Psychomotor agitation: symptoms and emergency care
- Psychotherapist of the highest category Oleg Viktorovich
- 41295
- Update date: October 2019
Psychomotor agitation is characterized by increased motor and mental activity.
The severity of such symptoms can vary and depends on the degree of development of the pathological process. The main manifestations of the syndrome include anger, anxiety, excessive fun or aggression and other behavior that is classified in modern society as inadequate.
In some patients, the pathology causes confusion and lethargy.
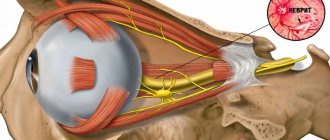
Symptoms of nervous excitement are disturbances in the movements of the eyeballs, asymmetry of the facial muscles, poor orientation in time and space, awkwardness and lack of composure. In addition, headaches and a slight delay in intellectual development are noted. Insomnia is a hallmark of increased nervous excitability.
Insomnia is determined by a person’s condition if he cannot fall asleep for three to four hours, he tosses around in bed, trying to find a comfortable body position. A person may also wake up in the middle of the night and lie there until the morning with his eyes open. In some cases, insomnia is considered as a symptom of some somatic pathology.
Agitation has clear symptoms, but the patient himself usually does not notice them. The first thing that may appear in a person is speech anxiety.
Speaking quickly and indistinctly, he has difficulty formulating his thoughts. Added to this phenomenon is trembling of the fingers or sudden movements of the entire hand. At the same time, there is an increase in heart rate and breathing. The patient is sweating heavily and is in undisguised emotional excitement.
If the disease has passed the initial stage, the patient will complain of a feeling of devastation and difficulty concentrating. The disease does not allow us to draw up cause-and-effect relationships and think logically. In this case, fear, panic and fussiness arise.
A person has difficulty expressing thoughts, and cannot write at all due to trembling hands. He can perform only the simplest actions and requests, but as the disease worsens, his activity will be reduced to sleep and meals.
Diagnosis and treatment should be carried out by a psychiatrist. In addition, you will need to consult a neurologist and, possibly, a narcologist. Currently, there are accurate and rapid methods for diagnosing mental disorders. In order to determine the diagnosis and correctly plan the treatment, the specialist will need to collect an anamnesis, namely:
- visual inspection;
- monitoring pulse and blood pressure;
- general blood, urine and biochemical analysis;
- hormone analysis;
- MRI of the brain.
This will allow the doctor to determine the severity of the disease and state that it is agitation and not, for example, akathisia. similar in symptoms. Based on the information collected, a treatment plan will be developed and specific medications will be selected. The specialist will also decide whether the patient needs hospitalization.
Psychomotor agitation is a dangerous health condition in humans. It can occur in both adults and children. The pathology is episodic in nature, and the factors that provoke its occurrence are different. In general terms, psychomotor agitation can be described as a state in which a person performs many actions, sometimes illogical and dangerous to life and the people around him. Let's look at this syndrome in more detail.
Depending on the clinical picture, there are many types of psychomotor agitation:
- Dysphoric: characterized by the patient’s tension, gloominess, gloominess, irritability, distrust, suicide attempts, unexpected aggression. Most often occurs with organic brain lesions and epilepsy;
- Anxious: manifested by simple movements (for example, swaying of the body) and is often accompanied by the repetition of some words or phrases, groans. Sometimes it suddenly gives way to frantic excitement (raptus), in which a person begins to rush around, scream, and hit surrounding objects. It is observed, as a rule, in depressive syndromes;
- Manic: characterized by an increased desire for any activity, high spirits, accelerated flow of thoughts;
- Catatonic: manifested by impulsive, mannered, uncoordinated, pretentious, sometimes monotonous rhythmic movements and conversations;
- Hebephrenic: this psychomotor agitation is of a foolish nature, often accompanied by meaningless impulsive actions with aggression, hallucinations, delusions, and mental automatism. Mainly observed in schizophrenia;
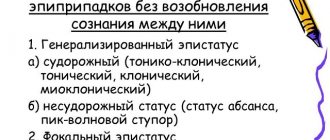
- Epileptiform: is a form of epileptic twilight state and is manifested by sudden onset motor agitation, which is accompanied by aggressiveness, fear, hallucinations, desire to escape, disorientation in the situation and in time;
- Psychosomatic: occurs against the background of psychopathy and other sluggish diseases (for example, with organic damage to the central nervous system, schizophrenia). The patient begins to scream, swear, threaten and show aggression towards the person with whom he has a conflict. May be dangerous to others;
- Hallucinatory and delusional: expressed by impetuous movements, intense concentration, incoherent phrases, changeable facial expressions, aggressive gestures, tension of the patient who angrily shouts threats, can insult and even hit. These types of psychomotor agitation are found in hallucinatory-delusional and delusional syndromes, sometimes with delirium. Under the influence of hallucinations or delusions, people commit unmotivated attacks (often unexpectedly) and suicidal acts;
- Psychogenic: characterized by a narrowed consciousness, insane fear, panic mood, senseless thrashing. Observed during psychogenic reactions;
- Eretic: manifested by senseless destructive actions accompanied by screams. Occurs in patients with oligophrenia.
