Catatonia is a psychopathological syndrome with a predominance of psychomotor and autonomic disorders in the motor sphere, characterized by a clinical picture of agitation or stupor, which is unmotivated.
In the International Classification of Diseases (ICD-10), the disorder is considered within the framework of catatonic schizophrenia. This interpretation makes it difficult to diagnose the disorder.
Catatonic states of excitement and stupor can quickly replace each other. They arise autochthonously and are functional in nature. Catatonia may not be accompanied by stupefaction (lucid), or may be accompanied by oneiric stupefaction.
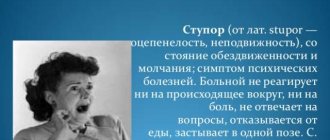
Catatonic stupor is characterized by increased muscle tone and immobility. Stupor can develop quickly or gradually. With gradual development, slowness, angular movements, prolonged freezing in one place (substupor), etc. initially appear. Over time, the severity of stupor increases.
Variants of motor stupor:
- Depressive;
- Catatonic;
- Hallucinatory;
- Apathetic;
- dissociative (“hysterical”);
- affective-shock.
Types of motor excitation:
- Manic;
- Anxious;
- Hallucinatory;
- Delusional;
- Affective-shock;
- Dissociative (“hysterical”);
- Against the background of confusion: delirium, twilight confusion.
Catatonic excitation develops suddenly, often rapidly moving from a state of stupor.
Catatonia is also characterized by other clinical manifestations:
Mutism is an unmotivated refusal to speak during normal functioning of the speech apparatus. Passive and active negativism is an unmotivated refusal to perform actions (for example, changing a position) or performing opposite actions. Motor and speech stereotypies - pretentiousness of movements and facial expressions. Echopraxia and echolalia are unmotivated repetition of the actions and phrases of others.
Causes
Specific reasons for the development of catatonia have not been established. The disorder may be initiated due to:
- Concomitant mental disorders (depression, bipolar disorder, schizophrenia, schizotypal disorder, acute psychosis);
- Substance and alcohol use;
- Neurological diseases (epilepsy, multiple sclerosis, Parkinson's disease, brain tumors, dementia);
- Metabolic and endocrine disorders (Cushing's syndrome, hyperthyroidism, Sheehan's syndrome);
- Autoimmune diseases (systemic lupus erythematosus, antiphospholipid syndrome), etc.
Genetic predisposition to certain mental disorders plays a great role. Some infectious diseases can also cause the development of catatonic stupor.
Pathogenesis
There is no consensus on the pathogenesis of catatonia. Studies have shown that disruption of communication between cortical structures, the thalamus and the basal ganglia play an important role in the occurrence of catatonic symptoms, therefore, in addition to clinical assessment, when studying catatonia, it is worth taking into account the results of neuroimaging and neuropsychological examinations. The hypothesis is based on a lack of gamma-aminobutyric acid (GABA) in the basal ganglia. Normally, GABA reduces the intensity of emotional reactions, such as anger, fear or anxiety.
In modern literature, there are often cases of catatonia caused by abrupt withdrawal of drugs used to treat catatonic states and accompanying mental disorders. This therapy uses mechanisms to increase GABA activity in the basal ganglia, which has a positive therapeutic effect. With abrupt withdrawal of drugs, an increase in motor symptoms often occurs (the phenomenon of “rebound catatonia”).
It is possible that catatonia develops as a result of severe anxiety, in response to stress. Therefore, scientists suggest that catatonic states are directly related to affective and other mental disorders that are accompanied by symptoms of severe anxiety.
Symptoms
There are many clinical signs of catatonic syndrome. Symptoms are often related to the motor area. With catatonic stupor, the patient becomes numb or completely immobile. Muscle tone is increased, especially in the head and shoulder girdle. The chewing muscles are toned, the lips are pulled forward (proboscis symptom), the person lies on his back, holding his head above the pillow (the “air cushion” symptom). Less severe conditions occur in the form of catalepsy. Muscle tone may alternate with complete relaxation, and epileptiform seizures are sometimes observed. The state of catatonic excitement is characterized by incoherent speech, absurd rhyming, and echolalia.
