Medical information is reliable Checked by Shaidullin Renat Flyurovich
Schizoaffective disorder is an endogenous mental disorder, the symptoms of which simultaneously resemble the symptoms of both schizophrenia and affective psychoses. It is characterized by impaired thinking and unregulated emotions. May include disorganization of speech, hallucinations, and paranoid delusions. The diagnosis of the disease is made based on observation if a person has simultaneously signs of bipolar disorder, depression and schizophrenia, but there are no clear criteria for each of these deviations. The pathology usually manifests itself at a young age and is treated by a psychiatrist.
Causes of schizoaffective disorder
The exact causes of the pathology are unknown, like many other mental disorders, but there are several individual characteristics of the body that increase the likelihood of developing schizoaffective disorder. Most often it is observed in individuals with a hereditary predisposition.
Researchers have identified a risk gene that causes the development of schizophrenia. But under certain conditions, it is in a “dormant state” and begins to manifest itself after exposure to severe stress, severe somatic illness, etc. In addition, the appearance of this gene in the fetus may be due to mutational processes. There is also an assumption of the etiological and pathogenetic similarity of this disease and epilepsy, since in both cases there is a periodicity of manifestations and characteristic changes in the electrical activity of the brain on the EEG.
Provoking factors for the development of schizoaffective disorder can be:
- low social status;
- hunger and poverty;
- hostilities;
- forced migration;
- complete loneliness and lack of help from other people;
- alcohol and drug use.
In the case of the use of psychoactive drugs and alcohol, the possibility of developing this mental disorder increases. At the same time, people with this pathology also often have chemical dependencies, with the help of which they try to get away from their painful sensations, but this only aggravates the process of degradation. To determine what is primary – a mental illness or an addiction to alcohol or drugs, an experienced specialist and monitoring of the patient’s condition in a psychiatric hospital are required.
Dr. Isaev’s clinic has all the conditions for conducting differential diagnosis and providing professional assistance for schizoaffective disorder. For more detailed information, you just need to call the number listed on the website.
For what types of mental disorders is cognitive behavioral therapy indicated?
CBT has proven successful in treating many mental disorders, in particular: • Depression. • Increased anxiety and even its generalized forms. • Panic attacks. • Hypochondria. • Post-traumatic syndrome. • Phobias of various genesis and nature. • Eating disorders and their extreme manifestations in the form of psychogenic anorexia. • Fear of public speaking. • Sociopathic disorders. • Chronic pain. • Psychological problems in the family, athletes, schoolchildren, temporarily isolated persons and other categories of the population, including preschoolers and pensioners. In combination with drug therapy, CBT has proven its effectiveness in treating diseases such as: • Various types of addictions, including alcohol and drug addiction. • Schizophrenia and hallucinations that accompany it. • Severe depressive states. • Bipolar disorder (split personality). • Psychoses. • Somatic disorders – hypertension, colitis, chronic fatigue syndrome, etc.
The scope of CBT is constantly expanding, and the direction itself is gaining more and more popularity. This is explained primarily by its safety for the patient, minimal interference in deep mental processes and its focus on adapting the patient to the changing modern world. The most important thing that CBT allows you to achieve is the ability to maintain your emotional and mental status in any, even the most stressful and seemingly catastrophic situations.
Types of Schizoaffective Disorder
Depending on the predominance of a particular clinical picture, the following types of shazoaffective disorder are distinguished:
- manic;
- depressive;
- mixed;
- unknown etiology;
- other types of deviation.
The manic type is difficult, and the prognosis is often unfavorable. Such a person poses a danger during an exacerbation period and requires placement in a psychiatric ward. The depressive form of the disorder resembles prolonged or moderate clinical depression. In the mixed type, signs of schizophrenia and a picture of affective disorders are noted. Symptoms of schizoaffective disorder begin with the pre-manifest stage, then the attack itself is observed, and after that a remission of varying duration occurs. On average, the acute period lasts for 6-8 months.
Any form of schizoaffective disorder requires timely help. If such a problem has arisen in your family, call us and an experienced specialist will tell you what can be done in this case.
Schizoaffective disorder: symptoms
The first symptoms of this mental disorder are usually observed in adults; children, as a rule, do not suffer from it; the pathology is more often described in women. The first attacks, reminiscent of schizophrenia, alternate with affective manifestations and delusions, while relatively preserved social adaptation and ability to work are observed. Sometimes, at first, emotional disturbances come first, which are replaced by delusions and hallucinations. In some cases, deviations occur simultaneously, and then diagnosis does not cause difficulties.
Schizoaffective disorder refers to transient conditions of an endogenous nature. In this case, disturbances of the emotional type prevail over productive symptoms. The attack is characterized by significant polymorphism of manifestations; its structure includes depressive-paranoid and manic-paranoid types of attack.
