Literally, the word “schizophrenia” is translated from Greek as “splitting / splitting of the mind / thinking.” With this disease, a person loses the ability to adequately perceive himself and the surrounding reality. This pathology has many forms and types. Each of them has its own symptoms. Impaired thinking in schizophrenia is observed in almost all cases. In this article we will consider the main aspects of this problem.
In this article
- Key Features
- What is thinking
- Operational aspect
- Motivational aspect
- Cognitive sphere in schizophrenia
Key Features
Most people believe that schizophrenia is a split personality disorder. However, this is too simple a definition. In fact, it is a more complex mental pathology that covers many different disorders. Most of them have nothing to do with the formation of new personalities in a person’s head.
According to ICD-10, a diagnosis of schizophrenia (F20.0-F20.3) can be made if at least one of the following symptoms is observed:
- Putting/taking away thoughts, their openness to others, “echo” of thinking. It seems to a person that strangers hear his thought process (or other people influence him by planting ideas or replacing memories).
- Crazy ideas. First of all, schizophrenics are concerned about delusions of influence. They are sure that their body or thoughts are influenced by surrounding or otherworldly forces, for example, aliens.
- Hallucinations - auditory, visual and tactile. Patients hear, see and touch what is not in reality.
- Persistent delusions. They are associated with culture, politics, invention, etc. As a rule, such nonsense sounds ridiculous or even fantastic.
A person may also be diagnosed with schizophrenia if two of the following signs are present:
- Persistent hallucinations of any type, accompanied by delusions, which appear over the course of a month.
- Sperrungs and neologisms are breaks in thinking, the use of non-existent words in speech.
- Catatonic syndrome - psychomotor (motor) disorders. The patient is either highly excited or falls into a stupor, freezing in an unnatural position for several hours.
- Negative symptoms: apathy, poverty of speech, lack of initiative, loss of interests, inadequacy of emotions, alienation, etc.
The last group of symptoms, negative, can also be observed in depression. However, in the presence of hallucinations, sperrungs or catatonic syndrome, which develop against the background of apathy and other signs of a negative type, the question arises of making a diagnosis of schizophrenia.
What are the reasons for this problem?
In most cases, a disorder of human thinking processes occurs due to biological pathologies and disorders. They provoke lesions of the brain substrate of various types. Moderate or mild forms of the disorder can be triggered by individual characteristics in the formation of reactions to stress and other traumatic situations that arise in life. Among the most common causes of thought disorder syndrome are:
- biochemical changes occurring in brain cells;
- TBI;
- psychoses;
- degenerative pathologies of the central nervous system;
- epilepsy;
- inflammatory processes of the central nervous system;
- malignant and benign neoplasms formed in the brain;
- neuroses, stress.
What is thinking
Thinking is defined differently depending on the research methodology and the discipline within which it is studied. Moreover, this category has worried many thinkers for several millennia. In simple terms, thinking is the mental process of identifying patterns in the world around us based on the values and judgments that are embedded in the brain.
However, other definitions are possible. Thus, thinking can be understood as the highest stage of information processing or the process of finding connections between objects. In neuroscience, this concept refers to the creation of complex intellectual objects from simple ones. In almost all disciplines, thinking is studied as one of the highest mental functions.
In the context of psychiatric disorders, physicians are primarily interested in such aspects as operationality, motivation, as well as the ability for associative, abstract and other types of thought processes.
At the same time, thinking in schizophrenia is almost always impaired. If you carefully study the symptoms of the disease, partially described earlier, it becomes clear that most of its symptoms directly or indirectly affect the thought process or other cognitive abilities.
We will find out exactly how schizophrenia affects different aspects of thinking, primarily operational and motivational.
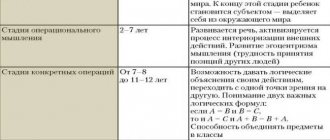
Operational aspect
Operational thinking is the ability to generalize available judgments. When analyzing this criterion, the following parameters are taken into account:
- reduction in the level of generalization;
- distortions in the generalization process;
- weakening of the categorical structure of thinking.
Let's analyze each indicator separately.