Forecast
Mild forms of catatonia usually do not have a strong impact on the patient’s further social adaptation and respond well to treatment. Treatment is carried out in a psychiatric hospital. In case of severe somatic diseases, hospitalization is carried out in a specialized department (neurological, oncological). A poor prognosis is associated with catatonia of a malignant course, due to the risk of death, and the presence of catatonia in children, adolescents and the elderly with schizophrenia. Such people require constant psychiatric treatment. Relapses of catatonic states most often occur with the idiopathic version of the disorder or in the presence of concomitant affective disorders. If a person has renal failure, Parkinson's disease, or alcohol addiction, the dysfunction of the brain is chronic, which can also lead to relapses.
In most cases, the prognosis of catatonic syndrome depends on the course of the underlying disease and timely treatment.
Classification
Types of psychomotor agitation:
- Dysphoric. Increased aggressiveness against a background of gloomy mood. Often a consequence of organic brain damage or epilepsy;
- Alarming. The patient is restless, cannot sit quietly - he sways his body, bites his nails, and often repeats fragments of phrases or words. This may be followed by raptus, a sudden agitation in which the person begins to scream and rush around the room. It is a consequence of depressive syndrome;
- Manic. Increased desire to perform any activity, high productivity, good mood and accelerated flow of thoughts. Often - during the manic phase of bipolar disorder;
- Catatonic. Against the background of complete immobilization and waxy flexibility (freezing in a certain position for up to several hours or even days), impulsive behavior begins, during which a person can injure himself and others. Characteristic of catatanonic schizophrenia;
- Hebephrenic. Senselessness of actions, aggressiveness, bizarre judgments, hallucinations and delusions indicate the onset of schizophrenia;
- Epileptiform. A sharp onset of excitement, which is accompanied by fear, hallucinations and aggressiveness;
- Psychosomatic. In many ways similar to the hebephrenic form, it occurs both in schizophrenia and organic brain lesions;
- Hallucinatory and delusional. Against the background of a clouding of consciousness, a person becomes “driven” by his hallucinations, his mood changes extremely quickly, there is anger and the risk of committing an illegal act;
- Psychogenic. There is a fear of death, an anxious mood, and rushing around the room. Easily confused with an anxious form of arousal. Occurs in healthy individuals in difficult life situations;
- Eretic. Senseless exclamations and destructive actions towards surrounding people and objects are a consequence of mental retardation.
Suicidal behavior
Suicidal tendencies are an almost obligatory component of severe depressive states (see section 8.3.1). Patients without severe inhibition (anxious or agitated depression) commit suicide especially easily. A history of suicide attempts is a very alarming sign, since in most cases such attempts are repeated. A patient with depression should be monitored throughout the entire period while he is in a sad mood, and supervision should be especially careful in the morning, when depression is most severe. It should be taken into account that men are 3 times more likely to commit suicide than women, although women attempt suicide 4 times more than men. The greatest number of attempts are made by people aged 15 to 40 years, but older people are more likely to complete suicide than young people. Factors correlating with suicide risk are presented in Table. 25.1.
