Anticonvulsants: classification and mechanisms of action
According to the modern definition of the International League Against Epilepsy and the International Bureau of Epilepsy in 2005 (ILAE, IBE, 2005), “epilepsy is a disorder (disease) of the brain characterized by a persistent predisposition to the generation (development) of epileptic seizures, as well as neurobiological, cognitive, psychological and social consequences of this condition.” Epilepsy is one of the most common diseases of the nervous system. Worldwide, the prevalence of epilepsy is 4–10/1000 people, corresponding to 0.5–1.0% of the population. [1]
The International Classification of Epileptic Seizures distinguishes two main types: generalized and partial. Generalized seizures include tonic-clonic, tonic, clonic, myoclonic seizures and absence seizures; to partial - simple, complex and secondary generalized. However, the wide variety of seizures does not always allow them to be classified as one of these types of seizures, so another category has been highlighted - “unclassified” seizures, which include 9–15% of seizures. [2] Currently, to differentiate attacks, they use the classification adopted in 1981 in Kyoto, Japan. The ability to correctly differentiate seizures is a necessary component of rational selection of anticonvulsant therapy.
The classification of forms of epilepsy is very extensive, but globally all epilepsy can be divided according to etiology into:
1. Idiopathic (genetic (hereditary) predisposition in the absence of other possible causes of the disease); [3]
2. Symptomatic (the cause of the disease is brain damage due to various factors acting during pregnancy and after childbirth: brain malformations (mainly malformations of the cerebral cortex - cortical dysplasia); intrauterine infections; chromosomal syndromes; hereditary metabolic diseases; hypoxic-ischemic brain damage in the perinatal period (during childbirth, in the last weeks of pregnancy, in the first week of a child’s life); infectious diseases of the nervous system (meningitis, meningoencephalitis); traumatic brain injury; tumors, degenerative diseases of the nervous system); [3]
3. Cryptogenic (epileptic syndromes, the etiology of which is unknown or unclear. The word “cryptogenic” itself is translated as secret, hidden. These syndromes do not yet meet the requirements of the idiopathic variety, but they cannot be classified as symptomatic epilepsy).
The mechanism of action of anticonvulsants (anticonvulsants) is not fully understood. This is largely due to insufficient knowledge of epilepsy as such, since often the cause of convulsive attacks cannot be determined. An imbalance between inhibitory (GABA, glycine) and excitatory neurotransmitters (glutamate, aspartate) is important in the development of epileptogenic activity of the brain. For excitatory amino acids, there are specific receptors in the brain - NMDA and AMPA receptors, associated in neurons with fast sodium channels. It has been established that the glutamate content in brain tissue in the area of the epileptogenic focus is increased. At the same time, the content of GABA in the brain tissues of patients with epilepsy is reduced. [4]
Antiepileptic drugs are classified, usually based on their use in certain forms of epilepsy: [4]
I. Generalized forms of epilepsy - Grand mal seizures (grand mal; tonic-clonic seizures): Sodium valproate. Lamotrigine, Diphenine, Topiramate, Carbamazepine, Phenobarbital, Hexamidine. — Status epilepticus: Diazepam, Clonazepam, Diphenin-sodium, Lorazepam, Phenobarbital-sodium, Anesthesia. - Petit mal; absense epilepsia: Ethosuximide, Clonazepam, Trimethine, Sodium valproate, Lamotrigine. — Myoclonus-epilepsy: Clonazepam, Sodium valproate, Lamotrigine.
II. Focal (partial) forms of epilepsy Carbamazepine, Lamotrigine, Clonazepam, Tiagabine, Sodium valproate, Phenobarbital, Topiramate, Vigabatrin, Difenin, Hexamidine, Gabapentin.
There is also a classification by “generations” of drugs: I - 1st generation anticonvulsants Phenobarbital, Phenytoin, Carbamazepine, Valproic acid, Ethosuximide. II - 2nd generation anticonvulsants Felbamate, Gabapentin, Lamotrigine, Topiramate, Tiagabine, Oxcarbazepine, Levetiracetam, Zonisamide, Clobazam, Vigabatrin. III - 3rd generation anticonvulsants (newest, many in the clinical trial stage) Brivaracetam, Valrocemide, Ganaxolone, Karabersat, Carisbamate, Lacosamide, Losigamon, Pregabalin, Remacemide, Retigabine, Rufinamide, Safinamide, Seletracetam, Soretolide, Stiripentol, Talampanel, Fluorofelbamate, Fosphenytoin, Eslicarbazepine, DP-valproic acid. This post will discuss the main drugs of the 1st and 2nd generations.
