Everyone is familiar with the feeling of sharp pain as a result of an elbow strike. It’s as if an electric current shoots through the arm from the elbow joint to the little finger, sometimes radiating up the shoulder. This occurs due to contusion of the ulnar nerve. Compression of the nerve at the elbow joint is called cubital tunnel syndrome or cubital tunnel syndrome.
The disease is the second most common among carpal tunnel syndromes, second only to carpal tunnel syndrome.
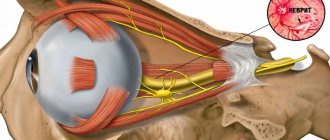
Anatomy of the ulnar nerve and cubital tunnel
The ulnar nerve originates in the cervical plexus, being one of the three main nerves of the upper limb. It runs along the inner surface of the shoulder, then lies in the canal formed by the olecranon process, the internal epicondyle and the ligament that connects these two bone formations, forming a rather narrow cubital canal.
Next, the nerve passes through the intermuscular space of the forearm, flowing into another channel, this time on the wrist. This canal is called the Guyon Canal. It is at the level of this canal that the ulnar nerve begins to divide into 3, sometimes 4 branches, ending with the sensory branches of the 5th and inner half of the 4th fingers, as well as the motor branches of the 3-4-5 lumbrical muscles of the hand.
How does compression of the median nerve manifest?
Through the carpal tunnel (the same as the carpal tunnel), the median nerve passes to the hand at two levels: through the wrist joint and above it. The sensitive part of the median nerve passes over the joint, which on the hand itself is divided into small branches, and these branches are different for each person - concentrated or scattered. Inside the wrist joint there is a muscle branch that goes to the thumb and allows you to clench your hand into a fist.
The first sign of the syndrome is bursting night pain in the hand. “Goosebumps” run all over the fingers of the hand, except the little finger. The pain is exhausting and excruciating and can radiate to the forearm or shoulder. A person wakes up in the middle of the night in pain and has to get up to rub his hand, put it down and shake it. When the hand goes down, the pain subsides, but when you try to lift it, it resumes. Sometimes you have to spend several hours like this. The hand swells, women cannot wear their usual rings. If you tap your wrist, the pain intensifies. It becomes difficult to retract the thumb. Simple housework - wringing out clothes, knitting, sewing - causes pain even during the daytime.
If the median nerve is compressed in the upper part of the forearm, the forearm will become very painful. This happens to those who, due to the nature of their work, often have to turn their hand up and down while holding an object with their fingers. These are drivers, carvers, hand milkers, painters, and artists. The pain first appears after carrying heavy loads, when the main load falls on the forearm, usually after lifting a heavy box or crate. If you clench your hand into a fist and sharply turn it down, the pain will instantly intensify. Difficulties are caused by writing and raising your hand up. The muscles at the base of the thumb may undergo atrophy.
Compression of the median nerve in the lower third of the shoulder is called “lover's palsy.” This condition occurs in those on whose shoulder a person sleeps for a long time and serenely. Of course, this is not real paralysis, but the same pain, numbness and impaired movement.
Causes of cubital tunnel syndrome
The cause of this particular disease is compression of the nerve in the cubital canal. In this article we do not discuss nerve injury.
There are several causes of cubital tunnel syndrome:
- repeated trauma to the ligaments and bone structures of the elbow joint that form the canal,
- intense sports,
- arthritis, arthrosis of the elbow joint
- synovitis of the elbow joint or hemarthrosis
- repeated monotonous activities,
- consequences of fractures can also be the causes of the syndrome.
For drivers, the disease can be caused by the habit of placing their elbow on the window opening of the car door. When symptoms appear, this habit will have to be eradicated.
At the computer, you should pay attention to the position of your hand when working on the keyboard and mouse. When doing this type of work, the forearm should rest completely on the tabletop. You can put something soft under the sore elbow.
Compression of the ulnar nerve in the canal can be caused by inflammatory processes not only in the nerve tissue, but also in the soft tissue component of the cubital canal wall. For example, with medial epicondylitis, inflammation in the projection of the internal epicondyle can cause swelling and compression of the nerve. Failure to consult a doctor in a timely manner and delays in starting treatment can lead to organic damage to the wall and the process becoming chronic. As a result of the thickening of the nerve sheath, the transmission of nerve impulses may become difficult, leading to loss of sensation and motor function in some muscles of the hand and forearm.
Clinical manifestations
The full picture of tunnel syndrome includes sensory (pain, paresthesia, numbness), motor (decreased function, weakness, atrophy) and trophic disorders.