In severe cases, the attack of stupor with catalepsy is prolonged, mutism, lack of reaction of the pupils to intense painful stimuli (Bumke's symptom), and persistent insomnia are noted.
Stupor may be accompanied by oneiric stupefaction, delusions and hallucinations. Motor disturbances manifest themselves in combination with a feeling of stiffness of the body and the inability to move, with stupor, or a feeling of muscle looseness with motor excitement.
In catatonic states, the following symptoms may occur:
- catatonic stupor or substupor - complete or partial immobility, often in a sitting or standing position;
- catalepsy - a person remains in one position for a long time;
- waxy flexibility - long-term preservation of the position that another person gives the patient;
- negativism—resistance when another person tries to change the patient’s position;
- mutism – prolonged silence;
- stereotypy - repeated monotonous movements;
- catatonic agitation - increased disordered motor activity;
- echolalia/echopraxia - copying the words and movements of another person;
- pretentiousness of facial expressions and movements.
In addition to the main symptoms, manifestations of disruption of the autonomic nervous system may occur. With catatonia, there may be an increase in body temperature to subfebrile, a feeling of thirst, increased blood pressure, and tachycardia. Often patients refuse water and food.
The detailed picture of catatonic stupor and agitation does not differ in clinical manifestations in adolescents and adults. Oneiric catatonia often occurs against the background of the manic phase in schizoaffective psychosis; it is much less common in depression and attacks of fur-like schizophrenia, especially in adolescents. Hebephrenic syndrome is characteristic of adolescence and the malignant course of schizophrenia. As a rule, catatonic symptoms appear against the background of this syndrome.
Fibril catatonia develops with symptoms of oneiric, neurological and somatic disorders. A febrile attack is characterized by manic-delusional, hallucinatory and depressive syndromes. With more pronounced psychosis, fantastic delirium appears. The patient is in a state of agitation or stupor.
Body temperature rises sharply to febrile and higher. There is no relationship with somatic and infectious diseases. Blood pressure rises, tachycardia and increased sweating are present. The person is in an excited state and feels very thirsty. Excitement gives way to stupor or sub-stupor. General health worsens. The feeling of thirst and hunger disappears, the skin becomes dry, and swelling appears. If assistance is not provided in a timely manner, congestion in the lungs, bedsores and other complications may develop.
Most often, attacks of febrile catatonia are observed in people 41-50 years old. They are characterized by a severe course and a high risk of death.
With primary manifestations of catatonia, you should immediately consult a doctor. With timely diagnosis and effective treatment, the condition can be normalized without further development of complications.
Amentive clouding of consciousness (amentia)
This is a condition in which the patient completely loses all ability to navigate both in space and in himself and his experiences. Everything he sees and feels is perceived in fragments and is not something whole. The processes of thinking and understanding what is happening are disrupted. of delirium occur
and
oneiric state
, causing fear.
The speech of such people can be thoughtless and incoherent. They are also characterized by a sharp change in activity, that is, excitement can suddenly give way to apathy
and helplessness. My mood also changes unusually often.
The amental state can be quite long - up to several months, and it is sometimes replaced by short periods of “enlightenment”. The dynamics of the disease completely depend on the physical condition of the patient, and this condition itself is characteristic of sepsis and cancer intoxication. In general, the very fact of an amental state, as a rule, indicates a serious illness in the patient.
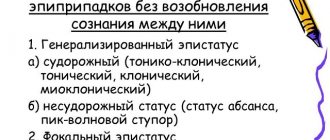
Classification
Catatonic states are classified based on the severity of clinical manifestations and the nature of the course of the disorder. Currently, there are two types of catatonia: benign and malignant. Malignant catatonia is the most severe form of the disorder and poses a threat to the patient’s life (“lethal” or “febrile” catatonia).