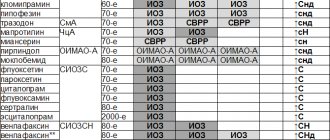
In addition, antiepileptic drugs can be classified based on the principles of their action:
Figure 1. | Sites of action of various drugs on GABA metabolism
I. Sodium channel blockers: Diphenine, Lamotrigine, Topiramate, Carbamazepine, Sodium valproate.
II. T-type calcium channel blockers: Ethosuximide, Trimethine, Sodium valproate.
III. Agents that activate the GABAergic system: 1. Agents that increase the affinity of GABA to GABA-A receptors Benzodiazepines, Phenobarbital, Diazepam, Lorazepam, Clonazepam, Topiramate. 2. Agents that promote the formation of GABA and prevent its inactivation Sodium valproate 3. Agents that prevent the inactivation of GABA Vigabatrin 4. Agents that block neuronal and glial uptake of GABA Tiagabine
IV. Drugs that reduce the activity of the glutamatergic system: 1. Drugs that reduce the release of glutamate from presynaptic terminals Lamotrigine 2. Drugs that block glutamate (AMPA) receptors Topiramate
Sodium channel blockers
Carbamazepine (Tegretol, Finlepsin) is an iminostilbene derivative. The anticonvulsant effect of the drug is due to the fact that it blocks sodium channels in the membranes of nerve cells and reduces the ability of neurons to support high-frequency impulses, typical of epileptogenic activity; blocks presynaptic sodium channels and prevents transmitter release. The drug is metabolized in the liver, increases the rate of its own metabolism due to the induction of microsomal liver enzymes. One of the metabolites, carbamazepine-10,11-epoxide, has anticonvulsant, antidepressant and antineuralgic activity. Excreted mainly by the kidneys (more than 70%). Side effects: loss of appetite, nausea, headache, drowsiness, ataxia; violation of accommodation; diplopia, heart rhythm disturbances, hyponatremia, hypocalcemia, hepatitis, allergic reactions, leukopenia, thrombocytopenia, agranulocytosis (blood picture monitoring is required). There is a risk of developing teratogenic effects. Carbamazepine increases the metabolic rate, as a result of which it reduces the concentration of certain drugs in the blood, including antiepileptic drugs (clonazepam, lamotrigine, sodium valproate, ethosuximide, etc.).
Phenytoin (Difenin) is a derivative of hydantoin. Anticonvulsant effect: blockade of sodium channels; reducing the entry of sodium ions into neurons; disruption of the generation and propagation of high-frequency discharges; decreased excitability of neurons, preventing their activation when impulses arrive from an epileptogenic focus. To prevent seizures, phenytoin is prescribed orally in tablet form. Phenytoin sodium is used to relieve status epilepticus and is administered intravenously. Phenytoin intensively binds to plasma proteins (90%). Metabolized in the liver, the main inactive metabolite, 5-(p-hydroxyphenyl)-5-phenylhydantoin, is conjugated with glucuronic acid. It is mainly excreted from the body by the kidneys in the form of metabolites. Side effects: dizziness, agitation, nausea, vomiting, tremor, nystagmus, ataxia, diplopia, hirsutism; gingival hyperplasia (especially in young people), decreased folate levels and megaloblastic anemia, osteomalacia (associated with impaired vitamin D metabolism), allergic reactions, etc. Teratogenic effects have been noted. Causes the induction of microsomal enzymes in the liver and thus accelerates the metabolism of a number of drugs (corticosteroids, estrogens, theophylline), increases their concentration in the blood.
