Encephalitis and meningitis are inflammatory conditions that affect the central nervous system. Encephalitis is an inflammation of the brain, while meningitis is an inflammation of the membranes that protect the brain and spinal cord.
Encephalitis and meningitis can develop as a result of certain viral, bacterial, fungal, and parasitic infections. Both conditions have similar symptoms and require immediate diagnosis and treatment to help prevent complications.
This article outlines the differences between encephalitis and meningitis, including their associated symptoms, causes, and risk factors. In addition, we will briefly provide information about the treatment and prevention of these diseases and give recommendations when it is necessary to seek medical help.
Encephalitis
is a medical term for inflammation of the brain.
Meningitis
is a medical term meaning inflammation of the membranes. The meninges are protective membranes that surround the brain and spinal cord.
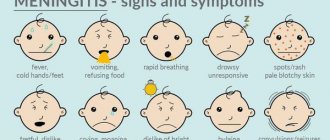
The symptoms of encephalitis and meningitis are similar, but not identical.
Symptoms of encephalitis
Symptoms of encephalitis are as follows:
- flu symptoms
- sudden fever
- headache
- vomit
- convulsions
- visual impairment
- increased sensitivity to light
- increased stiffness of the neck and back muscles
- muscle weakness
- unsteady gait
- speech and hearing impairment
- irritability
- drowsiness
- confusion or disorientation
- changes in personality or behavior
- hallucinations
- sudden memory loss
- loss of consciousness
Meningoencephalitis of newborns
The most common pathogen is viruses. Intrauterine infection of a baby occurs from a mother suffering from glandular fever, measles, rubella, herpetic infection, and mumps.
The most common symptoms are focal disorders, hyperkinesis, hydrocephalus. Nonspecific manifestations of meningoencephalitis in newborns:
- Eye twitching;
- Difficulty feeding from the breast;
- High fever;
- Intoxication syndrome;
- Vomiting reflex;
- Diarrhea;
- Strabismus;
- Increased heart rate (tachycardia);
- Muscle twitching.
Neurologists define neurological disorders in the form of Kernig's sign (the inability to bring the head to the chest due to stiff neck muscles). Cerebrospinal fluid contains an increased amount of lymphocytes and protein.
Causes of meningitis and encephalitis
Both encephalitis and meningitis can result from infection with the following pathogens, such as:
- bacteria
- viruses
- mushrooms
- parasites
Encephalitis
Common causes of encephalitis:
- herpes simplex viruses types 1 and 2
- arboviruses, which are spread through bites from infected ticks and mosquitoes
- enteroviruses, which can spread between people through droplets in the air when they cough or sneeze
In some cases, encephalitis may develop as a result of an autoimmune condition.
Meningitis
The causes of meningitis depend on the type of meningitis.
Viral meningitis
Viruses that can cause meningitis include:
- enteroviruses
- varicella zoster virus, which causes chickenpox and shingles
- influenza virus
- herpes simplex type 2
- HIV
Bacterial meningitis
Bacteria that can cause meningitis include:
- Pneumococcus: Causes pneumococcal meningitis.
- Neisseria Meningitides: Causes meningococcal meningitis.
- Escherichia Coli
Fungal meningitis
Fungi that can cause meningitis include:
- Cryptococcus: lives in the environment in most parts of the world.
- Histoplasma: Lives mainly in soil.
- Blastomyces: Lives in moist soil and decaying wood and leaves.
Parasitic meningitis
According to the Centers for Disease Control and Prevention (CDC), parasitic meningitis is much less common than viral and bacterial meningitis.
The following parasites can cause a rare form of meningitis called eosinophilic meningitis
:
- Angiostrongylus cantonensis
: can be transmitted to people who eat raw snails or slugs. - Baylisascaris Procyonis
: Can be transmitted to people who come into contact with animal feces contaminated with parasites. - Gnathostoma spinigerum
: can be transmitted to people who consume any of the following raw or undercooked animal products: poultry - freshwater fish or eel
- frog
- snakes
Additional risk factors for developing meningitis
The following group of people have an increased risk of developing meningitis:
- infants
- people traveling to endemic areas
- college students, especially freshmen
- military recruits
- people living in dormitories
Other groups of people at high risk of developing meningitis include:
- Older adults and newborns
: have an increased risk of developing E. coli meningitis. - Children under 2 years of age
: Children in this age group are at increased risk of pneumococcal meningitis.
