People who have suffered a stroke have the possibility of full or partial recovery. Experts insist on carrying out rehabilitation measures for three years.
As a rule, ischemic stroke gives more hope, since it is characterized by less dangerous damage to the cells of the cerebral cortex and the use of “spare” vessels for nutrition. In the hemorrhagic form, physical rehabilitation is limited to preventing recurrent circulatory disorders, timing of hematoma resorption, and the use of surgical intervention.
Gymnastics after a stroke is part of planned rehabilitation measures along with medications, physiotherapy, diet, and regimen.
What problems does exercise therapy solve after a stroke?
Exercise therapy for stroke plays an important role in the prevention of complications, the development of a person’s adaptation to self-care, and the acquisition of lost functions.
A long period of forced immobility in bed is dangerous for the development of severe consequences. The exercise therapy complex helps prevent:
- formation of bedsores on the buttocks, back;
- congestive pneumonia;
- the occurrence of heart failure;
- progressive atrophy of non-working muscles;
- formation of blood clots followed by embolism in vital organs;
- spasm of muscle groups with increased tone during paresis and spastic paralysis, formation of contractures (change in limb shape).
Gymnastics after a stroke has a positive effect on microcirculation and metabolism in organs and tissues that are reduced as a result of the disease. It allows you to resume active movements and, in the long term, helps you gain the ability to draw, write, and use dishes and household appliances. Leads to normalization of the functioning of internal organs (urination, defecation), helps restore speech.
Drug therapy
If the right side is paralyzed due to a stroke, you should start with drug therapy. The drugs of choice are:
- Antiplatelet agents and anticoagulants (Curantil, Warfarin) - thin the blood and improve its passage through the arteries. The use of these drugs is effective for atherosclerosis, thrombosis or vascular spasms;
- Diuretics (Hypothiazide, Veroshpiron) – remove excess fluid, prevent cerebral edema and hypertensive crisis;
- Antispasmodics (Papaverine, Vincamine) - relax blood vessels and improve blood circulation;
- Agnioprotectors (Parmidin, Alprostan) – have a beneficial effect on the arteries, preventing the development of spasms;
- Nootropics (Piracetam, Actovegin) - improve brain function. They are taken for a long time, including the rehabilitation period.
The doctor prescribes medications based on the patient’s condition. In severe cases, a complete list is written out, and daily blood pressure monitoring is carried out.
When can you start exercising?
Beginning to use physical activity, its volume. The target orientation is determined by the attending physician. It depends on the:
- the extent of damage to brain tissue;
- sufficient ability of the body to recover;
- timeliness and completeness of treatment.
The first 6 months are considered the acute period. At this time, changes occur in the ischemic focus: some cells die irrevocably, while others retain the ability to perform their functions, but need help. This is exactly what exercises after a stroke are designed to do. At the cellular level, there is a special memory that should “remember” the range of movements and restore the transmission pathways of nerve impulses.
If the patient is not in a coma and consciousness is preserved, then on the third day he is recommended to begin breathing exercises. Its goal is to prevent congestion in the lungs. From the fifth day, physical therapy (PT) is prescribed. The sets of exercises include familiar movements, taking into account the patient’s condition, the ability to sit or stand independently, and the degree of loss of motor functions.
It is recommended to continue physical education after discharge at home. To do this, loved ones should learn the necessary exercises themselves, support and encourage the patient’s aspirations. Positive emotions and good mood play a significant role in the speed of rehabilitation.
In the later period (after six months or more), the patient needs to use a rehabilitation course of treatment in specialized centers and sanatoriums. It is recommended to repeat therapy 2 times a year. Here, in addition to the physical education rehabilitation complex, there are opportunities for extended physiotherapeutic treatment under the supervision of medical personnel:
- oxygen baths;
- massage;
- acupuncture;
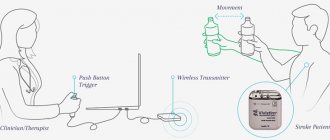
- hardware electrical stimulation of paralyzed muscle groups;
- pulsed magnetic therapy;
- electrosleep.
Neurostimulation of the leg muscles is performed
What to do at home?