Lamotrigine (Lamictal) blocks sodium channels in neuronal membranes and also reduces the release of glutamate from presynaptic terminals (which is associated with blockade of sodium channels in presynaptic membranes). Side effects: drowsiness, diplopia, headache, ataxia, tremor, nausea, skin rashes. [5]
T-type calcium channel blockers
Ethosuximide (Suxilep) belongs to the chemical class of succinimides, which are derivatives of succinic acid. Anticonvulsant effect: blocks T-type calcium channels involved in the development of epileptic activity in the thalamocortical region. It is the drug of choice for the treatment of absence seizures. Metabolized in the liver. It is mainly excreted from the body by the kidneys in the form of metabolites and about 20% of the administered dose is unchanged. Side effects: nausea, vomiting, dyskinesia; headache, drowsiness, sleep disturbances, decreased mental activity, anxiety, allergic reactions; rarely - leukopenia, agranulocytosis.
The mechanism of action of some antiepileptic drugs includes several components and it is not established which of them is predominant, as a result of which these drugs are difficult to classify into one of the above groups. Such drugs include valproic acid and topiramate.
Valproic acid (Acediprol, Apilepsin, Depakine) is also used in the form of sodium valproate. Anticonvulsant effect: 1) blocks sodium channels of neurons and reduces the excitability of neurons in the epileptogenic focus; 2) inhibits the enzyme that metabolizes GABA (GABA transaminase) + increases the activity of the enzyme that is involved in the synthesis of GABA (glutamate decarboxylase); increases the content of GABA in brain tissue; 3) blocks calcium channels. It is excreted mainly by the kidneys in the form of conjugates with glucuronic acid or as oxidation products. Side effects: nausea, vomiting, diarrhea, stomach pain, ataxia, tremor, allergic skin reactions, diplopia, nystagmus, anemia, thrombocytopenia, impaired blood clotting, drowsiness. The drug is contraindicated in cases of impaired liver and pancreas function.
Topiramate (Topamax) has a complex, not fully understood mechanism of action. It blocks sodium channels and also increases the action of GABA on GABA-A receptors. Reduces the activity of excitatory amino acid receptors (presumably kainate). The drug is used for adjunctive treatment of partial and generalized tonic-clonic seizures in combination with other antiepileptic drugs. Side effects: drowsiness, lethargy, decreased appetite (anorexia), diplopia, ataxia, tremor, nausea. [5]
Drugs that increase GABAergic activity
Phenobarbital (Luminal) interacts with specific binding sites (barbiturate receptors) located on the GABA-A receptor complex and, causing allosteric regulation of the GABA-A receptor, increases its sensitivity to GABA. At the same time, the opening of chlorine channels associated with the GABA-A receptor increases - more chlorine ions enter the cell through the neuron membrane and hyperpolarization of the membrane develops, which leads to a decrease in the excitability of neurons in the epileptogenic focus. In addition, it is believed that phenobarbital, interacting with the neuron membrane, causes a change in its permeability for other ions (sodium, potassium, calcium), and also exhibits antagonism towards glutamate. Metabolized in the liver; the inactive metabolite (4-hydroxyphenobarbital) is excreted by the kidneys in the form of a glucuronide, about 25% unchanged. Side effects: hypotension, allergic reactions (skin rash), feeling of weakness, drowsiness, depression, ataxia, nausea, vomiting. Phenobarbital causes a pronounced induction of microsomal liver enzymes and therefore accelerates the metabolism of drugs, including the acceleration of the metabolism of phenobarbital itself. With repeated use it causes the development of tolerance and drug dependence.
Benzodiazepines (Clonazepam) stimulate benzodiazepine receptors of the GABA-A receptor complex; The sensitivity of GABA-A receptors to GABA increases and the frequency of opening of chlorine channels increases, the entry of more negatively charged chlorine ions into the cell is stimulated, resulting in hyperpolarization of the neuronal membrane and increased inhibitory effects of GABA. Side effects: fatigue, dizziness, loss of coordination, muscle weakness, depression, disturbances in thinking and behavior, allergic reactions (skin rash). With long-term use in children, clonazepam can cause impairment of mental and physical development. When administered parenterally, respiratory depression (up to apnea), hypotension, and bradycardia are possible. Vigabatrin (Sabril) is a structural analogue of GABA and irreversibly inhibits GABA transaminase, which breaks down GABA. Increases GABA content in the brain. Vigabatrin has a wide spectrum of anticonvulsant action, is used to prevent grand mal seizures, and is effective for partial seizures.