Febrile catatonia is an acute mental disorder accompanied by a deterioration in general physical condition: increased body temperature, somatovegetative disturbances, homeostasis disorders, deterioration in the functional ability of body systems. The condition develops without connection with somatic diseases. With such a course of the disorder, there is a possible risk of developing cerebral edema and multiple organ failure
Catatonia that occurs at the onset of the disease is considered primary (often observed in schizophrenia). If catatonic manifestations develop against the background of a prolonged course of the disease, catatonia is secondary.
Often in psychiatry, a classification of catatonia is used, based on the pattern of the underlying disorder and the predominance of catatonia syndrome over other symptoms. According to these signs, minor and extensive catatonia are distinguished.
Mild (small) catatonia
. is a reduced version of the catatonic syndrome, in which some simple manifestations are present. Negativism is not clearly expressed, substuporous states, short-term stops of movements and speech, episodic echolalia, isolated grimaces and unexpected actions are noted. The patient enters into dialogue only under duress, is reluctant to answer questions, his speech is mannered, and he avoids visual and tactile contact with the interlocutor. This condition is most often observed in developing schizophrenia.
According to the degree of severity, catatonic excitation is:
- ecstatic - patients are mobile, talk a lot;
- hebephrenic - ridiculous, inappropriate jokes, unmotivated and unreasonable gaiety predominate;
- impulsive - unexpected actions, often destructive and aggressive;
- silent - motor agitation with aggression and destructive actions.
Silent (mute) catatonic agitation
. The person makes meaningless, chaotic movements and resists other people’s attempts to help. During this period of arousal, there is a risk of harm to yourself and others.
Impulsive catatonic agitation
. Development is fast. A person copies the movements and phrases of nearby people. Speech is limited to a chaotic set of phrases. There is a tendency towards cruelty and destructive actions, and a high risk of self-injury.
Ecstatic
. Symptoms increase gradually. At the beginning, there is little motor and speech activity. The nature of the speech is mannered, echolalia (copying other people's words) is possible, and laughter often occurs for no apparent reason.
Degrees of severity of catatonic stupor:
Cataleptic
(with waxy flexibility). Muscle tone is increased, a person can maintain an uncomfortable position for a long time. Manifested by symptoms: catalepsy, waxy flexibility (maintains a position devoted to another person), “air cushion” (characteristic position on the back with the head raised above the pillow).
With negativism
. More pronounced muscle tension. There is sharp opposition to passive movements and attempts by other people to change the patient’s posture. Mutism is often observed.
Rigid
. Muscle tone is very pronounced. Due to the predominance of flexor muscle tone, the person is in the fetal position (knees brought to the stomach, hands pressed to the chest). Trying passive movements increases muscle tension. Muscle tone decreases during deep sleep.
Catatonic states are divided into two types - oneiric and lucid, depending on the presence of clouding of consciousness. With oneiric clouding of consciousness, ecstatic, impulsive, hebephrenic excitement, stupor with waxy flexibility and substuporous states develop. With lucid catatonia, stupor with negativism often develops.
Oneiric catatonia
combines a state of stupor and a dream-like state with vivid scene-like hallucinations, which the patient can talk about after emerging from the stupor. During stupor, the patient is most often disoriented and unable to perceive surrounding events; perception occurs in a distorted form with dream-like fantasies.
Lucid catatonia
represents a stupor without clouding of consciousness. The perception of what is happening around is not distorted. The patient is normally oriented in time and space, remembers the events that occurred while in a stuporous state. Sometimes partial amnesia occurs regarding one's own movements and behavior. The patient may not remember his own impulsive actions, prolonged immobility, etc.
Taking into account diagnostic approaches, catatonia is classified according to provoking factors:
Catatonia developed against the background of concomitant mental disorders. Most often, catatonic schizophrenia is considered (if motor disorders are the main clinical symptoms of the disorder), affective disorders with catatonic symptoms, and others.