Various clinical course options are possible. Most often it starts with pain or other sensory disorders. Less commonly, it begins with movement disorders. Trophic changes are usually expressed insignificantly and only in advanced cases. The most characteristic feature of carpal tunnel syndrome is pain. Typically, pain appears during movement (load), then occurs at rest. Sometimes the pain wakes the patient up at night, which exhausts the patient and forces him to see a doctor. Pain in tunnel syndromes can include both a nociceptive component (pain caused by inflammatory changes occurring in the area of the nerve-canal conflict) and a neuropathic component (due to nerve damage). Tunnel syndromes are characterized by manifestations of neuropathic pain such as allodynia and hyperpathy, a sensation of electric current passing (electrical shooting), and burning pain. In later stages, pain may be due to muscle spasms. Therefore, when choosing pain therapy, it is necessary to be guided by the results of a thorough clinical analysis of the characteristics of the pain syndrome. Motor disorders arise as a result of damage to the motor branches of the nerve and manifest themselves in the form of decreased strength and rapid fatigue. In some cases, the progression of the disease leads to atrophy and the development of contractures (“clawed paw”, “monkey paw”).
With compression of arteries and veins, vascular disorders may develop, which is manifested by pallor, a decrease in local temperature, or the appearance of cyanosis and swelling in the affected area. With isolated nerve damage (in the absence of compression of arteries and veins), trophic changes are most often insignificantly expressed.
Signs and symptoms of cubital tunnel syndrome
Symptoms of cubital tunnel syndrome include each of the following:
It is not necessary to have all the signs.
- Stiffness, loss of sensation, or significant dull or sharp pain in the ulnar part of the hand, 4th and 5th fingers.
- Pain and weakness when attempting to grasp an object with a brush.
- Discomfort in the elbow area.
Such symptoms indicate ischemia (lack of blood supply) of the nervous tissue. These symptoms are most pronounced in the morning, after the hand has been resting overnight. After some time, when the patient performs a certain amount of movements, the pain and numbness slightly recedes.
Rehabilitation
The recovery period takes at least six months. First, touch is restored, then sensitivity when touching two points. For recovery, it is important to recognize objects by touch.
Principles of successful rehabilitation:
- Early intervention;
- Reducing the risk of complications;
- Ensuring healing;
- Restoring the functions of the nerve of the hand;
- Using a multi-stakeholder approach.
Restoration of the hand nerve is carried out at the clinic of the Central Clinical Hospital of the Russian Academy of Sciences, in the department of hand microsurgery. Everything is available here for effective treatment of a nerve rupture in the arm - experienced, highly qualified surgeons work, the most modern microsurgical equipment is used, and the staff is caring.
Registration for a consultation is carried out on the website. You can get the information you are interested in and find out the price of treatment by calling the number provided.
Diagnosis of cubital tunnel syndrome
When examining the elbow joint by a doctor, the patient may notice a significant increase in pain. A painful examination is necessary for a specialist to make an accurate diagnosis:
- If the nerve is compressed in the canal, there will be a positive Tinnel's sign, which is manifested by the sensation of a current shooting through the nerve into the little and ring fingers when the doctor taps with a neurological hammer - although this can happen when the nerve is without pathology, with a strong blow.
- The doctor will check to see if the nerve slips out of the canal when the patient bends the arm at the elbow.
- Tests sensitivity and strength in the hand and fingers.
If the doctor has doubts about the causes of cubital tunnel syndrome, the patient may be recommended to undergo additional examinations, such as MRI, ENMG, and radiography.
Radiography. Based on radiographs, it is possible to determine bone exostoses in the projection of the canal, which compress the nerve. But most of the causes of compression of the ulnar nerve cannot be seen on x-ray, since they are of soft tissue etiopathogenesis.
Electroneuromyography (ENMG). This study makes it possible to determine how well the impulses are transmitted along the nerve and to determine at what level and how much the nerve is compressed.
During nerve conduction testing, the nerve is stimulated proximally and the time required to conduct the impulse is measured and compared with normal values.
results
All patients examined and operated on in our clinic had previously sought advice from other medical institutions, but in 60% of cases an erroneous diagnosis was made. Cervical osteochondrosis was diagnosed in 39 (45.8%) patients, diabetic polyneuropathy - in 5 (5.88%), osteoarthritis of small joints of the hand - in 3 (3.53%), rheumatoid arthritis - in 2 (2.35%) , Raynaud's syndrome - in 1 (1.17%), toxic polyneuropathy - in 1 (1.17%). It should be noted that all patients had a characteristic clinical picture of CTS.
A thorough neurological examination with identification of areas of impaired sensitivity, assessment of hand strength, and performance of specialized Tinel and Phalen tests in other medical institutions was performed in only 17 (20%) patients. In 21 (24.7%) patients, an MRI of the cervical spine was performed, which revealed degenerative changes, which led to an erroneous diagnosis of the vertebrogenic nature of the pathological manifestations.
