Types of stroke Ischemic stroke Cerebral stroke Hemorrhagic stroke Extensive stroke Signs and symptoms of stroke Symptoms in women Symptoms in men First aid for stroke Treatment Rehabilitation and recovery after stroke Rehabilitation at home Rehabilitation in a sanatorium Restoration of the arm after a stroke Exercises for stroke survivors Exercise therapy Restoration of speech after a stroke Exercise equipment for rehabilitation after a stroke Massage for recovery after a stroke Breathing exercises Consequences of a stroke Stroke prevention
Stroke is an acute disturbance of the blood circulation of the brain and, as a consequence, its focal damage. Today, 23% of the Russian population dies from strokes, and among those who overcome the disease, many become disabled.
In this regard, one of the most important tasks of modern medicine is high-quality medical care for stroke and comprehensive rehabilitation of patients who have suffered from the disease.
Types of stroke
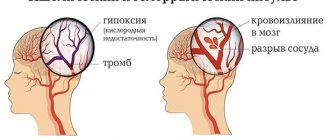
Modern medicine knows two types of strokes: ischemic and hemorrhagic.
Hemorrhagic stroke, in turn, can be expressed as subarachnoid hemorrhage (in the subarachnoid space of the cerebral membranes), parenchymal hemorrhage (in the substance of the brain), hemorrhage in the ventricles of the brain, and mixed.
The periods of stroke are defined as:
- acute (3–5 days from the moment of hemorrhage),
- acute (the first month after a vascular accident),
- early recovery period (6 months after hemorrhage),
- late recovery period – from 6 months to 2 years.
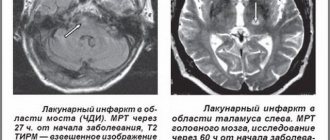
Ischemic stroke
Ischemic stroke is a pathological condition that develops as a progressive general or local lesion in various diseases of the cardiovascular system. Circulatory disorders during ischemic stroke manifest themselves as sudden disturbances in focal or cerebral symptoms that persist for more than a day. This type of stroke often accompanies:
- arterial hypertension,
- coronary heart disease,
- diabetes,
- atrial fibrillation,
- atherosclerosis,
- other vascular diseases.
In addition, the occurrence of ischemic stroke is influenced by hereditary predisposition and age.
Risk factors for ischemic stroke are:
- stress,
- low level of physical activity,
- prolonged psycho-emotional stress,
- excess weight,
- smoking.
Brain stroke
In medicine, strokes include cerebral infarction (ischemic stroke), cerebral hemorrhage (hemorrhagic stroke) and subarachnoid hemorrhage.
Among all types of stroke, ischemic brain damage is the most common. In layman's language, a stroke is often called a cerebral hemorrhage. In fact, hemorrhages account for only a quarter of cases of cerebral stroke. The vast majority of strokes are ischemic strokes (up to 85% of cases).
The incidence of stroke increases significantly with age, starting at age 45. 95% of strokes are diagnosed after the age of 45, of which 75% are diagnosed after the age of 65 years.
Hemorrhagic stroke
Hemorrhagic stroke is a spontaneous, unprovoked hemorrhage into the cranial cavity. Often it occurs as a consequence of vascular disease of the brain:
- amyloid angiopathy,
- atherosclerosis,
- hypertension.
In addition, hemorrhage can be provoked by fibrinolytic drugs and anticoagulants, cocaine and amphetamine.
Modern medicine distinguishes:
- intracerebral (parenchymal),
- subarachnoid,
- ventricular,
- mixed hemorrhages.
The clinical picture of hemorrhagic stroke is characterized by an acute onset:
- severe headache
- dizziness,
- nausea and vomiting,
- a progressive decrease in the level of wakefulness (up to coma).
With extensive hemorrhage or its deep localization, secondary stem symptoms quickly appear. With hemorrhage in the brain stem and extensive hematomas of the cerebellum, consciousness and speech functions are rapidly damaged.