If the recovery process is not started in a timely manner, the patient experiences complete or partial paralysis, disturbances in the functioning of the speech apparatus, loss of memory, hearing and decreased vision. The most severe consequences of a stroke are coma and swelling of the brain.
Before restoring the right or left side after a stroke, the victim’s relatives and friends must ensure:
- Comfort. The rehabilitation process at home requires a positive atmosphere and a comfortable environment. Relatives should create a well-ventilated and lit room. You should also install a bed with a special mattress, which will reduce the likelihood of bedsores. The pillow should provide good support for the head, made of loose material.
- Nutrition. Cooked food should be moderately warm and tasty. It is recommended to divide food into 4-5 meals, the last of which is served no later than 2 hours before bedtime. Dishes are prepared without the use of salt, baked or boiled. To clarify dietary standards, you should consult your doctor.
- Hygiene. The main problem slowing down the rehabilitation process is bedsores, which appear due to pressure from hard chairs, beds, or improper turns and movements. To avoid this, carry out timely body hygiene and care for the patient every day. The victim's skin should be kept clean, without excessive moisture or dryness.
You should also arrange household items in such a way that a person who has had a stroke can reach them without lifting their torso on their toes. It is recommended to cover the table with a slightly damp towel to prevent the dishes from slipping. The handles of utensils such as razors, combs, spoons, etc. should be covered with foam padding.
How to do breathing exercises?
While lying down, the patient simply needs to take a few deep breaths, repeat throughout the day as often as possible. When the doctor allows you to sit, it is important not to bend your back, but to keep it straight so that the air can straighten your lungs as much as possible.
Breathing exercises involve taking a slow, deep breath, holding your breath for a few seconds, and then gradually exhaling. After each such breath, the patient needs rest. You need to make sure that dizziness does not increase, and do not strain while holding your breath.
There are options for controlling long exhalation:
- inflating a rubber ball;
- using a cocktail straw dipped into a cup of water.
The patient feels the result of his work by the volume of the ball and the gurgling of the liquid. In the future, you can begin to master a course of exercises using Strelnikova’s method.
What exercises can you do lying down?
If the patient is not allowed to sit and stand up or cannot do this, the exercises are carried out first in a passive mode, then in an active mode.
Passive physical education means the absence of participation of the patient, the use of the efforts of another person
Exercises are limited to movements in the joints of the arms and legs. The complex gradually includes passive flexion, extension, rotation, abduction and adduction with increasing amplitude. You should not immediately try to fully complete the maximum option. Start with small vibrations up to 15 movements in each joint 3-4 times a day.
It is recommended not to forget about the sequence of joint development: from the center to the periphery. In other words, exercises for the arm begin with the shoulder, then move on to the elbow joint, wrist and hand. Similarly on the legs: from the femur to the small joints of the foot.
Passive exercises in the hand with monoparesis can be performed by the patient himself with the help of a healthy hand. As a device for self-study, a loop made of fabric or wide rubber is used, into which the patient threads a stationary limb and performs movements, clinging to it.
The patient performs active exercises independently. Special complexes have been developed for this purpose. They begin lying down and continue in a sitting position.
Experts insist on carrying out rehabilitation measures for three years after a stroke. As a rule, ischemic stroke gives more hope, since it is characterized by less dangerous damage to the cells of the cerebral cortex and the use of “spare” vessels for nutrition. In the hemorrhagic form, physical rehabilitation is limited to preventing recurrent circulatory disorders, timing of hematoma resorption, and the use of surgical intervention. Gymnastics after a stroke is part of planned rehabilitation measures along with medications, physiotherapy, diet, and regimen.
What problems does exercise therapy solve after a stroke?
Exercise therapy for stroke plays an important role in the prevention of complications, the development of a person’s adaptation to self-care, and the acquisition of lost functions. A long period of forced immobility in bed is dangerous for the development of severe consequences. The exercise therapy complex helps prevent:
- formation of bedsores on the buttocks, back;
- congestive pneumonia;
- the occurrence of heart failure;
- progressive atrophy of non-working muscles;
- formation of blood clots followed by embolism in vital organs;
- spasm of muscle groups with increased tone during paresis and spastic paralysis, formation of contractures (change in limb shape).