Gabapentin (Neurontin) was created as a lipophilic structural analogue of GABA to stimulate GABAA receptors in the brain. However, it does not have GABA-mimetic activity, but has an anticonvulsant effect. The mechanism of action is not clear; it is assumed that the drug promotes the release of GABA; the possibility of blocking the transport systems of excitatory amino acids cannot be ruled out. Gabapentin is used as an adjunct in the treatment of partial seizures. The drug is effective for neuropathic pain. Side effects: drowsiness, dizziness, ataxia, tremor, headache. [5]
Sources:
- Alekseev V.V., Yakhno N.N. Main syndromes of damage to the nervous system // Diseases of the nervous system. Ed. NN Yakhno, DR Shtulman. Moscow - 2001
- Zatsepilova T. A., Alyautdin R. N. Pharmacology. — 2004.
- Kharkevich D. A. Pharmacology: Textbook – 10th ed., revised, revised. and additional //M.: GEOTAR-Media, 2010. - 752 p. — 2010.
- Epilepsy // Fact sheet N°999. WHO October 2012
- https://vk.cc/70bi6o
Modern principles of antiepileptic therapy in adults
Epilepsy is a chronic brain disease that requires many years, and in 30% of cases lifelong use of antiepileptic drugs. The goal of treating epilepsy is to prevent the development of seizures. For this purpose, modern antiepileptic drugs (AEDs) are used. However, the goal cannot be achieved at any cost. The current concept is that treatment of epilepsy is more than just seizure control, although seizure freedom is very important. Thus, we are talking about changing the treatment strategy: from quantitative to qualitative care for patients with epilepsy. Carrying out comprehensive rehabilitation (medical and non-medicinal) allows people with epilepsy to lead a full, unrestricted, productive life in the absence of seizures and side effects of AEDs.
Achieving complete cessation of epileptic seizures in patients with epilepsy is not only clinically, but prognostically significant. The complete absence of attacks in the patient helps prevent various medical and social consequences, such as physical damage (trauma, etc.), mental disorders (depression, anxiety, etc.), social consequences (alienation in society, discrimination, etc.). ), and in the future, taking into account various factors after achieving drug remission, to achieve complete cessation of drug use.
Modern prescription of antiepileptic drugs is based on taking into account many factors, primarily the definition of the epileptic syndrome, the type of seizures, as well as age, gender, concomitant pathology, social status and the “wishes” of the patient himself. To identify an epileptic syndrome, at the time of diagnosis, clinicians must rely on a number of factors: seizure type, electroencephalogram (EEG) (with and without seizure), etiology, changes on magnetic resonance imaging (MRI), response to AED treatment, take into account heredity and anamnestic data, the history of the present disease.
Over the past two decades, the main treatment strategy for epilepsy has been the use of only one AED, i.e. monotherapy (Baulac M., 2003). Clinical data have shown that epilepsy monotherapy is associated with better tolerability, fewer adverse events, lower toxicity, and a lower risk of teratogenicity. In addition, monotherapy avoids the use of complex dosing regimens, achieves higher patient compliance, and reduces the cost of treatment compared to polytherapy. Moreover, some studies have shown that polytherapy compared to monotherapy does not provide any advantages in terms of controlling the development of epileptic seizures and reducing the number of side effects (Schmidt D., 1995, Baulac M., 2003, Kanner A., 2005) . An early example is a 1983 study of institutionalized patients with intellectual disabilities who were switched from polytherapy to monotherapy. The study showed that epileptic seizures did not occur in 78% of patients, and many patients became more alert (Bennett H., 1983).
The initial prescription of AEDs to patients with epilepsy in a monotherapy mode allows achieving drug remission in 50% of cases. The inclusion of alternative monotherapy, if the primary one is ineffective, ensures the absence of attacks in 10% of patients.
The use of monotherapy for epilepsy is justified: in case of a initially diagnosed disease, in case of ineffectiveness of polytherapy, in a situation where the possibilities of monotherapy have not been fully used, and if there are no epileptic seizures during polytherapy.