The first month is the most difficult period of the disease. This is associated with progressive cerebral edema, increased dislocation and cerebral symptoms. It is dislocation and swelling of the brain that is the main cause of death in the acute period of stroke. By the beginning of the second month of the disease, the clinical picture clearly indicates the consequences of focal brain damage, by which the patient’s prospects for recovery are judged.
Major stroke
A major stroke is the most severe type of cerebrovascular accident, leading to the death of areas of the brain. In a major stroke, the lesions are large and the pathological foci are multiple, affecting the large supplying arteries. The rapid loss of oxygen in the brain causes the death of nerve cells, the body loses the most important functions: vision, hearing, movement.
Extensive lesions develop quickly, but even with these severe forms of stroke, approximately 20% of patients have a chance of recovery.
Mechanism of pathogenesis
Spinal stroke accounts for approximately 1–1.5% of all CNS pathologies associated with acute hemodynamic disorders. The greatest prevalence occurs in the age category from 30 to 70 years, regardless of gender. The bulk of spinal strokes are of the ischemic type, and the overwhelming majority of lesions occur in the lower thoracic and/or lumbar region.
Impaired blood flow in the vessels causes oxygen deficiency (hypoxia), neural metabolic failures and hemorrhages in the pathological area. The sudden development of such conditions does not give the body time to react adequately, launch compensatory processes and rebuild the metabolism of neurons. A hemorrhagic zone is formed, the consequence of which is neurological necrosis. This condition is called “spinal stroke.”
Signs and symptoms of stroke
Symptoms of a stroke are usually quite obvious, however, in some rare cases, a stroke can occur without symptoms. Symptoms may also appear and disappear within two days. At the very beginning of a stroke, the symptoms are the most severe, and if treatment is not started on time, the first symptoms will turn into irreversible changes in the brain.
The main symptom is a very severe headache. It is characterized by suddenness, is more pronounced when lying down, and intensifies when changing body position or coughing. Symptoms:
- drowsiness,
- loss of consciousness,
- decreased wakefulness,
- hearing impairment,
- taste,
- vision,
- tactile sensitivity,
- confusion of thoughts,
- difficulty swallowing,
- memory loss.
A stroke may be characterized by:
- violation of control over the physiological processes of the body,
- loss of balance,
- inability to speak, read and write,
- lack of coordination
- understanding someone else's speech,
- severe muscle weakness or numbness in an arm, leg, or face (usually on one side of the body).
Symptoms in women
Stroke occurs in women at any age.
Often the symptoms of a stroke in a woman are atypical, so women often confuse stroke with other diseases. On the eve of a stroke, a woman may experience:
- attacks of sharp or dull pain in the chest,
- blood pressure surges,
- high anxiety,
- redness of the face and bulging veins on the temples,
- heart rate up to 120 beats/min.,
- stomach ache,
- prostration,
- weakness in arms and legs.
Also, cerebral circulation disorders in women may be indicated by:
- tremor of the limbs,
- the appearance of awkward unnatural movements,
- loss of sensation in legs and arms,
- speech function disorder,
- blurred vision,
- lack of coordination
- transient amnesia,
- loss of balance.
Most often, women develop hemorrhagic stroke due to high blood pressure. This is facilitated by changes in hormonal levels, increased sensitivity to stress, and changes in blood clotting due to oral contraceptives.
Symptoms in men
For men, at the first signs of a stroke, the manifestation of motor activity disorders is more typical:
- weakness in arms and legs,
- disorientation in space,
- impaired coordination of movements,
- unsteady gait.
Common symptoms of stroke in men:
- severe headaches for which pain relief with pills does not help,
- vomit,
- high salivation,
- difficulty swallowing,
- decreased speech function,
- double vision,
- fear of light and sounds,
- prostration,
- drowsiness,
- weakness,
- convulsions.
Focal symptoms occur after general cerebral symptoms on the second day of stroke:
- numbness of the limbs,
- decreased skin sensitivity,
- memory loss,
- drooping eyelids.