Gymnastics after a stroke has a positive effect on microcirculation and metabolism in organs and tissues that are reduced as a result of the disease. It allows you to resume active movements and, in the long term, helps you gain the ability to draw, write, and use dishes and household appliances. Leads to normalization of the functioning of internal organs (urination, defecation), helps restore speech.
When can you start exercising?
The beginning of the use of physical activity, its volume, and target orientation are determined by the attending physician depending on:
- the extent of damage to brain tissue;
- sufficient ability of the body to recover;
- timeliness and completeness of treatment.
The first 6 months are considered the acute period. At this time, changes occur in the ischemic focus: some cells die irrevocably, while others retain the ability to perform their functions, but need help. This is exactly what exercises after a stroke are designed to do. At the cellular level, there is a special memory that should “remember” the range of movements and restore the transmission pathways of nerve impulses. If the patient is not in a coma and consciousness is preserved, then on the third day he is recommended to begin breathing exercises. Its goal is to prevent congestion in the lungs. From the fifth day, physical therapy (PT) is prescribed. The sets of exercises include familiar movements, taking into account the patient’s condition, the ability to sit or stand independently, and the degree of loss of motor functions. It is recommended to continue physical education after discharge at home. To do this, loved ones should learn the necessary exercises themselves, support and encourage the patient’s aspirations. Positive emotions and good mood play a significant role in the speed of rehabilitation. In the later period (after six months or more), the patient needs to use a rehabilitation course of treatment in specialized centers and sanatoriums. It is recommended to repeat therapy 2 times a year
How to do breathing exercises?
While lying down, the patient simply needs to take a few deep breaths, repeat throughout the day as often as possible. When the doctor allows you to sit, it is important not to bend your back, but to keep it straight so that the air can straighten your lungs as much as possible. Breathing exercises involve taking a slow, deep breath, holding your breath for a few seconds, and then gradually exhaling. After each such breath, the patient needs rest. You need to make sure that dizziness does not increase, and do not strain while holding your breath.
There are options for controlling long exhalation:
- inflating a rubber ball;
- using a cocktail straw dipped into a cup of water.
This is important at any stage of rehabilitation
Proper physical rehabilitation is impossible without targeted support for mental activity. Muscle memory allows even weakened cortical structures to issue commands. The patient is recommended to accompany all exercises with mental “orders” for his legs and arms to move. This modern approach to recovery allows the patient to become a full participant in the recovery process.
What exercises can you do lying down?
If the patient is not allowed to sit and stand up or cannot do this, the exercises are carried out first in a passive mode, then in an active mode. Passive physical education means the absence of the patient’s participation, using the efforts of another person.
Exercises are limited to movements in the joints of the arms and legs. The complex gradually includes passive flexion, extension, rotation, abduction and adduction with increasing amplitude. You should not immediately try to fully complete the maximum option. Start with small vibrations up to 15 movements in each joint 3-4 times a day. It is recommended not to forget about the sequence of joint development: from the center to the periphery. In other words, exercises for the arm begin with the shoulder, then move on to the elbow joint, wrist and hand. Similarly on the legs: from the femur to the small joints of the foot.
Passive exercises in the hand with monoparesis can be performed by the patient himself with the help of a healthy hand. As a device for self-study, a loop made of fabric or wide rubber is used, into which the patient threads a stationary limb and performs movements, clinging to it. The patient performs active exercises independently. Special complexes have been developed for this purpose. They begin lying down and continue in a sitting position.
A set of active movements for the hands
You can make independent movements with your hands up to 20 times in one approach:
- clench and unclench your fingers into a fist;
- circles in both directions in the wrist joint (it is recommended to keep your fist clenched);
- flexion and extension at the elbows;
- from a position along the body, slowly rise and fall, while loading the shoulder joints;
- swing to the sides.
Exercises with dumbbells use the flexor muscles and hold by clenching the hand into a fist.
After a stroke, a person loses the ability to make small movements with his fingers. And this is very necessary in restoring self-service. To develop hand motor skills it is recommended:
- Place small items (nuts, buttons, spools of thread, pencils) in a large bowl;
- the patient should transfer them with the affected hand from one bowl to another.