Reducing the level of generalization
If the first sign is present, a person cannot compare objects with each other, analyze the situation and generalize the information received, working with complex terms. He simply operates with general features, being unable to identify something important or specific in order to fully reveal the content of the concept.
For schizophrenics, a decrease in the level of generalization is not typical, especially at the early stage of development of schizophrenia. Typically, such symptoms are typical for patients with an oligophrenic type of disorder or patients taking antipsychotics, which are reflected in the operational side of thinking.
To obtain such indicators, simple techniques are used:
- "Classification of objects." A person is given a group of cards and asked to distribute them according to certain characteristics.
In severe cases, the patient cannot master the instructions for the task. In lighter ones, it forms classes based on uncharacteristic properties - elongated, yellow or starting with the letter “m”. In such generalizations there is no clear pattern that would reveal the true content of concepts. Thus, a subject may group scissors, a coil, and a tube into one class on the basis that all of these objects have holes. He cannot give a name to the formed group.
- "Exclusion of items." The patient excludes objects from the class based on unimportant criteria (“there is no glass here”). As a result, he copes only with very simple tasks, when an animal must be excluded from four cards on which three plants and one cat are depicted. As in the first case, there are problems with the names of the groups.
- "Pictograms". The patient is offered a list of words that he must remember. At the same time, he needs to draw something on paper that will help him correctly reproduce the resulting list. With schizophrenia, patients demonstrate specifics with personal experience, for example, “I came home from work, undressed, put the kettle on, lay down on the sofa,” etc. In a healthy person, the drawing will be more concise.
These techniques are developed not only for schizophrenics. They can also be used to examine healthy people, including children.
Distortion of the generalization process
This symptom is observed at a later stage of schizophrenia. It is associated with the qualitative characteristics of objects and concepts. The patient can operate with complex intellectual objects, but at the same time relies on their latent properties. This means that they are inherent in the phenomenon, but are not directly related to its content.
The following method can be used as an example. The patient is given cards with images of a beetle, an airplane, a bird and a butterfly. A healthy person will focus on concepts such as “animate / inanimate”, “technology / animal”, etc. However, in schizophrenia, a patient may exclude a beetle from the group just because it is depicted on a black and white card.
One patient may show signs of generalization distortion but not show symptoms of decreased generalization.
If the “pictogram” technique is used, then the patient has difficulties with abstractions - “sadness”, “doubt”, “torment”. In such cases, the phonetic features of the terms act as latent features. As a result, the patient, in order to remember them, draws objects that are consonant with the proposed words, for example, a seal (“sadness”), a catfish (“doubt”) and a bag of flour (“flour”).
Category thinking disorder
A disorder or weakening of categorical thinking is observed in cases where there is a departure from the correct thought. This phenomenon is called slippage. In general, the patient makes correct judgments, but makes isolated errors. He formulates a chain of conclusions, but at some point he gets lost. Next, he restores the thought process and continues the reasoning, but without correcting the erroneous link.
Diagnostic methods
To prescribe a suitable treatment option, a person seeks help from a psychiatrist. Only a doctor can determine the type of thought disorder and the causes of its occurrence. Many people with banal neurosis associated with stress or fatigue suspect serious mental disorders. This thought does not leave you alone, so to determine the problem it is necessary to undergo a thorough examination. To make a diagnosis, the doctor:
- collects life and family history;
- talks with the patient’s closest relatives;
- communicates with the patient;
- prescribes procedures that will confirm or refute the presence of brain pathologies that can lead to disruptions in the thought process.
Based on the results of these procedures, a diagnosis is made and treatment is carried out.
Motivational aspect
The motivational and personal component of thinking is one of the most important in the study of mental disorders. Thus, in almost any form of schizophrenia, especially at an early stage or before an attack, there are symptoms such as apathy and lack of initiative. Any person should be interested in his destiny. If there is no concern for the future, then there will be no motivation to do anything to achieve it.
Moreover, it is important to note that there are two aspects of apathy. The first is associated with complete insensibility, which is observed in severe patients. The second is typical for milder cases, when apathy is considered as a common lack of motivation. With the first, everything is clear without an examination, but the second type of patient is sent to experts for examination, during which three main criteria are assessed:
- diversity of judgments;
- reasoning;
- criticality violations.
Let's take a closer look at each.
