Migraine with aura differs from the classical form of the disease in the appearance a few minutes or an hour before the attack of precursors in the form of disturbances in vision, hearing, coordination of movements or general well-being. To determine the disease, additional examination regarding aura symptoms is required. Treatment achieves relief of the onset of an attack and a maximum extension of the period until the next one.
Pathology accounts for approximately a quarter of all cases of this disorder. Like classic migraine without aura, it occurs more often in women, especially during childbearing years. The aura lasts a maximum of 60 minutes and goes away with the onset of the attack. If it is prolonged, which is not often the case, then with the onset of pain it persists and may be present for a considerable time. In some patients, pain after an aura does not always occur. In this case, after the aura passes, the state is completely restored. If the aura persists for more than 7 days, then there is a high probability that the patient has experienced a complication of the pathology and developed a migraine infarction. It is detected through examination using neuroimaging methods.
The frequency of migraine attacks with aura is individual for each patient. On average, there are from 2 to 8 attacks per month, but cases are also diagnosed when the disease manifests itself only 2 times a year or, conversely, torments a person almost constantly, making it impossible to lead a normal life and leading to disability. Most often, the disease first appears between the ages of 16 and 20 years, when active hormonal changes occur in the body. The disease is hereditary, and a child has a 90% chance of developing the problem if both parents suffer from the disorder.
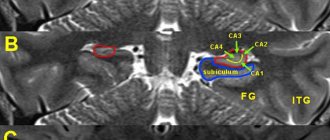
The most common is the visual aura. In this case, there are usually no symptoms from other systems, and the patient is only bothered by visual disturbances.
Causes
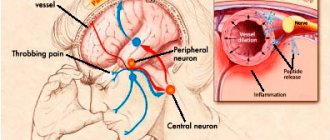
The main reason for the occurrence of an attack is short-term oxygen starvation of the brain, which develops due to spasm of the vessels that feed it. What directly causes the disease itself has not yet been precisely established. Doctors name hereditary predisposition and hormonal changes as the main, most likely causes.
There are many factors that can cause an attack to develop. Doctors know them well. The patient himself can determine what is causing his condition to worsen. Most often, the provocateurs of an attack are:
- drinking large portions of coffee;
- severe stress;
- nervous tension;
- emotional stress;
- lack of sleep;
- hard physical work;
- long stay in stuffy conditions;
- prolonged exposure to the sun;
- a sharp jump in atmospheric pressure;
- rapid changes in weather or climate;
- starting to take oral hormonal contraceptives or abruptly stopping them;
- the beginning of menstruation;
- certain foods, especially those with a high caffeine content, as well as hot and spicy foods;
- unauthorized use of vasodilator drugs;
- prolonged exposure to flickering light;
- prolonged exposure to bright light;
- drinking large amounts of alcohol.
Without a provoking factor, the development of migraine with aura is also possible, but somewhat less common. Moreover, in most of these cases, the factor that caused the headache occurred, but simply went unnoticed. Identifying the triggers of attacks is important for prescribing the correct therapy and reducing the negative impact of the disease on the body.
In children, the pathology is not common, but it can occur. It is not so easy to determine which factor caused a negative phenomenon in a child. This is due to the fact that often a patient who is passionate about his work does not immediately notice the appearance of an aura if it is not very pronounced. As a result, migraines can sometimes be misdiagnosed as simple migraines.
Patients are advised to keep a headache diary, which will note the factors that acted before the attack developed. Ideally, write down in such a diary everything that happened on the day of the attack: from how long the night's sleep lasted to the foods that were eaten. Such recordings for monitoring standing are necessary, as they allow a person to better analyze what is happening to him, and also help the doctor assess the patient’s condition.
Symptoms of an epileptic seizure
Epileptic seizures in women, men and children occur as a result of an imbalance between inhibition and excitation of neurons in certain areas of the cerebral cortex. The International Classification of Diseases, 10th revision of pathology, assigned the code G40.
Causes of epilepsy in infants, adolescents and adults:
- head and brain trauma (concussion, etc.);
- acute circulatory disorder in the cerebral region;
- infectious lesion of the meninges;
- chronic disease of the central nervous system;
- tumor-like neoplasm in the brain;
- development of parasitic infection in the cerebral region;
- alcoholism and drug addiction;
- hereditary and congenital factor (epilepsy is often inherited).
The diagnosis of epilepsy of any type (focal, absence, etc.) in most cases is made in childhood and adolescence (up to 18 years). Rarely do the first attacks occur in adults.
Symptoms of epilepsy must be differentiated from a nervous (hysterical) seizure. The latter occurs after the onset of a pronounced emotional reaction, for example, with offense, grief, fear. During a hysterical attack, consciousness is retained and the person is aware of his actions.
Clinical picture
At the initial stage of the attack, the patient begins to scream, makes unnatural sounds, loses balance and consciousness, and falls. The body acquires an arched position. Respiratory function is almost completely suppressed. The skin begins to turn pale.
After a few seconds, the body begins to twitch, the pupils dilate, foamy exudate and a large amount of saliva are released from the oral cavity. Due to a sharp increase in blood pressure, the face turns red. Urinary function and the process of defecation may be impaired in the form of urinary and fecal incontinence.
At the time of an attack, you need to move all impact objects away from the person’s location to prevent injury.
After the seizure ends, the body relaxes, respiratory function is restored, and the color of the skin returns to normal.
The above symptoms characterize a generalized form of epilepsy. There is also a focal type of seizures, when the convulsive syndrome covers a certain part of the body. Infants and children under 4 years of age experience febrile seizures caused by elevated body temperature, which are often confused with true epilepsy.