Depending on the location of the damage to the cerebral arteries, symptoms of a stroke appear in a man:
- in the cerebellum - severe nausea and vomiting, pain in the back of the head. The patient cannot stand;
- in the brain stem - sudden loss of consciousness, paralysis, coma;
- in the ventricles - fainting;
- in the parietal lobe – tactile disturbances and spatial disorientation;
- in the temporal lobe – speech disorientation and hallucinations;
- in the frontal lobe - depression, aggressive behavior, seizures.
Diagnostics
When diagnosing spinal strokes, it is important to determine the stage of development of the pathological process and the mechanism of its triggering. The list of instrumental examinations includes:
- computed tomography of the spinal column;
- collection of cerebrospinal fluid (lumbar puncture);
- spinal angiography;
- electroneuromyography of muscle tissue.
The reason against which the disease began to develop is determined together with highly specialized doctors and general practitioners (therapist, hematologist, endocrinologist, etc.). Laboratory diagnostics involves a detailed blood test, coagulogram, etc.
First aid for stroke
When a person has a stroke, there are several external signs that are important for everyone to know:
- the corners of the lips are located on different lines due to difficulty contracting the facial muscles,
- arms are not raised symmetrically,
- pronouncing words is difficult.
Signs of ischemic stroke appear even before changes in brain tissue develop. Their name is the initial manifestations of insufficiency of blood supply to the brain (IPNCM).
NPNCM can be identified at home using the L.S. questionnaire. Manvelova. One positive answer (+) is equal to one point. To confirm the diagnosis, you should answer yes at least twice to the questions about the presence of the following sensations at least once a week or constantly during the last three months:
- headache without clear localization, often associated with fatigue and changes in weather;
- dizziness, increasing with changes in body position in space;
- noise in the head is constant or transient;
- memory impairment, which extends to current events; logical memory, as a rule, does not suffer;
- sleep and/or performance disorders.
Two or more points indicate the prerequisites for the rapid development of a stroke and the need to take preventive measures.
After identifying signs of a stroke, you must call an ambulance
, the patient should take a horizontal position, head slightly higher than the body, remove dentures, eye lenses and glasses. In the absence of consciousness, open the patient’s mouth slightly, tilting his head slightly to one side, and monitor his breathing.
Before the ambulance arrives, prepare a list of medications the patient is taking, information about drug intolerance, and prepare documents for hospitalization. Assistance to the patient in a hospital setting will be provided in accordance with the standards of medical care for patients with stroke, approved by Order of the Ministry of Health and Social Development of the Russian Federation dated August 1, 2007 N 513.
What to do if a person has a stroke?
- First of all, call an ambulance. Sometimes the minutes count.
- Provide fresh air, open windows and doors, and free the person’s neck from constricting clothing.
- Leave the person where the attack occurred. The patient cannot be moved.
- Elevate the person's head and upper body 30 degrees by placing several pillows under the thoracic spine.
- If vomiting occurs, turn the person's head to the side and ensure that the vomit passes away so that the person does not suffocate.
- In the event of an epileptic attack, carefully hold the person, turn his head to the side and insert an object wrapped in cloth into his mouth - a stick, a comb, a spoon.
- In case of cardiac arrest, immediately begin compressions through the chest and perform artificial respiration.
- Wait for the ambulance.
Treatment
A favorable outcome in stroke is highly dependent on the time of initiation of qualified medical care.
The first stage of treatment is aimed at restoring blood flow through the thrombosed artery, minimizing the risks of developing cerebral edema and convulsions, and reducing the risk of complications from the heart and blood vessels.
During intensive stroke therapy, blood pressure is constantly monitored and this indicator is maintained 10% above the patient’s “working” pressure in order to establish blood supply to the brain. Monitoring of heart rhythm and metabolic rates in the body is carried out.
For ischemic stroke (cerebral infarction), conservative treatment methods are used. Within 5 hours from the first signs of cerebral infarction, thrombolytic intravenous therapy is administered to dissolve the blood clot that has blocked the cerebral vessel. Therapy is carried out only with the consent of the patient (he must be conscious) or his relatives with the exact time of hemorrhage confirmed by CT.