Initial treatment of epilepsy should always be carried out in the form of monotherapy with drugs registered for use in this regimen. In Russia, both “old” and “new” antiepileptic drugs are registered and can be used in monotherapy for the treatment of epilepsy. The “old” registered drugs include traditionally used ones - barbiturates, carbamazepines (Tegretol, Finlepsin), phenytoin, ethosuximide (Suxilep), drugs of valproic acid and its derivatives (Depakine, Konvulex), the “new” ones - lamotrigine (Lamictal, Konvulsan), topiramate (Topamax), oxcarbazepine (Trileptal), levetiracetam (Keppra). For comparison, in the United States, antiepileptic drugs approved by the Food and Drug Administration (FDA) for the treatment of epilepsy for initial monotherapy of most types of epileptic seizures include both the “older” generation drugs (phenytoin, carbamazepine and sodium valproate) and newer drugs: topiramate and oxcarbazepine. Lamotrigine is approved for conversion to monotherapy. Randomized trials have also shown the use of lamotrigine (Lamictal, Convulsan) and levetiracetam (Keppra) as initial treatment for epilepsy (Faught E., 2007).
There is evidence of the advantages of new AEDs compared to traditional ones, which is reflected in good effectiveness combined with less toxicity, better tolerability and ease of use, as well as the absence of the need for regular monitoring of drug concentrations in the blood (Ochoa JG, Riche W., 2002).
Various studies based on evidence-based medicine and based on literature reviews provide different recommendations about which drugs should be prescribed to patients depending on the form of epilepsy (French J., 2004, NICE, 2006, Glauser T., 2006). Thus, the recommendations of the American Academy of Neurology (AAN) and the American Epilepsy Society (AES) indicate the validity of the use of both “old” and “new” drugs for monotherapy in newly diagnosed epilepsy. The main thing is that the choice of AED should depend on the individual characteristics of the patient. For epileptic seizures of the nature of partial/mixed seizures, the following new drugs can be used: lamotrigine (Lamictal, Convulsan), topiramate (Topamax), oxcarbazepine (Trileptal), levetiracetam (Keppra); for newly diagnosed absence seizures, lamotrigine ( Lamictal, Convulsan).
For the treatment of adult patients with refractory partial epilepsy, the AAN and AOE recommend the use of oxcarbazepine (Trileptal) and topiramate (Topamax) as monotherapy and gabapentin (Neurontin), lamotrigine (Lamictal, Convulsan), tiagabine, topiramate (Topamax), oxcarbazepine (Trileptal), levetiracetam (Keppra) or zonisamide as adjunctive therapy (French J., 2004). Topiramate (Topamax) is recommended for the treatment of refractory generalized tonic-clonic seizures in adults, and, like lamotrigine (Lamictal, Convulsan), for the treatment of drop attacks in Lennox-Gastaut syndrome (French J., 2004). In our country, drugs such as tiagabine and zonisamide are currently not registered and cannot be officially used, while pregabalin (Lyrica) is registered as an additional therapy in adults with partial seizures.
Recommendations for the use of new AEDs, published in the UK by the National Institute (NICE), are based on randomized controlled trials (RCTs) and systematic reviews in which new AEDs are compared with each other, with older drugs and with placebo (NICE, 2006 ). In general, these recommendations are more conservative than the AAN recommendations. NICE guidelines indicate that the use of new AEDs is justified in the following cases: the use of an older drug will not provide benefit, the use of an older drug is contraindicated due to possible interactions with other agents, there is a previous negative experience with these drugs or indications of their poor tolerability, treatment women of childbearing age (Beghi E., 2001, NICE, 2006).
The International League Against Epilepsy (ILAE) recommendations are based on a structured review of the literature in which the quality of clinical trial evidence was used to determine the level of recommendation. These recommendations focus on the effectiveness of drugs for the treatment of newly diagnosed or previously untreated epilepsy (Glauser T., 2006). For the treatment of adult patients with generalized tonic-clonic seizures, none of the AEDs has the highest level of evidence, however, the most effective drugs for monotherapy in these situations, according to RCT data, are carbamazepine (Tegretol, Finlepsin), lamotrigine (Lamictal, Convulsan), oxcarbazepine (Trileptal), phenobarbital, phenytoin, topiramate (Topamax) and valproate (Depakine, Convulex). For the treatment of adult patients with newly diagnosed partial seizures, carbamazepine (Tegretol, Finlepsin) and phenytoin are considered effective for initial monotherapy, while valproate is considered likely effective, and gabapentin (Neurontin), lamotrigine (Lamictal, Convulsan), oxcarbazepine (Trileptal) , phenobarbital, topiramate (Topamax) appear to be less effective. Recommendations for the treatment of elderly patients with partial seizures include carbamazepine, gabapentin (Neurontin) and lamotrigine (Lamictal, Convulsan) - all of these drugs have the highest level of evidence of effectiveness (Glauser T., 2006).