Table 25.1. Factors correlated with suicide risk (but G.I. Kaplan and B.J. Sadok, 1994)
Age 45 years and older Alcoholism
Excitability, aggressiveness, tendency to violence Suicidal behavior in the past Male gender
Reluctance to accept help History of prolonged depressive episode Hospitalization and treatment in a psychiatric hospital Depression
Physical illness, upcoming surgery Loss of a job or retirement Loneliness, loss of a partner, divorced Suicides among close relatives
If suspicion arises, the doctor should directly ask the patient about the presence of suicidal thoughts: most patients do not hide them. If a person who has previously admitted to wanting to commit suicide avoids communication and seems to be hiding, this should alert the doctor. If the patient has developed a specific plan for suicidal action, supervision should be the most stringent. Patients are prescribed antidepressants, but they do not have a quick effect on depressive symptoms. Therefore, in the first days of treatment (especially with agitated depression), antipsychotics or tranquilizers (25-75 mg tizercin, 15-30 mg relanium, 30-75 mg sonapax per day) are additionally prescribed. Sometimes lithium salts are prescribed.
In schizophrenia, suicidal behavior can be caused by imperative hallucinations and hypochondriacal delusions. However, unexpected suicide attempts often occur against the background of mild schizophrenic personality changes, when patients seem to be conducting an “experiment” (“It was interesting to see what would happen...”); it can be difficult to foresee such a suicide.
With hysteria and hysterical psychopathy, demonstrative suicide attempts are often observed, when patients, against the background of a conflict situation, declare that they will commit suicide, without actually having the desire to die. Such behavior should not be ignored, since in a temper, patients can take dangerous steps and do not take into account the possible consequences. Decisive actions are required to prevent rash actions by patients. Hospitalization is advisable.
You should always be extremely wary of any statements from patients regarding their reluctance to live or desire to die. The doctor should not be reassured by the patient’s smile that accompanies these words and the apparent criticism. By telling the doctor about his thoughts, the patient, of course, wants the doctor to prevent suicide, and if he does not receive reciprocal attention, then this can become another impetus for suicide.
Treatment of psychomotor agitation
The most important way to deal with nervous agitation or causeless anxiety is to find and treat the cause. Without treatment, this nervous agitation leads to an increased risk of suicide. The following measures will help reduce anxiety:
- Calm environment
- Sufficient lighting
- Medicines such as benzodiazepines and, in some cases, antipsychotics
- Full, quality sleep
- Exercise stress
- A change in familiarity or surroundings, such as a short vacation
- Hobbies and interests
Don't focus too much on your anxiety if possible. This usually makes the problem worse. If your loved one is at risk of harming themselves or others due to nervousness or anxiety, and there are no other less restrictive ways to control their behavior, use only firm boundaries.
It is important for the doctor to discover the cause of the appearance of hydration, and, based on this, then draw up a treatment regimen; usually treatment consists of several methods:
- taking medications to relieve symptoms;
- psychotherapy for social adaptation;
- getting rid of alcoholism (if required);
- physical therapy;
- diet correction.
Properly selected medications play a leading role. The course will include several drug groups:
- Adsorbents (Polyphepan, Baktistatin) and absorbents (activated carbon, Polysorb). If the agitation was caused by alcoholism, then first the patient will need to be brought out of this state, to “cleanse” his body of toxins and their breakdown products.
- Antipsychotics (Solean, Zeldox). Relieves paranoid attacks and obsessive thoughts and ideas. Their reception is carried out exclusively within the walls of the hospital, under the supervision of medical staff. Take the course for up to 14 days.
- Sedative antidepressants (Lyudiomil, Fluoxetine). “Softer” drugs for depression and nervous agitation. Course – 14 days.
- Tranquilizers (Phenazepam, Diphenhydramine, Lexotan). Required to stabilize the condition, to remove a person from a state of binge drinking. Use for no more than 5-7 days, as they can be addictive.
- Antianxiolytic drugs are prescribed with extreme caution.
A psychiatrist and narcologist regularly works with the patient, offering certain methods of behavior for optimal recovery from depression. The main thing is for the patient to learn to control their emotions and “work around” stressful situations. Psychotherapy will increase stress resistance and allow you to independently deal with emotional oppression.