Treatment
Both encephalitis and meningitis are conditions that require immediate treatment. Infectious disease doctors will typically provide treatment in an inpatient setting.
Treatment of encephalitis
Treatment for encephalitis may include antiviral drugs for viral encephalitis, such as acyclovir and ganciclovir, and immunosuppressive drugs for autoimmune encephalitis.
Treatment of meningitis
Treatment for meningitis may include:
- antibiotics to treat bacterial meningitis
- intravenous antifungal drugs for fungal meningitis
Patients also require treatment for symptoms of encephalitis or meningitis. Treatment may include:
- corticosteroids to control inflammation and swelling of the brain
- medications to relieve headaches and reduce fever
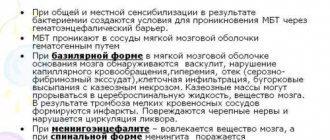
Manifestations of meningoencephalitis in adults
Various symptoms of the disease in an adult are caused by different pathogens and characteristics of the course. The incubation period of the disease lasts several weeks.
Symptoms of the clinical stage:
- Muscle stagnation;
- Decreased appetite;
- Constant fatigue;
- Headaches without the effectiveness of painkillers.
Inflammatory changes in the meninges lead to meningeal syndrome with special manifestations:
- Nausea;
- Speech disorders;
- Interruptions of heart activity;
- Respiratory disorders.
The occurrence of the described manifestations leads to death. The progression of individual symptoms becomes a cause of disability.
Prognosis for meningitis and encephalitis
The prognosis depends on the severity of the disease and how quickly the patient is diagnosed and treated. Encephalitis or meningitis is often mild. For people with mild symptoms, recovery may take 2-4 weeks.
In severe cases, encephalitis and meningitis can lead to long-term neurological damage or even death.
Encephalitis
Recovery from encephalitis may depend on the severity of the condition and the degree of inflammation in the brain. Symptoms of encephalitis may last 1-2 weeks. Fever and neurological symptoms may resolve gradually or suddenly.
Meningitis
With treatment, patients with bacterial meningitis may show improvement within 48 to 72 hours, although they may be at high risk of complications. Treatment with antibiotics can significantly reduce the risk of death from most types of bacterial meningitis.
Viral meningitis is usually not life-threatening, and patients with mild illness can make a full recovery in 7 to 10 days without treatment.
Meningococcal infections
Meningococcal infection is an infectious disease caused by the bacterium Neisseria meningitidis
. There are 12 serogroups (varieties) of this bacterium, of which 6 (A, B, C, W, Y and X) cause most severe forms of meningococcal infection. The peculiarity of the infection is that meningococcus, like Haemophilus influenzae type b and pneumococci, has a polysaccharide capsule that surrounds the bacterium and protects it from attacks by the immune system. Young children (aged 0 to 5 years) usually do not yet have developed protective immunity against this infection. (1)
Reasons and sources. Incubation period
The causative agent of meningococcal infection is transmitted only from person to person. The infection spreads by airborne droplets and enters the body through the mucous membranes of the nose, mouth and pharynx. The smallest drops of secretions from the respiratory tract, oral cavity or nasopharynx of a carrier or a sick person during close contact - kissing, sneezing, coughing - fall on the mucous membrane of a healthy person. There, bacteria can remain and multiply for some time without causing signs of disease or affecting well-being, causing asymptomatic carriage (sometimes symptoms of a runny nose [nasopharyngitis] are observed). According to available data, it is believed that at any given time, about 10-20% of the population are carriers of meningococci. But sometimes, for reasons that are not entirely clear, suppressing the body’s defenses, the infection penetrates through the mucous membrane into the blood. Using nutrients in the blood, meningococci can multiply rapidly, causing blood poisoning (sepsis), and spread through the blood into the membranes of the brain or other internal organs (for example, lungs, joints, heart, subcutaneous fat, etc.). (12)
The time between the moment a bacterium enters the body and the first signs of illness appears is called the incubation period . For meningococcal infection, it averages 4 days, but can vary from 2 to 10 days. (2)
Forms of the disease
The forms of the disease mean what the nature of the disease is, how it progresses, what organs and systems it affects. In cases of meningococcal infection, the following forms exist:
- Localized forms. They develop when the body’s defenses cope with the infection and it does not enter the blood.
