Encephalitis
21372 November 18
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Definition
Encephalitis is a group of diseases characterized by inflammation of the brain. Currently, encephalitis is called not only infectious, but also infectious-allergic, allergic and toxic brain damage.
Causes of encephalitis
Primary encephalitis, which includes tick-borne encephalitis, herpetic encephalitis, encephalitis caused by the Coxsackie virus (A9, B3, B6), ECHO (2, 11, 24) and some others, arise as a result of the penetration of the virus through the blood-brain barrier, causing damage neurons of the brain and the inflammatory process develops.
Secondary encephalitis is considered as a complication of previous infectious diseases: influenza, rubella, measles, chickenpox, leptospirosis, etc., as well as post-vaccination encephalitis.
Influenza encephalitis is caused by influenza viruses A1, A2, A3, B. The pathogenetic mechanisms of influenza infection are toxic brain damage and cerebral circulatory failure.
The causative agent of rubella encephalitis is an RNA virus of the Togaviridae
.
Measles encephalitis is caused by the measles virus and is a form of damage to the brain (and sometimes the spinal cord) (encephalomyelitis). Encephalitis is considered the most common neurological complication of measles (more than 95% of all cases of neurological complications). It is observed with a frequency of 1:1000 cases of measles, most often in children over 2 years of age - both boys and girls.
Post-vaccination encephalitis can develop after vaccination, especially after the administration of certain rabies vaccinations. Post-vaccination encephalitis is based on a cross-autoimmune reaction to vaccine antigens and brain antigens, which is morphologically expressed in inflammatory damage to the cerebral vessels and surrounding brain matter.
Leptospirosis encephalitis is caused by Leptospira interrogans
. The source of infection is infected domestic animals. Leptospirosis is most common in the southern regions. Autoimmune reactions are of great importance in the development of the disease.
The group of subacute sclerosing leukoencephalitis includes forms of chronic and subacute encephalitis with a progressive severe course (Dawson's inclusion encephalitis, subacute sclerosing leukoencephalitis of Van Bogart, nodular panencephalitis of Pette Doering).
Since the differences in their clinical picture and morphology are insignificant, they are currently treated as one disease, most often under the name “subacute sclerosing panencephalitis.”
Persistent viral infections play an important role in the development of the disease: measles, enterovirus, tick-borne encephalitis virus. In patients with subacute sclerosing panencephalitis, very high titers of measles antibodies are found in the blood and cerebrospinal fluid (not observed even in patients with acute measles infection). In addition, autoimmune mechanisms, as well as acquired or congenital defects of the immune system, occupy a significant place.
Classification of the disease
The classification of encephalitis reflects the factors leading to the development of the disease, and the associated clinical manifestations and course features.
According to the timing of occurrence, they are distinguished:
- Primary encephalitis is an independent disease caused primarily by neurotropic viruses:
- viral: multiseasonal (herpetic, enterovirus, influenza, cytomegalovirus, rabies virus, etc.); arboviral, or vector-borne (tick-borne, mosquito (Japanese), Australian Murray Valley, American St. Louis); caused by an unknown virus (epidemic);
- microbial and rickettsial (for syphilis, Lyme disease, typhus, etc.);
- measles, rubella, chickenpox;
- post-vaccination;
- bacterial and parasitic (staphylococcal, streptococcal, tuberculosis, toxoplasma, chlamydial, malarial, etc.)
The disease can occur in acute, subacute, chronic and recurrent forms and affect various parts of the brain.
There are moderate, severe and extremely severe encephalitis.
Symptoms of encephalitis
Primary polyseasonal encephalitis
The incubation period can vary from 2-3 days to several weeks. Prodromal phenomena are observed in the form of decreased appetite, lethargy, and low-grade fever. The onset of the disease occurs against the background of a sharp rise in temperature. The severity of clinical manifestations and their course can be different - from mild erased forms to severe fulminant forms, in which death occurs on the 1st-2nd day of the disease. The duration of the acute period ranges from 3-5 days to several weeks. A severe course with pronounced and rapidly progressing cerebral edema is observed mainly in encephalitis of herpetic etiology.
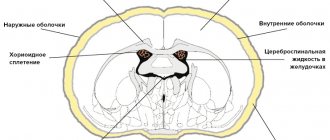
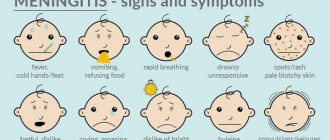
General cerebral symptoms come to the fore: vomiting, convulsive paroxysms, lethargy, disturbances of consciousness, and possible respiratory and cardiovascular disorders. The predominance of cerebral manifestations, disturbances of consciousness and pronounced meningeal symptoms (i.e., involvement of the cerebral membranes in the inflammatory process) are more typical for young children.
Focal symptoms depend on the localization of pathological changes in the brain—stem, cerebellar, and hemispheric forms are distinguished.
Cerebellar syndrome
is characterized by acute loss of coordination, tremor, and muscle hypotonia. It has the most favorable course with complete regression of these symptoms and without subsequent delay in psychomotor development, even in young children.
Stem syndrome
manifested by damage to the cranial nerves and pyramidal tracts passing through the trunk. A specific disturbance of gait and coordination of movements occurs, caused by pathological work of the vestibular apparatus, there are oculomotor disorders (strabismus, gaze paresis, double vision), severe muscle hypotonia, which is then replaced by spastic paresis of the arms and legs. Disorders of swallowing, sucking, and phonation develop less frequently. Neuroendocrine disorders are possible, and in severe cases, cardiac and respiratory disorders of central origin, which can cause death.