Diversity of judgments
With schizophrenia, a person’s judgments become contradictory. Their thought process can proceed on different planes, while the patient does not perceive such logical contradictions as errors. This is due to the lack of a clear goal for which the conclusion is formed.
In fact, the patient has several plans to solve one problem, each of which may be completely unrelated to the other. Moreover, one of them may contradict the second, but the patient does not understand this. Often one goal is dictated by the desire to complete a task, and the second is related to personal preferences.
The following case can be cited as an example. The patient is asked to distribute the cards into groups. At first he does this correctly, explaining everything clearly and logically, since the process of generalizing judgments, in principle, works well. Then he changes his mind and excludes mushrooms from the group on the basis that he was once poisoned by them and therefore does not eat them anymore.
In this case, there is a lack of goal setting. In everyday life, this will interfere with decision-making. As a result, a person may refuse to perform certain actions altogether.
A particular example of the diversity of thinking is its fragmentation, when the patient’s speech turns into a “word salad.” The beginning of a phrase refers to one situation, the middle to another, and the end to a third. In mild forms of schizophrenia, the patient may temporarily wander away from the topic due to various associations. However, he is still able to return to the topic, especially with support from a specialist.
Based on one conversation with a person, it is impossible to draw a conclusion about the fragmentation or diversity of thinking. It is necessary to carry out various techniques, including “classification” and “exclusion of items”. If contradictions appear when performing most of the tasks, appropriate conclusions are drawn about thinking disorders.
Reasoning
Reasoning is typical idle talk, a tendency to meaningless reasoning, fruitless philosophizing, which does not lead to the formation of a full-fledged intellectual product. This phenomenon is typical not only for sick people, but also for healthy people.
As an example, we can mention a student’s uncertain answer in an exam, when he does not know how to fill in his lack of knowledge of a particular subject. In such cases, he simply talks about what comes to mind, just so as not to remain silent. In general, this is an adequate human reaction to a complex and unpredictable situation. In a sense, he's just buying time.
In schizophrenia, idle talk occurs without any purpose, out of nowhere. In this case, the patient usually speaks pretentiously, pretentiously or mannered, trying to impress. He can speak with a smart look and complete platitudes that do not require any philosophizing. He does not listen to the opinions of other people at such moments. It is simply important for him to speak, especially on topics that are directly related to him. As a result, the speech turns into a long and lengthy monologue that has no clear content.
Criticality Violations
Uncriticality is characterized by a loss of purposefulness of thinking, its incompleteness. The thought process ceases to be a regulator that limits and controls a person’s actions.
To assess criticality, a simple test, or Ebbinghaus test, is performed. The patient is offered a text with gaps that he must fill in with words. He selects concepts himself, based on subjective opinion. However, in the end he must prepare a logically coherent and understandable text.
Then the expert reads it. If contradictions are detected, he asks the patient to find and correct them himself. Then the error correction rate begins to be assessed. If the subject does not see the errors, the experimenter points them out, but the patient must still make corrections on his own.
Experts distinguish three types of criticality:
- to the presence of a disease or specific symptoms;
- personal;
- to the effectiveness of their activities during experiments.
The last type of criticality is directly related to thinking. The doctor points out mistakes, and the patient corrects them. A healthy person should be interested in this, since he has a goal and his fate is important to him. A schizophrenic is usually indifferent to comments. If he was told that he did something wrong, he will accept it and do nothing. In other words, he doesn’t care - “whether it’s will or not.”
The described complex of symptoms of thinking damage is not observed in all patients. It all depends on the specific form of pathology and its stage.
Schizophrenia affects not only thinking, but also other cognitive abilities of a person - perception, attention and memory. Let's touch on them, since they are largely related to the subject discussed in the article - the thought process.
Memory impairment
During a pathopsychological examination to identify memory pathology, the following questions seem most important:
- the problem of the structure of mnestic activity of mediated and non-mediated, voluntary and involuntary memorization;
- the question of the dynamics of the mnestic process;
- question about the motivational component of memory.