- Asymptomatic carriage: bacteria Neisseria meningitidis
remains on the mucous membrane, multiplies and is periodically released into the external environment. The person himself is not sick, but is contagious to others.
- Acute nasopharyngitis: inflammation is limited to the nasal mucosa and nasopharynx.
- Generalized forms - meningitis , meningoencephalitis, sepsis (blood poisoning). They develop if the pathogen overcomes the local immune defense on the mucous membranes of the nasopharynx and enters the blood. With the bloodstream, bacteria spread throughout the body, penetrating the skin, kidneys, adrenal glands, lungs, heart tissue, and membranes of the brain. The reproduction and death of meningococci leads to the release of endotoxin, a toxic product of bacterial breakdown. It destroys the walls of blood vessels, causing hemorrhages to form, which at first look like a rash ( exanthema ) - reddish dots on the skin or enanthema - as well as rashes on the mucous membranes of the mouth, nasopharynx, and sometimes the eyes, and then take on the typical appearance of hemorrhagic (from dark red to black) rash ranging in size from dots to extensive necrosis (death) of skin areas. The same bacterial toxin leads to the development of cerebral edema and brain symptoms, hemorrhages in the internal organs.
- Mixed (a combination, for example, of meningitis and sepsis) and rare forms: the development of inflammation in the joints - polyarthritis, in the lungs - pneumonia, etc. (1) (2) (3)
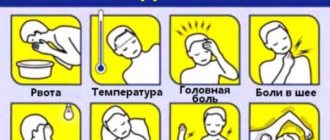
Symptoms of meningococcal infection
Carriage. It proceeds without complaints, lasts on average 10-15 days, the pathogen is detected only during laboratory examination.
Acute nasopharyngitis. Symptoms of meningococcal acute nasopharyngitis may resemble ARVI - fever, weakness, headache, drowsiness, mucus and slight nasal congestion. It may result in recovery, transition to carrier status, or cause the development of meningitis and other severe forms of meningococcal infection. In any case, even with minimal suspicion or risk of infection with meningococcus, you need to call a doctor, since it is impossible to independently determine whether it is really meningococcal nasopharyngitis or another infection: an examination and laboratory tests are necessary.
Meningococcemia (sepsis, blood poisoning). It develops quickly, often against the background of nasopharyngitis. The temperature may rise sharply, with muscle aches, severe headaches, and clouding of consciousness. Within 1-2 days, a typical rash appears during meningococcal infection - first pinkish, then hemorrhagic: uneven rashes, dark red in color, slightly raised above the skin. As a rule, the rash is localized on the buttocks, legs, and lower torso. The elements of the rash are very different, from “pinprick” and red-brown “stars” to large hemorrhages, which in severe cases lead to tissue death - necrosis. An unfavorable sign is the early appearance of a rash on the face. (1)
Meningitis . According to the source (1) in Russia, “50% of all bacterial meningitis in children under 5 years of age” is caused by meningococcus. Meningococcal bacterial meningitis begins acutely, the temperature can quickly increase to high numbers, and at the same time complaints of pain in the back, neck, severe headache with intolerance to light and sounds may appear. Vomiting is repeated many times, it does not bring relief. Consciousness is confused, the person shrinks into a ball: he lies on his side, with his legs pulled up to his stomach, a typical description of this sign is “the posture of a pointing dog.” The general condition is usually severe or very severe.
Symptoms can quickly develop - sometimes on the first day, but more often 2-3 days after the onset of signs of the disease - indicating that the infectious-inflammatory process has affected the membranes of the brain and caused their irritation. Such symptoms are called meningeal, they include: stiff neck (impossible to press the chin to the chest), Kernig’s symptoms (the doctor cannot straighten the patient’s leg at the knee), Brudzinsky’s (simultaneous bending of the head and pulling the legs towards the stomach) and others. A typical rash may appear. (13)
Meningeal symptoms can indicate the severity of the disease, but you should not determine it on your own, without a doctor: a comprehensive check and experience in assessing symptoms is needed.