If it is impossible to perform thrombolysis, the patient is prescribed antiplatelet drugs that reduce the formation of blood clots.
For treatment after a stroke, aspirin, dipyridamole, and clopidogrel are used no later than 48 hours. Aspirin is also prescribed in the future; patients take it up to a year after the stroke.
Surgical interventions are common for hemorrhagic strokes. Due to them, blood clots are removed with minimal damage to the brain substance, intracranial pressure is reduced, and liquor dynamics are restored.
- Contraindications for surgery:
- patient age over 75 years,
- coma,
- presence of severe diabetes,
- renal failure,
- oncology.
Antispasmodics are used to relieve vascular spasms during hemorrhagic strokes. During the first 24 hours after a stroke, the patient is prescribed medications to increase blood clotting.
Causes
Acute disorders of blood circulation in the spinal cord have a multifaceted etiology, but all factors, one way or another, lead to vascular damage - spasms, ruptures, compression, and the development of thromboembolism. Spinal stroke is divided into two main categories based on its causes:
- Primary vascular damage.
- Secondary hemodynamic disturbance.
The first group includes pathologies affecting the functioning of blood vessels:
- rare anomalies - aneurysms, defects of venous and arterial development with slow blood flow. Thinning of the tissues of the vascular walls leads to rupture and hemorrhage;
- deformation of the walls of blood vessels - atherosclerotic, varicose and similar disorders most often become the cause of ischemic stroke of the spinal cord;
- ruptures - damage as a result of spinal injuries, as a consequence of surgery, anesthesia, or puncture of the spinal column.
The second group consists of hemodynamic failures:
- anatomical and neurological abnormalities (hernias, displacements, osteochondrosis, spondylolisthesis, etc.);
- tumor formations on the spine and spinal cord with compression of nearby vessels, metastasis, hemorrhages;
- diseases of the hematopoietic system with impaired hemostasis (hemophilia, coagulopathy, etc.).
Often the cause of a spinal stroke consists of various factors, the most common in importance. As a rule, this applies to obesity, arterial hypertension, nicotine addiction, etc.
Rehabilitation and recovery after stroke
The recovery program after a stroke should be comprehensive and include:
- quality patient care,
- drug treatment,
- restoration of lost skills through gymnastics,
- physiotherapy,
- massage.
Rehabilitation measures also include psychotherapeutic assistance and social adaptation. The rehabilitation period takes several months or years and requires patience and perseverance.
When drug therapy is used:
- aspirin,
- beta blockers,
- diuretics,
- ACE inhibitors,
- calcium channel blockers statins,
- muscle relaxants,
- anticonvulsants,
- nootropic and neurotrophic agents,
- antidepressants.
Rehabilitation at home
Treatment after a stroke at home is carried out under the constant supervision of a neurologist. It is also aimed at preventing recurrent strokes, the risks of which are significant in the first two years after a stroke.
Treatment includes a set of rehabilitation measures related to the restoration of vital functions (movement, thinking, speech, vision, hearing), drug therapy, exercise therapy and breathing exercises.
Rehabilitation in a sanatorium
Treatment in sanatoriums is aimed at:
- consolidation of treatment results,
- normalization of blood circulation,
- prevention of recurrent stroke,
- increased performance and restoration of motor activity,
- maintaining psycho-emotional health.
The following basic methods are used:
- hardware treatment,
- manual therapy,
- exercise therapy,
- classes with a speech therapist,
- massage,
- acupuncture,
- laser treatment,
- magnetotherapy,
- hirudotherapy.
Sanatoriums for rehabilitation after a stroke are available to anyone who has had the disease, except those who:
- can't take care of himself
- suffers from severe arrhythmia,
- has mental disorders
- serious speech and motor impairments,
- epilepsy.
When choosing a sanatorium, preference is given to treatment in a specialized sanatorium with proven programs for recovery after strokes. A set of procedures requires recommendations from the treating neurologist.