Hemispheric syndrome
more often accompanied by disorders of consciousness, disturbances of orientation in space and time, and lethargy. Episodes of psychomotor agitation and hallucinatory syndrome are possible. In the first days, epileptic attacks occur, which, as a rule, are preceded by paresis that develops acutely and stroke-like.
Typical symptoms of the onset of herpetic encephalitis
- fever, headache, mental dysfunction, epileptic seizures, muscle weakness, memory loss. Then there is a violation of behavior, speech and movement coordination disorder.
Secondary encephalitis in general infections
Clinical picture of influenza encephalitis
develops more often at the end of the disease and even 1-2 weeks after recovery: the patient’s health deteriorates again, body temperature rises, and general cerebral symptoms occur (headache, vomiting, dizziness). Possible damage to the peripheral nervous system in the form of neuralgia of the trigeminal and greater occipital nerves, lumbosacral and cervical radiculitis, damage to the sympathetic nodes. Leukocytosis or leukopenia is determined in the blood. The current is favorable. The disease lasts from several days to a month and ends with complete recovery.
Measles encephalitis
develops acutely, most often on the 3-5th day after the appearance of the rash. By this point, body temperature may have returned to normal, but often rises again to high values. Meningeal symptoms are identified, manifested by headache, dizziness, nausea, vomiting, impaired consciousness (excitement, delirium, hallucinations); damage to the cranial nerves is observed; impairment of motor function of the limbs and function of the pelvic organs. In severe cases, mortality reaches 25%, and the severity of encephalitis does not depend on the course of measles.
Encephalitis due to chickenpox
- severe infectious-allergic disease. Its clinical picture develops on the 3-7th day after the appearance of the rash (rarely at a later date or before the period of the rash) and is manifested by hyperthermia, coma, convulsions, meningeal symptoms (headache, dizziness, nausea, vomiting, impaired consciousness), motor dysfunction. Signs of cerebral edema appear early. The course is usually favorable and only in isolated cases is it very severe with the risk of death. After recovery, paresis, hyperkinesis, and convulsive seizures may persist for a long time.
Encephalitis due to rubella
may develop 1-10 (usually 2-5 days) after the appearance of the rash. There are known cases of manifestation of acute encephalitis several days before the appearance of the rash, as well as without rashes, which complicates the diagnosis. Most often, encephalitis develops in children aged 3-15 years; in adults, cases of encephalitis are described as casuistry. Rarely, neurological symptoms are accompanied by secondary rashes.
Leptospirosis encephalitis is characterized by an acute onset and occurs as a respiratory viral infection. There is an undulating fever with muscle pain. Subsequently, the clinical picture may be dominated by symptoms of liver and kidney damage, and from the 2-3rd week - damage to the nervous system in the form of encephalitis or encephalomyelitis involving the cranial nerves. The course of the disease is usually favorable, and spontaneous recovery is sometimes possible.
Subacute sclerosing leukoencephalitis
Mostly children and adolescents under 15 years of age are affected, but sometimes the disease is also recorded in adults. The onset of the disease is subacute: symptoms appear that are regarded as neurasthenic - absent-mindedness, irritability, fatigue, tearfulness.
There are 4 stages of sclerosing leukoencephalitis:
- Stage 1 lasts up to 6 months: personality changes, mood swings or depression are possible, fever and headache may be present;
- Stage 2 may include seizures, muscle spasms, vision loss and dementia;
- Stage 3 is characterized by rapid progression of dementia, increased muscle tone with weakening of the convulsive syndrome. At this stage, complications can be fatal;
- Stage 4 is characterized by disturbances in breathing, heart rate and blood pressure, leading to coma and death.
The course of sclerosing encephalitis is steadily progressive and always ends in death.
In 80% of cases, the disease lasts 1–3 years, 10% of patients live longer (up to 10 years), in 10% a fulminant course is described, when death occurs in less than 3 months.
There is no specific treatment. Diagnosis of encephalitis
The purpose of diagnosing primary multiseasonal encephalitis is to establish the type of pathogen. For this purpose, a series of serological studies is carried out. A multiple increase in antibody titer to a specific virus is of diagnostic significance when comparing the results of a study of the patient’s serum taken at the onset of the disease and 2 weeks later.
Encephalitis caused by the herpes simplex virus is detected by determining the increase in the level of specific antibodies IgM and Ig G in the blood.
How to remove a tick?
The longer the tick suction lasts, the higher the risk of infection entering the human body. Therefore, it is necessary to remove the tick as quickly as possible. To remove a tick, it is best to go to a trauma center. You can also remove the tick yourself. For this purpose, special devices have been developed - a lasso handle, a pliers-screwdriver. These products can be purchased at pet stores. In extreme cases, a regular strong thread will do. You need to know that you cannot use oil, cream or other liquids to remove ticks yourself. This will not help prevent the disease, but will make it more difficult to remove the vector.
If self-removal of the tick went smoothly, then the remaining wound must be treated with an antiseptic solution. But if, during the process of removing the tick, the head separated from the body and remained in the human skin, or if the tick was unsuccessfully crushed by hand, then you need to seek help from a trauma center and get a referral to a consultation with an infectious disease doctor.
Vaccinal prevention
Currently, the vaccine is developed only for the prevention of tick-borne viral encephalitis.
Routine vaccination against tick-borne viral encephalitis is carried out for residents of regions endemic for tick-borne encephalitis, and for those who plan to visit these areas. Emergency prophylaxis with human immunoglobulin against TBE is recommended to be carried out no later than 4 days from the moment of tick ingestion (according to Sanitary and Epidemiological Rules 3.1.3.2352-08 Prevention of tick-borne viral encephalitis).
Vaccination is the most reliable method of preventing tick-borne viral encephalitis.