To prevent the development of agitation, it is recommended to follow a diet and not abuse alcohol. If you often experience stress or simply have a difficult life situation, you should not neglect a visit to a psychoanalyst.
Clinical picture
Symptoms of psychomotor agitation depend on its type, but the main manifestations are excessive physical and mental activity. Do not forget that such a reaction can be natural if a person is in a stressful situation for him - this is how the body adapts to the current circumstances.
The severity of clinical manifestations varies from mild to severe. With a mild degree, erased or weak symptoms are observed, mood swings are possible, but behavior remains within normal limits. The average degree is characterized by pronounced emotional disharmony, the mood has only two extremes - excellent and disgusting, which has a great influence on human behavior.
Pathogenesis
There is no consensus on the pathogenesis of catatonia. Studies have shown that disruption of communication between cortical structures, the thalamus and the basal ganglia play an important role in the occurrence of catatonic symptoms, therefore, in addition to clinical assessment, when studying catatonia, it is worth taking into account the results of neuroimaging and neuropsychological examinations. The hypothesis is based on a lack of gamma-aminobutyric acid (GABA) in the basal ganglia. Normally, GABA reduces the intensity of emotional reactions, such as anger, fear or anxiety.
In modern literature, there are often cases of catatonia caused by abrupt withdrawal of drugs used to treat catatonic states and accompanying mental disorders. This therapy uses mechanisms to increase GABA activity in the basal ganglia, which has a positive therapeutic effect. With abrupt withdrawal of drugs, an increase in motor symptoms often occurs (the phenomenon of “rebound catatonia”).
It is possible that catatonia develops as a result of severe anxiety, in response to stress. Therefore, scientists suggest that catatonic states are directly related to affective and other mental disorders that are accompanied by symptoms of severe anxiety.
Questions and answers on the topic “Nervous excitement”
Question: For several months now I have had constant increased nervous excitability. I get nervous with or without reason, and now I’m already nervous from the very fear of starting to get nervous. On the EEG: moderately pronounced general changes in bioelectrical activity. Signs of irritation of brain stem structures. How likely can we talk about organic brain damage here?
Answer: Carrying out an instrumental examination without indications and an overdiagnostic coven in the description of examination data is the path to the somatization of mental disorders and the neuroticization of the nation. General rule: EEG is needed to diagnose epilepsy. Exceptions to this rule are extremely rare. An example of an exception is suspected brain death.
Psychomotor agitation in children
Psychomotor disorders in children are not as common as in adults. Therefore, any deviations in behavior are noticeable almost immediately. Most often, increased motor and mental excitability is a consequence of organic brain damage, birth trauma, or a previous neuroinfection.
In many ways, the pathology is similar to that in adults: fluctuations in mood and thoughts, constant fussiness and increased physical activity, in some cases – delusions and hallucinations. Apathy, social phobia and reluctance to communicate with peers in adolescence should alert parents, as this may serve as the onset of schizophrenia.
The presence of psychomotor agitation can be suspected by inadequacy of judgment and emotional component. Children with mental disorders react too sharply to events happening around them and show emotions that are radically different from the norm (laughter at a funeral, feelings of sadness and melancholy for no apparent reason).
Diagnostics
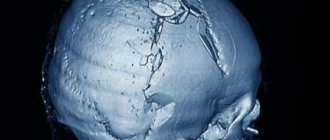
When diagnosing catatonic states, it is important to correctly assess the patient’s clinical condition. When collecting anamnesis and examination, it often turns out that the person used psychoactive substances, which most likely contributed to the development of catatonic syndrome. It is worth considering the likelihood of developing symptoms of catatonia during treatment with psychotropic drugs for concomitant diseases.
Psychometric scales are used to diagnose the disorder. The most commonly used is the Bush-Francis Catatonic Disorder Scale. It allows you to determine the presence and severity of catatonic symptoms over a certain period of time. Other rating scales are also used.
Electroencephalography (EEG), CT, MRI and neuropsychological examinations allow us to suggest the localization of disorders in the brain and diagnose the functional state of higher mental functions.