In the adult population, there are two categories of patients that require special attention: elderly patients and women.
Epilepsy and single epileptic seizures are widespread in elderly patients. The cause of attacks is diseases of the brain of vascular or other origin, leading to the appearance of focal symptoms. The incidence of epilepsy after 60 years, according to the study, is 25% of all newly diagnosed cases of the disease in this age group. Taking into account the presence of various somatic and/or other pathologies, monotherapy in elderly patients is preferable for the treatment of epilepsy (Hauser W., 1992, Pohlmann-Eden B., 2005). Treatment of elderly patients with epilepsy is a separate challenge (Faught E., 1999). The damage caused by seizures in these patients may be more severe, and the duration of the post-seizure state may be longer. Despite the fact that the effect of seizures on performance in older people is less, deprivation of work due to seizures is still difficult for this category of patients to tolerate. The pharmacokinetic characteristics of antiepileptic drugs also undergo changes in elderly patients. This concerns protein binding, distribution of the drug and its elimination, which can lead to a decrease in drug clearance, as well as an increase in receptor sensitivity, all of which increases the risk of dose-related side effects (Bourdet S., 2001). Perhaps most importantly, older patients take a large number of medications, which greatly increases the risk of pharmacokinetic and pharmacodynamic drug interactions. Thus, carbamazepine (Tegretol, Finlepsin), phenytoin, valproates (Depakine, Konvulex), barbiturates interact with drugs often taken in old age - warfarin, digoxin, antipsychotics, antacids and antibiotics; to a lesser extent, topiramate (Topamax) and oxcarbazepine (Trileptal) interact ), and lamotrigine (Lamictal, Convulsan) and levetiracetam (Keppra) have virtually no effect (Pohlmann-Eden B., 2005).
Treatment of elderly patients should begin with the lowest possible dose of the drug and increase it gradually, and it does not matter which drug was chosen for therapy (Pohlmann-Eden B., 2005). To minimize the risk of side effects and toxic effects of drugs, it is recommended to start therapy with half the dose recommended for adult patients, increase the dose to half or two thirds of the optimal dose, and also slow down the time of increasing the dose of the drug.
It is also important to prevent the worsening of existing problems due to limited options for choosing drugs. Thus, phenytoin should not be prescribed to patients with impaired coordination, valproates (Depakine, Konvulex) can aggravate the course of essential tremor, cardiac conduction disturbances may occur when using carbamazepine (Tegretol, Finlepsin), sedatives are not recommended for use in patients with drowsiness or dementia (French J., 2004, Sheth R., 2004). Levetiracetam (Keppra), while effective, without drug interactions and well tolerated, can cause behavioral disorders and drowsiness. Lamotrigine (Lamictal, Convulsan) - effective, with some drug-drug interactions, can cause allergic reactions and insomnia. Oxcarbazepine (Trileptal) is effective, has fewer drug interactions than carbamazepine, and can cause hyponatremia and dizziness. Topiramate (Topamax) is effective and well tolerated, especially in low doses, can worsen cognitive impairment and reduce weight (Pohlmann-Eden B., 2005). In elderly patients, an additional risk factor is the possibility of liver enzyme induction, which in turn increases the risk of drug interactions.
Another group that requires special attention are female patients. The characteristics and functioning of the female reproductive system influence the course of epilepsy and the use of antiepileptic drugs. During different periods of life of women with epilepsy, various hormonal, physiological and other changes occur, which require special attention to the treatment of the disease in this group of patients, especially during childbearing age (O'Brien M., 2005, Tettenborn B., 2006, Thomas S ., 2006).
Epileptic seizures, as well as drugs used to relieve them, affect conception, and after conception, the health of the mother and fetus, and the condition of postmenopausal women with epilepsy. In this regard, problems associated with the therapy of women are important and relevant. First of all, these are contraception, pregnancy, the use of AEDs during pregnancy, teratogenicity and many other issues that generally define the concept of female epilepsy.