Restoring a hand after a stroke
Due to impaired blood circulation in the brain, the hand after a stroke often loses sensitivity and mobility. It is necessary to begin rehabilitation of the hand in a timely manner so that the regeneration of nerve cells in the brain occurs and its mobility is restored. Most often, the hand goes numb and ceases to obey when the right hemisphere of the brain and cerebellum are damaged.
Psychological and physical rehabilitation helps restore the hand. Faith in treatment will help the patient recover faster and undergo the rehabilitation course more easily. It includes:
- drug therapy,
- exercise therapy,
- massage,
- rubbing and compresses,
- hydrotherapy,
- acupuncture,
- activities to develop fine motor skills.
The hand needs simple exercises:
- flexion-extension of fingers,
- grabbing objects
- raising your hand up,
- spreading to the sides
- modeling,
- writing and drawing.
It is important for the patient to be encouraged to eat and dress independently. Swimming is recommended if possible.
Rehabilitation exercises should be performed 2-3 times a day, physical therapy is prescribed once a day for 3-4 months. The duration of each rehabilitation session is from 10 minutes to an hour.
The task of the rehabilitation therapist is to help the patient remember how he moved his arm before the stroke and restore this action. At first, moving at least one finger can be considered a success. It is important to remember that restoring a hand after a stroke is a very long process, which does not imply giving up rehabilitation due to physical pain and despair from poor results.
It is correct to start the exercises with the large muscles of the healthy arm, mentally repeating all the movements of the affected arm. Exercises need to be changed daily, using objects or special exercise equipment. It is important to work out the entire arm, paying special attention to the fingers and shoulder muscles.
Simple exercises for every day include:
- clenching your fingers into a fist and straightening,
- flexion and extension of the arm at the elbow,
- clapping hands,
- grabbing objects
- rolling a ball on a hard surface.
After the first month of simple exercises, you can move on to training your shoulders and forearms with light dumbbells. Wrist workout includes:
- sculpting,
- letter,
- drawing,
- training with a rubber ring.
To develop the entire limb, you can train using checkers and chess, a Rubik's cube, a children's construction set, collecting buttons or matches.
At the same time, drug therapy is used to restore the arm, in which baclofen, tizanidin-teva, klonopin, and phenol are used.
After medical advice, you can use folk remedies to restore your hand. The most popular of them:
- ointment based on bay leaves and pine needles;
- compresses with alcohol tincture of pine cones and sage (200 ml of vodka per tablespoon of herb);
- sage baths,
- ointments made from propolis and fat.
About half of patients suffer from arm paralysis after a stroke, while 75% return their limbs to normal after six months of rehabilitation procedures.
Exercises for stroke survivors
Complexes and special programs are prepared by the treating neurologist, and the exercises can be performed at home or in exercise therapy rooms. Exercises include complexes of physical therapy, aerobic exercises, complexes for the restoration of motor activity and balance training.
The full rehabilitation package includes:
- massage of the limbs - every 3 hours daily;
- extension/flexion of arms and legs - 2 times a day for half an hour;
- exercises to restore speech and memory;
- breathing exercises.
Exercises can be physical and mental. The latter restore memory, speech, vision, hearing, concentration and thinking.
When performing any exercise, it is important that the patient feels good. If you experience headaches, dizziness, weakness, changes in blood pressure and other symptoms of circulatory disorders, exercise should be stopped.
Every patient who has suffered a stroke needs to undergo long-term rehabilitation, which can last for years. At the same time, it is important to remember that recovery after a stroke is not only possible, but also not uncommon, and to make every effort for successful rehabilitation.
Exercise therapy
Exercise therapy often begins after an acute period of stroke in a hospital. After discharge, as recommended, you can continue them at home. Exercise therapy relieves muscle spasms, restores motor activity and cerebral circulation.
If a stroke has completely or partially paralyzed a person, then the exercises in the first month of training only include changing the patient’s body position every three hours.
After this, they begin to perform a passive exercise therapy complex: massage and extension/flexion of the arms and legs. After the first successes in independent movements, you can perform more active exercises.