In sanatoriums, games of mosaic, lotto, and collecting pyramids are used.
A set of active exercises for legs
For the legs, exercises can also be started with a period of strict bed rest and continued while sitting. The number of repetitions should not tire the patient and increase gradually to 20.
- The toes actively perform flexion and extension.
- Pull your socks towards you, then move them to the opposite extreme position (it is recommended to mentally imagine the pressure on the pedals).
- Slow knee flexion, extension.
- Abduction to the side due to the work of the hip joint.
How to develop the muscles of the torso?
Lying on your back, you can perform the following exercises 5-10 times:
- turns to the sides by rolling from one side to the other;
- with emphasis on the shoulder blades, back of the head, feet, using the elbows, lift the pelvis;
- try to slightly raise your upper body by tensing your abdominal muscles.
- An important means of restoring and improving the motor activity of patients after a stroke is hydrokinesitherapy. The aquatic environment in which classes are conducted has a general tonic effect on the body, increases muscle elasticity and joint flexibility, and improves tissue trophism. Physical exercises performed in water have a relaxing effect on spasmed muscles, restore the smoothness of movements and their coordination. The recommended water temperature in the pool for patients with stroke consequences is 29-35°C; Duration of classes – 30 minutes.
What other movements need to be developed?
Physical education after a stroke, in addition to the limbs, requires the development of facial muscles, especially the eyes. To prevent drooping of the eyelid, the following exercises are recommended 5-7 times:
- eye movements up and down and to the sides;
- describe a circle with your eyes in one direction, then in the other;
- blink and squeeze for a few seconds.
To strengthen your neck muscles you need to:
- make slow turns of the head to the sides;
- rest your head on the pillow, then relax.
Exercises while standing
For a patient who is able to stand and move slowly, the number of exercises should be increased and varied. However, there is no need to rush. You need to start with a simple complex, and then move on to a more complex one with increasing load. The following exercises are considered simple:
- stretching with a description of circular movements with the hands and mandatory control of breathing (when moving up, take a deep breath, down, exhale completely);
- alternately rolling from toes to heels with tension in the calf muscles;
- turns to the sides (5-6 times each);
- squats without lifting your heels off the floor 4–5 times;
- bending to the sides while raising the opposite arm above your head 4 times;
- swing your legs forward and to the sides, 4 each;
- alternate lunges forward with a slight shift of weight to the front leg.
Added to the complex with increased load:
- stretching with hands clasped in a “lock”;
- swinging your legs while holding your hand on a stationary headboard of a bed or chair;
- bend forward and to the sides 10 times, standing on tense legs in a position slightly wider than shoulder width;
- “boxing” with your hands while turning your body;
- circular rotations in the shoulder joints forward and backward;
- arbitrary jumps.
The exercises should be completed by walking in place and deep breathing movements for 5 minutes.
Contraindications
Limitations in rehabilitation depend on the patient's condition. Physical activity is not indicated in the following cases:
- the patient did not recover from the coma;
- mental changes in behavior and aggressiveness are observed;
- repeated stroke in an elderly person;
- there are symptoms of epileptiform seizures, cramps in the limbs;
- Stroke is accompanied by severe diabetes mellitus, tuberculosis, and cancer.
An important point in physical therapy is the patient’s comfortable state of health. The appearance of headaches and weakness requires control of blood pressure, rest, and a slower rate of increase in load. After gaining the opportunity to walk, it is necessary to use walks in the air with a gradual lengthening of the route. Confidence in one’s abilities and the support of loved ones allows the patient to take stroke therapy as beneficially as possible and strive for a full recovery.
A set of active movements for the hands
You can make independent movements with your hands up to 20 times in one approach:
- clench and unclench your fingers into a fist;
- circles in both directions in the wrist joint (it is recommended to keep your fist clenched);
- flexion and extension at the elbows;
- from a position along the body, slowly rise and fall, while loading the shoulder joints;
- swing to the sides.
Exercises with dumbbells use flexor muscles and hold by clenching the hand into a fist.