Antiepileptic drugs, as well as the disease itself - epilepsy, can affect the likelihood of conception and pregnancy, increase the risk of polycystic ovary syndrome (PCOS) and disturbances in the pharmacokinetics of oral contraceptives (OC). Signs and symptoms of PCOS include enlarged or structural abnormalities of the ovaries, oligomenorrhea, amenorrhea, infertility due to chronic anovulation, elevated plasma androgens, and central obesity. Moreover, women with epilepsy are at greater risk of developing multiple ovarian cysts than women in the general population. Although there is conflicting evidence regarding the relationship between AED use and the development of PCOS, some studies indicate that certain AEDs may increase the risk of developing this disease. Researchers' attention was mainly focused on valproate (Depakine, Konvulex), although a reliable causal relationship with this drug was not identified. Despite this, some researchers suggest monitoring the duration of the menstrual period and the level of androgens in the blood plasma in women with epilepsy during treatment with valproate (Isojarvi J., 2005).
When using AEDs in women with epilepsy receiving oral contraceptives, unwanted or unplanned pregnancy may occur. The relative risk of contraceptive failure in women taking OCs and CYP450-inducing AEDs concomitantly is estimated to be 25 times higher than in women without epilepsy who take OCs alone. The main mechanism of contraceptive failure is associated with an increase in the activity of liver enzymes (CYP450), which leads to accelerated metabolism of estrogens to inactive substances, which is accompanied by a decrease in the concentration of estrogens in the blood plasma, the occurrence of ovulation and pregnancy. AEDs that induce liver enzymes may also lead to an increase in the level of sex hormone binding globulin (SHBG), which will be accompanied by a decrease in the level of free biologically active progesterone and estrogen and the onset of unplanned pregnancy (Crawford P., 2002, Zupanc M., 2006).
As a rule, most PCs do not affect the effectiveness of AEDs. At the same time, PCs are known to significantly reduce the level of lamotrigine (Lamictal, Convulsan) in the blood plasma and increase the risk of epileptic seizures when treated with this drug (Sabers A., 2001). Therefore, when taking PC, dose adjustment of lamotrigine is necessary. To confirm the creation of a therapeutic concentration of this drug, drug monitoring is important.
The pregnancy period is very important in a woman’s life, and therefore minimizing the factors that can cause its termination is a rather difficult task that requires a competent and comprehensive approach. The development of the embryo and fetus can be affected by both uncontrolled epileptic seizures and PEP (Tettenborn B., 2006). Therefore, the goal of treatment of epilepsy during pregnancy should be to ensure effective control of the development of epileptic seizures and minimize the undesirable effects of AEDs, which are known to be teratogens. Recurrent seizures during pregnancy are associated with risks for both mother and fetus and may often be associated with inappropriate use of AEDs. The benefits of appropriate AED therapy usually outweigh the risks associated with such therapy, since inadequate treatment of epilepsy during pregnancy is accompanied by the development of repeated epileptic seizures. The use of AED monotherapy, as opposed to polytherapy, is associated with a lower risk of teratogenicity.
The effect of pregnancy on the development of epileptic seizures varies among different patients, but in a fairly large proportion of women (from 17% to 37%), the frequency of seizures increases (Pennell P., 2003, Study Group, 2006). The reasons for this phenomenon may be hormonal changes, a decrease in plasma concentrations of AEDs due to pharmacokinetic changes associated with pregnancy, as well as low compliance with therapy (Sabers A., 2001, Tettenborn B., 2006). In pregnant women with an increased frequency of epileptic seizures, subtherapeutic plasma concentrations of AEDs are often recorded. In addition, some patients with nausea or vomiting during pregnancy may experience impaired absorption of AEDs taken (Tettenborn B., 2006). Pharmacokinetic changes caused by pregnancy are due to an increase in volume of distribution, higher renal elimination of the drug, altered liver enzyme activity, and decreased plasma protein levels (Pennell P., 2003, O'Brien M., 2005). In this regard, it is necessary to regularly monitor the level of AEDs in the blood plasma at each trimester of pregnancy and immediately after. The greatest attention should be paid to patients taking lamotrigine (Lamictal, Convulsan), the clearance of which increases significantly during pregnancy, which can lead to an increase in the incidence of epileptic seizures (Tran T., 2002, de Haan G.-J., 2004). On the contrary, immediately after childbirth, the plasma level of lamotrigine (Lamictal, Convulsan) increases again. This indicates that plasma levels of lamotrigine (Lamictal, Convulsan) should be monitored before conception, during pregnancy and after childbirth, and dosage adjustments are necessary to prevent the development of epileptic seizures and drug toxicity. These provisions also apply to all other PEP.