Korsakoff's syndrome is an immediate sign of memory impairment. One of the most studied disorders of immediate memory is a memory disorder for current events, in which memory for past events remains relatively intact, the so-called Korsakov syndrome, which was described by the famous Russian psychiatrist S.S. Korsakov in severe alcohol intoxication. This type of memory impairment is often combined with confabulations about current events and disorientation in place and time. The last two signs could be weakly expressed, but the first is always extremely pronounced and constitutes the main radical of this suffering (forgetting current events).
Pathopsychological examination revealed progressive amnesia. Memory impairment often extends not only to current events, but also to past ones: patients do not remember the past, confuse it with the present, they shift the chronology of events; disorientation in time and space is revealed. At times such memory disturbances are grotesque in nature.
Violation of mnestic activity
The memory impairments described above, identified by pathopsychological examination, were mainly stable. Although the degree of their severity could change, the main radical of these disorders (violation of temporal characteristics, amnestic disorientation) remained persistent.
In other cases, the memory of mentally ill patients may be impaired in terms of its dynamics. Patients remember and reproduce material well for a certain period of time, but after a short time they cannot do this. Fluctuations in their mnestic activity come to the fore. If such a patient is asked to remember 10 words (with ten presentations) and depict the number of words reproduced in the form of a curve, then the latter will have a broken character. The patient can remember 6-7 words after the second or third presentation, after the fifth - only 3 words, and after the sixth - again 6-8.
It is noteworthy that such disturbances in the dynamics of mnestic activity rarely appear in patients as an isolated monosymptom. Pathopsychological examination reveals the lability of all forms of their activity, their cognitive and effective-emotional spheres.
Violation of the dynamics of mnestic activity manifests itself in combination with the intermittency of all mental processes of patients and is essentially not a memory impairment in the narrow sense of the word, but an indicator of the instability of the mental performance of patients in general, its exhaustion.
Violation of mediated memory
Memory is a complex organized activity that depends on many factors, the level of cognitive processes, motivation, dynamic components, mental illness. By changing these components, it also destroys mnestic processes in different ways. The introduction of a mediation operation improves the memory of healthy people. However, in a number of patients with memory impairment, the mediating factor becomes an obstacle.
Thus, the violation of controllability, selectivity of mental processes, the replacement of the purposefulness of the act with stereotypes or random fragmentary actions were factors that impeded the process of mediation, making it fundamentally impossible. Disturbances in mnestic activity reflect the differently altered structure of the motivational sphere of patients. The motivational component is integral in the structure and flow of memory processes.
Cognitive sphere in schizophrenia
First of all, schizophrenia is reflected in the perception of the surrounding reality. Changes in this area may indicate the beginning of the development of a psychopathological process, which will subsequently affect a person’s thinking and emotionality. He begins to perceive the world too subjectively, which leads to limited judgments, unrealistic or fantastic ideas.
Changes in perception are assessed using the Rorschach test, which consists of showing the patient pictures with unusual images. The subject must say what exactly he sees on the cards. As a rule, he is shown three types of images:
- deficient - “man without a head”;
- dissociative - “flattened cat”;
- symbolic - “punishment of evil.”
Analysis of the test is quite complex. You can go through it on the Internet, but you should not draw any conclusions. Only a specialist can give a normal assessment.
Attention also has its own distinctive features in schizophrenia. It is disrupted even when the patient’s memory and high intellectual level are preserved. This indicator is studied using the Schulte test, or “switch counting,” which determines how quickly a person voluntarily or involuntarily switches from one object to another. Usually, in schizophrenia, voluntary attention suffers more. At the same time, the subject does not dwell on the indicated errors, and practically does not react to the experimenter’s reactions.
Memory in schizophrenia can suffer when motivation decreases. But this phenomenon is also quite complex. In some patients it remains completely, in others it disappears partially or completely. Sometimes the patient cannot say for sure whether a particular event occurred or not.
There is also a symptom of schizophrenia called confabulation, when the brain is filled with false memories. The current ability to remember, that is, short-term memory, is tested using tests, including the “pictogram” technique.
Schizophrenia can take years to develop. Before the first attack, a person almost always does not understand that he is sick. When he is taken to the clinic, which happens during an exacerbation of the disease, a complex of symptoms is already observed. Some of them are associated with formal thinking disorders, including meaningfulness, flexibility and criticality. The degree of brain damage is determined by the type of schizophrenia and the intensity of its development.