A set of active exercises for legs
For the legs, exercises can also be started with a period of strict bed rest and continued while sitting. The number of repetitions should not tire the patient and increase gradually to 20.
- The toes actively perform flexion and extension.
- Pull your socks towards you, then move them to the opposite extreme position (it is recommended to mentally imagine the pressure on the pedals).
- Slow knee flexion, extension.
- Abduction to the side due to the work of the hip joint.
What other movements need to be developed?
Physical education after a stroke, in addition to the limbs, requires the development of facial muscles, especially the eyes. To prevent drooping of the eyelid, the following exercises are recommended 5-7 times:
- eye movements up and down and to the sides;
- describe a circle with your eyes in one direction, then in the other;
- blink and squeeze for a few seconds.
To strengthen your neck muscles you need to:
- make slow turns of the head to the sides;
- rest your head on the pillow, then relax.
After a stroke, a person loses the ability to make small movements with his fingers. And this is very necessary in restoring self-service. To develop hand motor skills it is recommended:
- Place small items (nuts, buttons, spools of thread, pencils) in a large bowl;
- the patient should transfer them with the affected hand from one bowl to another.
In sanatoriums, games of mosaic, lotto, and collecting pyramids are used.
Diet
Diet is necessary to improve blood circulation and maintain immune resistance. A well-chosen table should contain everything necessary for the regeneration of damaged tissues, but not overload the weakened body.
The basic rules for the diet are as follows:
- exclusion of smoked and fatty foods;
- meat can only be eaten with the approval of a doctor, in small portions and pureed. The menu includes only lean varieties;
- enrich your diet with vegetables and fruits;
- exclude coffee, strong tea, soda and alcohol;
- food should be fractional, in small portions.
For seriously ill patients, the menu is prepared by a nutritionist, taking into account the state of the body and the necessary energy costs.
Exercises while standing
For a patient who is able to stand and move slowly, the number of exercises should be increased and varied. However, there is no need to rush. You need to start with a simple complex, and then move on to a more complex one with increasing load.
The following exercises are considered simple:
- stretching with a description of circular movements with the hands and mandatory control of breathing (when moving up, take a deep breath, down, exhale completely);
- alternately rolling from toes to heels with tension in the calf muscles;
- turns to the sides (5-6 times each);
- squats without lifting your heels off the floor 4–5 times;
- bending to the sides while raising the opposite arm above your head 4 times;
- swing your legs forward and to the sides, 4 each;
- alternate lunges forward with a slight shift of weight to the front leg.
Half-lunge with clasped hands is used to increase the load
Added to the complex with increased load:
- stretching with hands clasped in a “lock”;
- swinging your legs while holding your hand on a stationary headboard of a bed or chair;
- bend forward and to the sides 10 times, standing on tense legs in a position slightly wider than shoulder width;
- “boxing” with your hands while turning your body;
- circular rotations in the shoulder joints forward and backward;
- arbitrary jumps.
The exercises should be completed by walking in place and deep breathing movements for 5 minutes.
Contraindications
Limitations in rehabilitation depend on the patient's condition. Physical activity is not indicated in the following cases:
- the patient did not recover from the coma;
- mental changes in behavior and aggressiveness are observed;
- repeated stroke in an elderly person;
- there are symptoms of epileptiform seizures, cramps in the limbs;
- Stroke is accompanied by severe diabetes mellitus, tuberculosis, and cancer.
An important point in physical therapy is the patient’s comfortable state of health. The appearance of headaches and weakness requires control of blood pressure, rest, and a slower rate of increase in load.
After gaining the opportunity to walk, it is necessary to use walks in the air with a gradual lengthening of the route. Confidence in one’s abilities and the support of loved ones allows the patient to take stroke therapy as beneficially as possible and strive for a full recovery.
Visit to a speech therapist
To restore speech, daily training is required, which will be supervised by a specialist. The patient is given homework, including systematic exercises.
The objectives of such therapy are:
- restoration of oral speech;
- rehabilitation of writing;
- normalization of speech memory.
It is very important that a person not only learns to speak, but also understands the speech of others. Experts recommend that patients not isolate themselves, but constantly contact people.