Catatonia due to somatic illness. Catatonic syndrome may indicate neurological, infectious and other diseases with metabolic disorders.
Unspecified catatonia. Catatonic states without correlation with other mental and somatic disorders.
Types of catatonic stupor
Stupor is a motionless, apathetic state in which a person does not notice or respond to external stimuli. Motor activity is practically absent. People in this state see little or nothing of each other and may be mute and rigid. It is possible to stay in one position for a long period of time and then immediately move to another position immediately after the first position.
Catatonic arousal is a state of constant, aimless agitation and agitation. People in this state are extremely hyperactive, although, as mentioned, the activity seems to have no purpose. The person may also experience delusions or hallucinations. It is commonly referred to as one of the most dangerous mental conditions in psychiatry.
Malignant catatonia is the acute onset of agitation, fever, autonomic instability, delirium, and can be fatal.
Complications
The development of complications is often associated with late diagnosis and incorrect approach to treating the disorder.
When treating people with severe forms of catatonia, difficulties may arise in the daily care of patients, as a result of which complications may develop:
- aspiration pneumonia - occurs due to the difficulty of eating in patients with mutism and the risk of aspiration;
- risk of deep vein thrombosis and pulmonary embolism due to immobility in people with catatonia;
- metabolic disorders associated with dehydration and exhaustion of the body - patients with catatonia may not eat or drink for a long time;
- disorders of the gastrointestinal tract (constipation, intestinal obstruction, etc.)
- urinary retention or incontinence;
- neuromuscular complications (flexion contracture, nerve palsy)
- formation of bedsores.
Also, in a state of catatonic excitement, the patient poses a danger to himself and others. The sudden onset of an attack of stupor can lead to an accident, overtaking a person driving a car, while crossing the road, at work, etc.
Complications of severe forms of catatonia are difficult to treat due to the difficulties in contact between the patient and the doctor.
Questions and answers
Question:
Good day. I am 21 years old. When I start communicating with someone, I feel some kind of stupor, I can’t say anything, I can’t carry on a conversation, there’s some kind of mess in my head. If I want to tell something, I often forget the words and get lost. I’m afraid to stay with a person one-on-one, I think that he will be bored with me. In the company of friends, all I do is listen, although when there is a conversation about something, I understand that I can tell a lot, express my opinion . Sometimes I think that I am inattentive and “dumb”. I myself am interested in psychology, football, technology, but when these topics are discussed, I am still afraid to say something. It feels like a cockroach is sitting in your head and doesn’t allow you to get used to the information and express yourself competently. The problem started back in school, when conflicts with classmates began, then the situation improved a little, but I became a boring person who is often silent, and when he wants to say something, he blurts out some nonsense, but only then do I realize it. Tell me what could be the problem?
Answer: The problem is the fear of other people’s assessment of their statements, actions, and deeds. Fears inhibit communication, and this “inhibition” makes one feel ashamed. Shame is an affective feeling; it practically paralyzes both the thinking and the active processes. Anger at oneself and lack of self-acceptance appear. Perhaps this is roughly what is happening to you. You might want to take individual or group classes to reduce your fears and discover that you are not the only one, many experience similar feelings. Then it will be easier to accept yourself and cope with your fears.
Question:
When the teacher asks something, I can’t say anything, because it’s like there’s some kind of stupor. I speak normally with my friends, no problem. It also happens that in a minibus I have to tell them to stop at the bus stop, but I can’t say a word, or in a store. How to deal with this?
Answer: It seems to me that the fear of speaking appears in you in situations where you do not feel that you are on an equal footing with the interlocutor (as happens with friends: you are on the same level with them). In frightening situations, there is a feeling that you should be evaluated (by the teacher or people on the minibus). Perhaps this fear of being assessed (most likely, a low assessment) is what causes stupor: it’s better not to say anything than to “blurt something stupid” and embarrass yourself. In such cases (if this is your case, of course) you can work with self-esteem, self-acceptance - non-judgmental. Maybe you are too hard on yourself? In addition, there are a lot of tricks that, for example, speakers use when speaking in front of a large audience. The fact is that the fear of public speaking is inherent in a huge number of people. To calm down before going out in public, speakers use different things: breathing (several deep breaths, exhalations, for example), visualization (imagine that you are among friends - just chatting carefree). There are special exercises to help improve diction, including for moments when your throat gets dry. You can combine the practice of such exercises and work to increase self-esteem and self-confidence.