Differential diagnosis is carried out with other mental and somatic disorders accompanied by motor disorders. The most clinically similar to the catatonic syndrome is Parkinson's disease, but the disease is accompanied by a number of specific symptoms that make it possible to differentiate it from catatonia (tremor, apraxia of walking).
Catatonia is differentiated from schizophrenic catatonia, acute psychoses with motor agitation, conversion disorders and other conditions with severe motor retardation or agitation, and neurological symptoms.
Nervous overexcitement
Increased nervous excitement, as a rule, indicates a weakening of inhibitory nervous processes. According to the law of similarity, which forms the basis of homeopathic treatment, the potentized homeopathic preparation of caffeine Coffea cruda may be useful for an excited patient if the excitement is such that the limbs tremble, the person cannot cope with the influx of thoughts, nervous heartbeat and even a joyful mood, and sleep does not occur.
When the mental excitement is expressed by talkativeness, and the patient (usually a woman) appears lively and cheerful, but in reality it is a morbid condition, Lachesis and Cimicifuga are indicated.
Palladium and Sepia women are excited in company, but almost decompensated at home.
Excessive antasia - Belladonna, Cannabis indica, Hyosciamus, achesis. Stramonium.
A good remedy for painful excitation is potentized Camphor. Rhus has an unbalanced mood (internal restlessness, need for constant movement, as in the case of Chamomilla).
The drugs of choice for mental overexcitation are Aconitum, Anacardium, Argentum nitricum, Aurum, Causticum, Kalium bromatum, Opium, Moschus.
In severe cases of neurosis, obsessive ideas and sensations are formed (fear of space, animals, transport, public and performances, fear of illness, fear of imminent death).
With neurosis, in contrast to delirium, a critical attitude towards one’s condition is usually retained, and obsessive drives (for example, the desire to jump from a height) are usually not realized.
The leading remedy for a patient with truly obsessive ideas is Thuja: sometimes the patient believes that animals are moving in the stomach, sometimes the limbs are made of glass and will break. The patient constantly thinks about this and cannot get rid of these ideas, despite their absurdity.
The Argentum nitricum patient has an obsession with tall buildings falling on him in the street. If the patient feels as if his body and mind are separate, Anacardium or Tuja may help. An additional symptom for Anacardium is an obsessive feeling that the mind is being controlled by some superpower.
The Aurum metallicum patient is gloomy, constantly thinks about death and the extinction of life, and is depressed by a feeling of complete insignificance. Obsessions of a sexual nature are characteristic of Staphysagria (in contrast, in Sepia even the thought of sex makes her angry). The Silicea patient is consumed by an increased sense of responsibility, as well as a strange, persistent desire to sit on the floor and count small objects.
Causes of the disease
Prolonged alcohol intoxication, alcoholism and any other intoxication can provoke agitation and aggravate it.
Some infectious diseases can cause symptoms of the described illness, but this is not common. In some professions that involve constant stress, a person may periodically become confused, but this should not be confused with agitation.
In psychiatry, agitation is one of the leading ailments. More than one and a half million people are affected by this disease every year in the United States alone.
Many patients are unable to control themselves while in this state and become dangerous to themselves and others. In view of this, in megacities, closed medical institutions or psychiatric departments are provided for such patients on one of the floors of a regular hospital.
Complications
The development of complications is often associated with late diagnosis and incorrect approach to treating the disorder.
When treating people with severe forms of catatonia, difficulties may arise in the daily care of patients, as a result of which complications may develop:
- aspiration pneumonia - occurs due to the difficulty of eating in patients with mutism and the risk of aspiration;
- risk of deep vein thrombosis and pulmonary embolism due to immobility in people with catatonia;
- metabolic disorders associated with dehydration and exhaustion of the body - patients with catatonia may not eat or drink for a long time;
- disorders of the gastrointestinal tract (constipation, intestinal obstruction, etc.)
- urinary retention or incontinence;
- neuromuscular complications (flexion contracture, nerve palsy)
- formation of bedsores.
Also, in a state of catatonic excitement, the patient poses a danger to himself and others. The sudden onset of an attack of stupor can lead to an accident, overtaking a person driving a car, while crossing the road, at work, etc.
Complications of severe forms of catatonia are difficult to treat due to the difficulties in contact between the patient and the doctor.