Evidence that convulsions during pregnancy is a teratogenic factor is conflicting; at the same time, doubts about the fact that AEDs increase the risk of teratogenicity are insignificant (Perucca E., 2005). This effect of AEDs has been clearly established for traditional drugs; For newer drugs, the risk of teratogenicity is the same or slightly lower, although data for these new drugs are limited and insufficient to draw a definitive conclusion.
It should be remembered that a physician treating a pregnant woman with epilepsy must weigh the benefits of using AEDs against the risks to the health of the fetus.
Regardless of age and gender, all patients may experience side effects from the medications they take.
All used AEDs can lead to dysfunction of the central nervous system, including impairment of cognitive ability (A., 2003). According to various authors, more than 60% of patients indicate the presence of subjective complaints about the side effects of medications. Most often, central nervous system disorders (fatigue, dizziness) and cognitive disorders (for example, memory problems, difficulty concentrating) are indicated (Carpay J., 2005).
These side effects may go unnoticed by the physician, and patients receiving AEDs may be concerned about them despite having complete seizure control.
In addition to the usual dose-dependent CNS side effects, AEDs may have clinically significant metabolic effects. Long-term use of AEDs can cause changes in bone metabolism, resulting in decreased bone density and an increased risk of fractures. Valproate (Depakine, Convulex), carbamazepines (Tegretol, Finlepsin), gabapentin (Neurontin) and pregabalin (Lyrica) may be associated with weight gain sufficient to increase long-term health risks (Sheth R., 2004). Carbamazepines (Tegretol, Finlepsin), phenobarbital and phenytoin are associated with increases in serum total cholesterol, as well as triglycerides, high-density lipoproteins and low-density lipoproteins, although the clinical significance of this phenomenon is not yet known (Nikolaos T., 2004).
Side effects of AEDs increase when polytherapy is used. Monotherapy results in seizure control in most patients, but sometimes fails due to lack of efficacy, dose-related side effects, or idiosyncratic side effects. In patients in whom monotherapy with two or three different drugs has been ineffective, a polytherapeutic regimen may be necessary (Deckers C., 2002). For patients who fail to achieve seizure control with polytherapy, more effective control may be achieved by increasing the dose of one of the drugs, the most effective treatment regimen, and tapering off the other drugs. Often, an adequate dose of one drug is more effective and better tolerated than an inadequate dose of two or three drugs.
Patients who achieve seizure control with combination therapy are also candidates for switching to monotherapy. However, in this case an individual approach is required. The last drug included in the treatment regimen (its prescription in time was associated with the establishment of complete control) may be the drug of choice for monotherapy. This is especially true if the previous drugs or the current combination of drugs were accompanied by side effects. On the other hand, if the patient has achieved drug remission and tolerates a polytherapeutic regimen well, then continuation of this regimen is also a reasonable treatment choice. Although switching from polytherapy to monotherapy is common clinical practice, patients may be reluctant to make the switch due to fear of seizure recurrence. The choice of therapy should always be made with the consent of the patient (Faught E., 2007).
When treating epilepsy with polytherapy, the possibility of switching to monotherapy should be re-evaluated from time to time. Be that as it may, it is quite possible that the only reason to carry out monotherapy is the absence of pharmacokinetic and pharmacodynamic drug interactions (Baulac M., 2003).
Modern treatment of epilepsy is a complex task that requires a lot of knowledge and skills from the doctor in order to select a therapy that is appropriate and most suitable for each individual patient, with lower cost, simpler dosing regimens, less toxic and developed drug interactions. For most patients, tolerability and maximum seizure control are the best criteria for evaluating medications.
For questions regarding literature, please contact the editor.
S. G. Burd, Doctor of Medical Sciences, Associate Professor, O. L. Badalyan, Doctor of Medical Sciences, Associate Professor A. S. Chukanova, G. G. Avakyan
E. V. Krikova, Russian State Medical University, Moscow