Medicine defines four stages of exercise therapy training for patients after a stroke:
- acute (classes in the first weeks after a stroke in a hospital);
- early (classes in the first six months in rehabilitation centers or at home);
- late (in six months of the second half of the first year after the stroke);
- long-term (one year after the stroke).
Exercise therapy training is carried out at a certain time, several times a day according to a planned set of exercises.
Restoring speech after a stroke
Speech and articulation suffer to one degree or another in all patients after a stroke, therefore special training complexes have been developed to restore speech function. They usually include simple exercises:
- smile, hold for 10 seconds;
- rotate with protruding tongue;
- roll your tongue into a tube;
- pronounce the alphabet, words and tongue twisters;
- click your tongue;
- bite your lips.
Each exercise is performed according to an increasing pattern, starting with 4-5 times, increasing to 30 – 40 repetitions.
Exercise equipment for rehabilitation after stroke
Therapeutic exercises after a stroke involve the use of special exercise equipment. In a hospital or sanatorium setting, the attending physician will prescribe an exercise regimen for rehabilitation. The necessary equipment is available in rehabilitation centers and sanatoriums.
The simulators are intended for:
- restoration of the musculoskeletal system,
- fine motor skills,
- for kinesiotherapy and vibration therapy,
- restoration of walking.
For patients after a stroke, there are special lifts and multifunctional exercise machines to restore many functions at the same time.
At home, to train fine motor skills, use a Rubik's cube, spiked rubber balls, modeling clay, and an expander.
Massage for recovery after stroke
Any set of training after a stroke necessarily includes massage. They start it immediately, in a hospital setting, as soon as they receive permission from the doctor. The massage begins with light stroking of the arms and legs to gently restore blood circulation. The intensity of the massage needs to be increased. After just a few days, the massage includes body turns and massage of the back and chest. Massage techniques for the rehabilitation of patients with stroke are quite simple, but it is important to learn how to perform them correctly. During the entire rehabilitation period (up to one year), massage using a special complex is one of the main forms of recovery.
In this case, just as with exercise therapy exercises, the massage complex should be determined by the doctor, and you should not deviate from it. Independent decisions here can cause harm to the patient.
Breathing exercises
Breathing exercises after a stroke are an essential part of rehabilitation. It restores oxygen access to the brain and normalizes cerebral circulation. Breathing exercises can be performed without equipment, but exercises with breathing simulators are most effective.
Today, the best-selling breathing simulator in Russia is Samozdrav. Its effectiveness lies in the fact that with each workout it ensures the supply of the required volume of oxygen to the blood and cells of the body, maintains a normal level of carbon dioxide, which naturally relieves vascular spasm.
Classes with Samozdrav not only restore blood supply to the brain, but also significantly reduce the risk of a recurrent stroke. Thus, classes at Samozdrav are both rehabilitation measures and a reliable form of secondary prevention of stroke.
The advantage of the simulator is that the load for the patient increases gradually, the first sessions do not exceed three minutes. The simulator is suitable for bedridden patients; it is suitable for use while lying down throughout the entire training session.
Its effect is as gentle as possible on the body affected by a stroke. It does not cause overload, like physical exercise, but if it is impossible to engage actively, it can become a simulator of physical activity by increasing blood circulation and bringing the muscles to the desired tone.
Thus, “Samozdrav” has a comprehensive restorative effect on the body of patients who have suffered a stroke, and can be used at home, being today the main simulator for breathing exercises.
Consequences of a stroke
Many patients recover their body fairly quickly after a stroke, while others permanently forget many vital functions. Among the sad consequences of strokes:
- movement disorders
- paralysis,
- speech disorder,
- atactic disorders,
- partial or complete loss of vision,
- dementia,
- epileptic seizures,
- peripheral edema,
- swelling of the legs after a stroke.
The most severe consequences of a stroke are cerebral edema and coma. The greatest likelihood of justifying favorable prognoses occurs with transient ischemic attacks (pre-stroke condition), micro-strokes, as well as timely therapy within five hours after the onset of the first signs of the disease.