Diagnostics
When diagnosing catatonic states, it is important to correctly assess the patient’s clinical condition. When collecting anamnesis and examination, it often turns out that the person used psychoactive substances, which most likely contributed to the development of catatonic syndrome. It is worth considering the likelihood of developing symptoms of catatonia during treatment with psychotropic drugs for concomitant diseases.
Psychometric scales are used to diagnose the disorder. The most commonly used is the Bush-Francis Catatonic Disorder Scale. It allows you to determine the presence and severity of catatonic symptoms over a certain period of time. Other rating scales are also used.
Electroencephalography (EEG), CT, MRI and neuropsychological examinations allow us to suggest the localization of disorders in the brain and diagnose the functional state of higher mental functions.
Differential diagnosis is carried out with other mental and somatic disorders accompanied by motor disorders. The most clinically similar to the catatonic syndrome is Parkinson's disease, but the disease is accompanied by a number of specific symptoms that make it possible to differentiate it from catatonia (tremor, apraxia of walking).
Catatonia is differentiated from schizophrenic catatonia, acute psychoses with motor agitation, conversion disorders and other conditions with severe motor retardation or agitation, and neurological symptoms.
Forecast
Mild forms of catatonia usually do not have a strong impact on the patient’s further social adaptation and respond well to treatment. Treatment is carried out in a psychiatric hospital. In case of severe somatic diseases, hospitalization is carried out in a specialized department (neurological, oncological). A poor prognosis is associated with catatonia of a malignant course, due to the risk of death, and the presence of catatonia in children, adolescents and the elderly with schizophrenia. Such people require constant psychiatric treatment. Relapses of catatonic states most often occur with the idiopathic version of the disorder or in the presence of concomitant affective disorders. If a person has renal failure, Parkinson's disease, or alcohol addiction, the dysfunction of the brain is chronic, which can also lead to relapses.
In most cases, the prognosis of catatonic syndrome depends on the course of the underlying disease and timely treatment.
Twilight stupefaction
Twilight stupefaction is considered one of the most specific symptoms in medicine in general. It is characterized by complete loss of memory for the period of morning and evening (twilight). The patient's ability to navigate in space is severely impaired, severe hallucinations are possible, which the patient is afraid of, as well as incoherent speech and muttering. Fortunately, this symptom is quite rare and is not accompanied by a complete loss of consciousness (unlike, for example, epilepsy).
A characteristic feature of mental confusion in somatic diseases is that some of the memories are erased. The darknesses themselves are short-lived and proceed dynamically, often moving from one to another and to a normal state.
Treatment in Re-Alt
When treating catatonia that has developed against the background of another mental or physical disorder, therapy is aimed mainly at the underlying disease. Therefore, it is very important for the effectiveness of treatment to conduct a thorough diagnosis. At the Re-Alt mental health center, specialists conduct a detailed analysis of each clinical case and assess the patient’s mental and somatic status in order to individually select treatment tactics.
The most effective method of treating catatonia is the use of drugs from the group of benzodiazepine tranquilizers. Pharmacotherapy helps reduce muscle tone and eliminate other manifestations of catatonia. Treatment uses drugs with sedative, anticonvulsant effects, and muscle relaxants.
If drug treatment is ineffective, electroconvulsive therapy may be prescribed.
Febrile catatonia is a medical emergency. Treatment is carried out inpatiently. Measures are prescribed to maintain and normalize the functioning of all body systems. Antibacterial therapy is prescribed to prevent complications. After stabilization of the condition, electroconvulsive therapy is performed