Types of aura
Most often, the patient develops a visual aura. However, besides it, there may be other precursors of an attack. Doctors distinguish the following five forms of the phenomenon:
- visual is the most common aura. The patient experiences visual disturbances and a feeling of blindness in one or both eyes. In severe cases, this phenomenon can lead to the development of a panic state;
- aura with impaired sensitivity - the upper part of the body is affected on one side. The person experiences numbness, pins and needles, or tingling sensations. Disturbances begin with the fingers and, rising along the arm, reach the head and even involve the tongue and lips;
- movement disorders - in this form, before an attack, acute muscle weakness develops in the arm or leg, and less often in the upper and lower limbs at once. In especially severe cases, the entire half of the body may be affected at once, and in exceptional cases, the development of reversible paresis of a leg or arm is noted;
- speech disorders - it turns out to be difficult. The patient speaks indistinctly; it is not easy for him to formulate a sentence so that it makes sense. Finding words is difficult. Additionally, a person may temporarily lose the ability to recognize numbers and letters;
- mixed - an uncommon form in which two or more types of aura develop simultaneously, which is why the patient’s condition turns out to be quite serious.
Sometimes an aura can cause a person even more severe discomfort than the attack of pain itself, since it disrupts normal contact with the world. With this phenomenon, the doctor selects additional treatment for the patient and stronger anti-migraine drugs, so that when signs of aura begin to appear, they can be removed in a short time.
Some patients develop so-called headless migraine, in which the aura is not followed by an attack of pain. In case of such a disorder, treatment will be selected purely individually, depending on the main symptoms and how the body reacts to a particular drug.
Clinical picture
An epileptic seizure itself always occurs suddenly. The patient cannot predict when seizures will occur, so this affects the psychological state: the person lives in constant fear and tension.
In most patients with epilepsy, before convulsive seizures, a so-called aura occurs - a set of precursor symptoms that signal the imminent onset of an attack and are often associated with a mental state.
Features of an epilepsy attack
Epileptic seizures last a long time - from several hours to several days. Considering the type of disease a person suffers from, a different clinical picture arises: short-term disturbance of orientation in space, loss or impairment of consciousness, etc.
In most cases, epileptic seizures do not stop on their own and require therapeutic measures. Medicines are used when a series of attacks is observed and when there is a simultaneous effect of a provoking factor, for example, elevated body temperature.
In addition, each subsequent epileptic attack has a monotonous character. In other words, seizures of the same type occur, which do not differ in symptoms and features of occurrence.
The signs of precursor symptoms, that is, auras that occur before each subsequent attack of the disease, do not change either. Often the clinical picture of an aura is no different from the epileptic attack itself.
Cost of diagnostics in our clinic
| Appointment with a retinologist with diagnostics (adults) | 3,500 rubles |
| Appointment with a pediatric ophthalmologist (standard diagnostics) | 5,000 rubles |
| Comprehensive examination of the retina (angio-OCT, visual fields) | 8,600 rubles |
| Consultation with professor, doctor of medical sciences (including standard diagnostics) | 6,900 rubles |
| Laser coagulation of the retina | from 13,000 rubles |
| Intravitreal injections of anti-VEGF drugs | from 44,000 rubles |
| Microinvasive vitrectomy | from 46,000 rubles |
The treatment plan (if necessary) and its cost are determined individually, after a comprehensive diagnosis. You can find the clinic’s price list for other services for the diagnosis and treatment of retinal diseases in the OUR PRICES section.
List of sources
- Kopaeva V.G. Eye diseases. Textbook. Eye diseases. Educational literature for medical students. Fourth edition, corrected and expanded. Moscow – 2021. DOI:10.25276/978-5-903624-36-2
- Pavlenko S.S. Diagnosis and modern treatment of migraine / SAPF (Siberian Interregional Pain Foundation). – 2005. – P. 1-2.
- Chong YJ, Mollan SP, Logeswaran A, Sinclair AB, Wakerley BR. Current Perspective on Retinal Migraine. Vision (Basel). 2021 Aug 23;5(3):38. doi: 10.3390/vision5030038. PMID: 34449754; PMCID: PMC8396291.
- Hamamci M, Songur MS, Aslan Bayhan S, Bayhan HA. Is ocular vascularity affected in young migraine patients? A pilot study. J Clin Neurosci. 2021 Sep;91:144-151. doi: 10.1016/j.jocn.2021.06.045. Epub 2021 Jul 9. PMID: 34373020.
- Lyskin P.V., Zgoba M.I. Vitreomacular traction. Theoretical and practical aspects of treatment. Russian Children's Ophthalmology No. 1 2021 DOI:10.25276/2307-6658-2019-1-43-51
Material prepared by:
Ophthalmologist Dmitry Alekseevich Sagonenko
How to reduce the frequency of attacks?
It is impossible to cure the disease forever, as it has a chronic form. However, it is possible to prevent the rapid onset of an attack and reduce the frequency of its occurrence. To do this, you need to adhere to the following recommendations from doctors:
- eliminate stressful situations and emotional stress;
- do not be exposed to open flames or bright flashes of light;
- rest more, do not abuse physical activity;
- Maintain a balanced diet and avoid overeating;
- promptly diagnose and treat somatic diseases, infectious and parasitic infections;
- Stop taking alcohol, drugs, and caffeine-containing drinks.
In addition, it is recommended to monitor blood pressure and blood sugar levels and see a neurologist after a stroke. Head injuries should also be avoided.
Many people live with epilepsy and lead normal lives, even with a designated disability group. To reduce the frequency of attacks, it is important to fully comply with the doctor’s instructions (adhere to a ketogenic or other diet, take anticonvulsant pills, etc.). Self-treatment and the use of folk remedies lead to negative consequences.