Meningoencephalitis. Inflammation affects the meninges, brain, and sometimes the spinal cord. Signs are similar to those of meningitis, and a rash also develops. exanthema and enanthema may appear . An exanthema is a variety of skin rashes that can occur with a variety of infections and allergies; this is a general description of rashes. Enanthema is a rash of a different nature that appears on the mucous membranes. At the very beginning of meningoencephalitis, it may be difficult to determine the type of rash. It may begin as roseola, a small, 1 to 10 mm in diameter, rounded red lesion that lightens or disappears when pressed. Then it can turn into a hemorrhagic rash in the form of dots, spots, stars of different sizes, which do not disappear when you press on them. (13)
Meningococcal sepsis (menigococcemia) is a severe form of the disease. The condition of the patients is very serious: severe headache, vomiting, the temperature can be either very high - 41 ° C, or below 36.6 ° C. This is due to a very rapid disruption of the functioning of blood vessels, a drop in blood pressure. A maculopapular rash : spreading over the skin and mucous membranes, it often merges to form blisters with bloody contents. The mortality rate for this form is very high - up to 60%. (13)
Diagnosis of meningococcal infection
An accurate diagnosis can only be made after a laboratory test: if the doctor suspects meningococcal infection, he will prescribe a test of blood, cerebrospinal fluid, mucous discharge and rash.
According to the source (1), even with a timely and correct diagnosis and correctly prescribed treatment, “the risk of death is high. In the 10-20% of people who survive, bacterial meningitis can cause brain damage, hearing loss or learning difficulties. In severe cases, gangrene of the fingers, toes, and ears is possible.” Therefore, if at least one of the symptoms that resembles the description of the symptoms of meningococcal infection, sepsis and any other forms develops, it is recommended to call an ambulance.
A preliminary diagnosis, and then its clarification, is possible only after a clinical examination, with the obligatory collection of cerebrospinal fluid - cerebrospinal fluid, as well as smears from the surface of the nasopharyngeal mucosa and rash using a spinal puncture. According to source (1), “Meningococcal disease is potentially fatal and should always be treated as a medical emergency. The patient must be admitted to the hospital.”
Treatment
Treatment depends on the form of the disease. Hospitalization is required for any form, but if, when asymptomatic carriage of meningococcal infection and nasopharyngitis is detected, antibiotics and vitamin and mineral preparations can be prescribed, then other forms of the disease require emergency intervention and intensive treatment . (13)
Depending on the form of the disease, the characteristics of the course, the age of the patient and other reasons, antibiotics may be prescribed; their combination and dose adjustment may be required. You may also need medications to reduce fever, relieve seizures, improve blood circulation and for detoxification, maintain the functioning of the cardiovascular system, brain, and reduce the risk of possible complications. Other measures to maintain vital functions, including ventilation, may be required. For treatment to be as effective as possible, “it is important to identify the serogroup of meningococcus and test the microorganism for sensitivity to antibiotics.”(3)
At-risk groups
The infection caused by meningococcus is equally dangerous for all people except those who have received the meningococcal vaccine. According to WHO (2), 10–20% of the population are considered asymptomatic carriers of the meningococcal bacterium N. meningitidis
. The following groups are at increased risk for the development of meningococcal infection (1) (2) (3):
- Children of primary and preschool age. In the absence of vaccination, protective immunity against meningococci in children under 5 years of age, as a rule, has not yet been formed. It is also important that children often put toys and environmental objects in their mouths, share food with each other, and drink from common dishes. This increases the risk of transmission of infection if there is a child or adult asymptomatic carrier of meningococci without signs of disease .
- Teenagers and young adults with a large number of social contacts, living and communicating in crowded conditions (parties, discos, dormitories, barracks). As stated above, about 10-20% of people are considered possible asymptomatic carriers of meningococcal disease. The more and more intense the contacts, the higher the risk of becoming infected.
- For the same reason, conscripts and recruits are at risk.
- Persons who have had their spleen removed, with HIV infection, or with certain genetic disorders. These are people with immunodeficiency—reduced ability of the body to resist infections.
- Persons with cochlear implants. If you have hearing impairment and wear a cochlear implant, there may be damage to the internal structures of the ear and a decrease in local immunity, which may pose a certain risk of infection.
- Travelers to areas where the incidence of disease is high, the countries of the so-called “meningitis belt” in Africa, as well as to Saudi Arabia for the Hajj. A long dry period, wind, dust from dry soil, cold nights, and the prevalence of upper respiratory tract infections reduce the protective capabilities of the nasopharyngeal mucosa. Low indicators of socio-economic development (except in the UAE and Saudi Arabia), overcrowding, displacement of large numbers of people due to traditional nomadic lifestyles, and in Saudi Arabia due to pilgrimage, increase the risk that large numbers will gather in relatively small areas people, among whom there may be asymptomatic carriers of meningococcal infection and patients, which can lead to outbreaks of infection.
