yu., Popova M.Yu., Tantsurova K.S. Bulletin of the Council of Young Scientists and Specialists of the Chelyabinsk Region, 2016
- Visualization of the optic nerve in the diagnosis and monitoring of retrobulbar neuritis. Yuryeva T.N., Burlakova E.V., Khudonogov A.A., Ayueva E.K., Sukharchuk O.V. Acta Biomedica Scientifica, 2011. p. 133-136
- Modern view on the problem of optic neuritis (systematic review). Krivosheeva M.S., Ioileva E.E. Saratov Scientific and Medical Journal, 2021. p. 602-605
- Results of treatment of optic neuritis. Latypova E.A. Saratov Scientific and Medical Journal, 2021. p. 875-879
Examination methods
The main goal of the diagnostic procedure is to make a correct conclusion with a clear identification of the etiology and the mandatory exclusion of the presence of multiple sclerosis in the patient. The study will require clarification of all symptoms, the rate of their development and previously experienced diseases, as well as full ophthalmological and neurological testing. Diagnostics:
- Visometric analysis helps determine vision loss; emerging problems can be corrected by wearing lenses.
- Color vision test - designed to accurately identify anomalies in the absence of changes in the optic disc.
- Perimetric scanning - scan the central, paracentral and peripheral sections.
- Ophthalmoscopy - looks for swelling, bleeding and the possibility of atrophy.
Multiple sclerosis: what is this disease?
Multiple sclerosis (MS) is an autoimmune chronic pathology accompanied by damage to the upper layer of nerve fibers in the brain (brain and spinal cord).
Human nerves are covered by the so-called myelin sheath, whose task is to protect thin fibers from negative influences. When the structure of this surface layer is destroyed, plaques—defective areas—are formed. As a result, the signal transmitted from the brain centers to the organs reaches poorly or does not reach at all, which leads to disruption of many body functions, including visual.
The concept of “autoimmune pathology,” which is often used to describe multiple sclerosis, means that abnormalities in the functioning of the body’s own immune system lead to the development of the pathological process. Simply put, the immune system mistakes its own cells for foreign ones and begins to destroy them. Some cells are replaced by others, resulting in the formation of scar connective tissue in place of the nerve fibers.
Many people mistakenly associate the term “multiple sclerosis” with memory problems in older people. In fact, the disease we are talking about involves a different type of disorder and often develops at a young age. Most often, the disease is detected in patients in the age range of 15-40 years, although there are cases where multiple sclerosis was found in two-year-old children.
Statistics show that the incidence rate of multiple sclerosis is approximately 25 cases for every 100 thousand people. And this is the second most common cause that leads to neurological disability at a young or young age.
Clinical picture of toxic neuritis
The clinical picture of retrobulbar neuritis, which is caused by intoxication, has some of its own characteristics. The most common cause is poisoning with methyl alcohol and mixtures containing it.
In mild poisoning, only nausea and vomiting are observed, in severe cases - unconsciousness. After a few days, vision begins to deteriorate (up to complete blindness). On examination, the pupil is dilated and the reaction to light is weakened. The fundus is not deformed, although symptoms of ischemic neuritis may appear. Without treatment within a month, visual acuity may be restored, but with subsequent deterioration.
Alcohol and tobacco intoxication develops with chronic alcoholism and abuse of strong varieties of tobacco. Neuritis affecting the papillomacular bundle is diagnosed mainly in men over 30 years of age. The course of inflammation is similar to retrobulbar neuritis: mild hyperemia of the disc, the presence of a central scotoma. It is possible to improve visual acuity by giving up bad habits.
Advantages of treatment in Israel
- High level of qualifications and experience of doctors.
- Equipping clinics with modern equipment.
- Development of an individual comprehensive therapeutic program.
- Comfortable conditions for staying in the clinic.
- Reasonable prices.
Completing a full course of therapy in the initial stages of the disease will make it possible, after a short time, to restore visual functions and return to normal life. Don’t waste time, contact the clinic of your choice and start treatment.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)
The main directions of therapy for descending neuritis
Many patients are concerned about the question - if there is no specific treatment for MS, what kind of therapy is carried out for retrobulbar neuritis.
- Experts note that treatment is aimed at achieving several main goals:
- slow down the activity of the immune system, which destroys the body’s own cells;
- change the course of multiple sclerosis;
- eliminate or reduce the severity of ophthalmological symptoms; prolong periods of remission, ease periods of exacerbation.
To achieve these goals, predominantly medicinal methods are used.
First aid for retrobulbar neuritis
Before determining the cause of retrobulbar neuritis, antibacterial and anti-inflammatory therapy should be carried out. Urgent desensitization, dehydration, correction of immunity and measures to improve metabolism in the tissues of the central nervous system are prescribed.
Broad-spectrum antibiotics are prescribed by injection for a week. Do not use ototoxic drugs (Streptomycin, Gentamicin, Neomycin), which have a negative effect on the optic nerve. Corticosteroids are considered safe: Dexamethasone 1 ml every day (10-15 procedures), Prednisolone 0.005 g (4-6 times a day) for five days.
Therapy for retrobulbar neuritis:
- Diacab (Acetazolamide). 0.25 g of the drug 2-3 times a day. The course of treatment is three days. In parallel, Panangin is prescribed two tablets three times a day.
- Glycerol. 1-1.5 g/kg.
- Magnesium sulfate 25%. Intramuscularly 10 ml.
- Glucose 40% intravenously and Solcoseryl (Actovegin) intramuscularly.
- Hexamethylenetetramine solution 40%.
- Adrenaline solution 0.1%. Tampons in the middle nasal passage for 20 minutes.
- Piracetam (Nootropil). Up to 12 g/day.
- Dibazol. 10 mg twice a day for 2-3 months.
Similar therapy is indicated for bilateral toxic neuritis, which developed against the background of methyl alcohol poisoning. Only antibiotics are excluded.