Previous treatment of patients with compressive neuropathy of the median nerve was reviewed. It was found that 51 (60%) patients were prescribed non-steroidal anti-inflammatory drugs (NSAIDs), B vitamins and vasoactive drugs. Of these, only 7 (8%) patients noted a slight decrease in the severity of symptoms for a period of less than 3 months. Intracanal administration of GCS was performed in 18 (21%) patients; only 3 of them had injections performed in other medical institutions. A positive effect from the administration of GCS was obtained in 15 (18%) patients, but its duration did not exceed 4 months, 15 (18%) patients were not prescribed treatment. Wearing a brace at night and reducing wrist load was not recommended for any patient. 33 (39%) patients received physiotherapeutic treatment for the cervical spine and wrist, 5 (6%) patients were offered surgical intervention on the cervical spine to eliminate degenerative changes in the intervertebral discs identified on MRI.
As an example of typical medical practice and diagnostic errors, we present the following observation.
Patient S.
, 60 years old, complained of a constant feeling of numbness, burning, tingling in the area of the I-III and half of the IV fingers of the right hand, weakness of the I-III fingers of the right hand, shooting pain in the wrist and I-III fingers of the right hand. For the first time, a transient feeling of numbness at night appeared in fingers I-III about 8 years ago. The patient sought medical help at the clinic at her place of residence, where she was prescribed an MRI of the cervical spine; based on the results of the study, a diagnosis was made: osteochondrosis of the cervical spine, herniated intervertebral discs CV-CVI, radiculopathy of the CV-CVI roots on the right. With this diagnosis, for 5 years with a frequency of 2-3 courses per year, she was treated with NSAIDs, B vitamins, neurometabolic drugs, and received physiotherapeutic treatment for the cervical spine without significant effect. Over the past 2 years, numbness has become permanent, a burning sensation and tingling sensation have appeared in the fingers, the number of night awakenings from pain and paresthesia in the fingers has increased, there has been an increase in weakness in the 1st-3rd fingers, difficulties in grasping small objects (difficulty in holding a pen, art brushes, fastening buttons), and therefore was forced to stop her professional activities.
In September 2021, the patient contacted the clinic for nervous diseases A.Ya. Kozhevnikova. From the anamnesis it became known that the patient had been working as a decorative artist for 40 years and was fond of knitting and sewing. The neurological status revealed a decrease in strength in the right hand to 4 points, a decrease in temperature, tactile, pain sensitivity in the I-III and half of the IV finger of the right hand, a positive Tinel sign and a positive Phalen test on the right, atrophy of the thenar
on right.
According to the results of ENMG of the right median nerve, gross damage to motor and sensory fibers in the wrist area was revealed. Ultrasound of the right median nerve revealed signs of compression neuropathy of the median nerve at the wrist level.
The patient was clinically diagnosed with compression-ischemic neuropathy of the right median nerve. Right carpal tunnel syndrome. Given the duration of the disease, surgical treatment is recommended. However, at the time of examination, the patient refused it for family reasons. To reduce the severity of the symptoms of the disease, she was recommended to wear an orthosis at night, an injection of novocaine and dexamethasone was performed in the projection of the right carpal tunnel, after which the patient noted a decrease in sensory disturbances, the duration of the effect was about 2 months. Subsequently, due to the return of previous symptoms of the disease, decompression of the right median nerve was performed using a minimally invasive approach. 1 month after surgical treatment, the patient noted complete regression of pain both during the day and at night, disappearance of paresthesia, improvement in sensitivity and fine motor skills of the right hand. After 3 months, the patient was able to use an art brush without difficulty and returned to professional activity.
In the presented observation, in a patient with compressive neuropathy of the median nerve, the symptoms of the disease were regarded as a manifestation of cervical osteochondrosis and radicular syndrome at the CV-CV level, as a result of which she did not receive adequate treatment for more than 5 years. It is significant that a decrease in the severity of symptoms during blockade with GCS in the projection of the carpal tunnel and regression after decompressive surgery were achieved despite a long history of the disease. A thorough history, examination data and examination results allowed us to establish the correct diagnosis and prescribe treatment, which led to complete professional rehabilitation.
Treatment of cubital tunnel syndrome
The vast majority of such cases of the disease require non-surgical treatment. Non-surgical treatment options for cubital tunnel syndrome include:
- load reduction,
- temporary refusal of intense training,
- taking anti-inflammatory non-hormonal drugs.
Good remedies for treating cubital tunnel syndrome are anti-inflammatory non-steroidal ointments, taking vitamins and the patient undergoing a course of physiotherapy.
Surgical treatment of cubital tunnel syndrome is prescribed if therapeutic methods have not produced results after 12 weeks. During surgery, segments of the canal wall are removed from the patient and the tendon arches are cut. If it is impossible to expand the canal surgically, the nerve is completely removed from it, placing it between muscle tissue and fatty tissue.