Prevention
The short incubation period , the difficulty of early diagnosis, the rapid development of symptoms, the prevalence of carriage, the characteristics of children's immunity, the high level of mortality and disability, as well as the high prevalence of infection in some countries of the world require preventive measures in children and individual adults at risk.
In case of outbreaks of meningococcal infection (limited or in epidemics), so-called outbreak measures can be carried out by medical workers. These include the establishment of quarantine, identification and isolation of carriers, compliance with the sanitary and epidemiological regime, and other measures. (3)
The most effective measure is active immunization, that is, preventive vaccination. In Russia, it is included in the Calendar of Preventive Vaccinations for Epidemic Indications (4). It states that vaccination is required for “children and adults in areas of meningococcal infection caused by meningococcal serogroups A or C. Vaccination is carried out in endemic regions, as well as in the event of an epidemic caused by meningococcal serogroups A or C.” Persons subject to conscription for military service are also subject to vaccination. (4)
The list of vaccines that can be used in Russia for vaccination against meningococcal infection includes:
- Meningococcal polysaccharide vaccines:
- monovalent (against serogroup A) - dry polysaccharide;
- tetravalent (against serogroups A, C, Y and W).
- Meningococcal conjugate vaccines:
- monovalent (against serogroup C).
- tetravalent (against serogroups A, C, Y and W). (5) (6)
According to the World Health Organization, “conjugate vaccines are preferable to polysaccharide vaccines because they can provide herd immunity and also have higher immunogenicity, especially in children under 2 years of age.” (7)
Show sources
Sources
- Meningococcal infection. [Electronic resource]. URL: https://www.yaprivit.ru/diseases/meningokokkovaya-infekciya (as of 07/04/2017)
- World Health Organization. Meningococcal meningitis. Newsletter No. 141, November 2015 URL: https://www.who.int/mediacentre/factsheets/fs141/ru (accessed 07/04/2017)
- Berezhnova I.A. Infectious diseases. — Textbook / I.A. Berezhnova - M.: RIOR. - 2007. - 319 p.
- Order of the Ministry of Health of the Russian Federation dated March 21, 2014 No. 125n “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications” (with amendments and additions). URL: https://normativ.kontur.ru/document?moduleId=1&documentId=282161 (as of 07/04/2017)
- Abramtseva M.V., Tarasov A.P., Nemirovskaya T.I. Meningococcal infection. Conjugate polysaccharide meningococcal vaccines and new generation vaccines / Biological products. Prevention, diagnosis, treatment. - 2021 - volume 16, no. 1 (57) - p. 42.
- State register of medicines of the Russian Federation. URL: https://grls.rosminzdrav.ru (as of 07/04/2017)
- World Health Organization. Meningococcal vaccines: WHO position paper, November 2011. Wkly Epidemiol Rec 2011; 86:521-539. URL: https://www.who.int/wer/2011/wer8647.pdf (accessed 07/04/2017)
SPRU.MENAC.18.03.0032
When to Seek Medical Help
It is important that people see a doctor immediately if they notice symptoms of encephalitis or meningitis. To diagnose the disease, the doctor will ask about your symptoms and medical history and perform a physical examination.
If the doctor suspects encephalitis or meningitis, he may prescribe the following additional diagnostic methods:
- blood tests to identify pathogens
- cerebrospinal fluid analysis
diagnostic imaging techniques of the head and chest to detect inflammation in the brain and spinal cord
ICD 10 code for meningoencephalitis
The international classification of the tenth revision identifies the following types of brain inflammation with code “G04”:
- Meningomyelitis;
- Meningoencephalitis;
- Acute ascending myelitis.
The category excludes multiple sclerosis (“G95”), toxic, alcoholic encephalopathy “G31.2”, “G92”.
Classification of meningoecephalitis by course:
- Chronic – long-term development with a slow increase in symptoms;
- Subacute - erased signs of nosology increase over two to three years;
- Acute – rapid progression of symptoms helps early diagnosis;
- Fulminant – rapid cerebral damage causes death.
The difficulties of verifying pathology are complicated by the variety of etiological factors.