The main symptom accompanying schizoaffective disorder is frequent changes in the patient's mood. This happens suddenly, unpredictably and cannot be controlled. After that, attention deficit disorder, hallucinations, and a person’s ability to control their behavior are added to the overall picture. He ceases to understand the difference between reality and his own far-fetched illusions; imagination begins to play the leading role. The disease can manifest itself as pronounced deviations that become noticeable to everyone around, or it can occur in an erased form, when the changes are visible only to those close to you. Typically, schizoaffective disorder is accompanied by the following symptoms:
- depression;
- depression;
- loss of appetite;
- change in body weight;
- addiction to drinking alcohol;
- disturbance of the alternation of sleep and wakefulness;
- lack of interest in what is happening around;
- weakness, loss of strength;
- self-flagellation, decreased self-esteem;
- decreased concentration;
- lack of control over thoughts and actions;
- inadequate emotional reaction;
- suicidal tendencies, thoughts of death;
- strange behavior.
A person with schizoaffective disorder suffers from hallucinations, stops performing simple hygiene procedures, and develops obsessive ideas. The acceleration of thought processes leads to the fact that speech becomes fast, words seem to be layered on top of each other, endings are swallowed.
When the first signs of schizoaffective disorder appear in a loved one, you should not expect the problem to solve itself. The sooner you seek help, the more effective the therapy will be.
In depressive-paranoid types of attacks, the pathology manifests itself in the form of decreased mood and delusions of self-deprecation, ideas of poisoning, destruction, the presence of a fatal incurable disease, and sinfulness. A person suffers from apathy, depression, insomnia. A severe form of the seizure is manifested by depressive oneiroid or stupor. Depressive attacks, if left untreated, can result in the development of addiction or attempted suicide.
The manic form of the attack is accompanied by a decreased need for sleep, unbridled joy, agitation that does not correspond to the situation, and ideas of one’s own importance and greatness. With severe psychosis, delusions of fantastic content and other productive schizophrenia-like symptoms appear. There is a decrease in concentration, increased energy, and inappropriate social behavior due to disinhibition of the nervous system. Clinical manifestations do not appear immediately, but gradually increase in intensity. Sometimes there are ideas of persecution and pronounced aggressiveness, in which a person begins to pose a danger to those around him.
Mixed states represent frequent fluctuations from hypomania and mania to depression. These affects are accompanied by delusions, which contain the theme of the struggle between good and evil with auditory hallucinations of a positive and negative type. They are contradictory and often mutually exclusive in meaning. The mixed type of schizoaffective disorder manifests itself in the form of alternating depressive-paranoid and manic-paranoid disorders (happiness-fear psychosis).
During the period of remission, a person does not have an emotional-volitional defect; after an acute attack, residual symptoms of schizophrenia or affective deviations persist for some time.
Acute polymorphic psychotic disorder
Acute polymorphic psychotic disorder without signs of schizophrenia most often manifests itself in the form of delusions, where the main theme is one’s own greatness, or guilt, the presence of a serious illness, or persecution. Hallucinations and delusions replace each other every day and hour.
There is also a constant change of affects, the mood can be elevated, and after a while it is replaced by severe depression. The symptoms of this disorder are very variable and changeable over time. Thinking and physical activity may slow down or speed up. Anxiety, confusion, and lack of attention are often observed. Distinctive features of polymorphic disorder are:
- constant change in the intensity of manifestation and nature of hallucinations, delusional ideas, mood;
- suddenness of symptoms;
- absence of criteria characteristic of other mental disorders.
Acute polymorphic mental disorder with symptoms of schizophrenia is considered a more severe form of the disorder, it can develop into schizophrenia, and is usually accompanied by the following symptoms:
- delirium of influence of external forces on the patient;
- confidence in your superpowers;
- conviction in reading his thoughts, imposing them from the outside;
- hallucinations with voices that evaluate his actions, talk to each other, laugh at him (Kandinsky-Clerambault syndrome);
- other psychotic manifestations and affective disorders.
These symptoms do not always indicate that a person has developed schizophrenia. If assistance is started in a timely manner, severe mental deviation can be avoided. Otherwise, the patient’s condition worsens, and a schizophrenic personality defect gradually forms. Thus, an acute disorder of this type is diagnosed based on the following signs:
- rapid development of the clinic and abrupt start;
- typical changes characteristic of schizophrenia that last less than a month;
- constantly alternating psychotic and affective disorders (anger, euphoria, anxiety).
Signs of affective disorders
Clinical symptoms of schizoaffective disorder include mood disturbances and schizophrenic features. The degree of their expression is approximately the same, while they alternate or are observed simultaneously. Deviations of an emotional nature are:
- manic;
- depressed;
- agitated.
During mania, a person feels a surge of energy and strength, is always in a great mood, even to the point of euphoria, and is constantly busy doing something. His thinking speeds up greatly and he has difficulty trying to concentrate on a specific job, and problems with concentration arise. His speech becomes fast and incomprehensible due to constant jumping from one topic to another. The patient feels able to “move mountains.”
One of the variants of mania is increased irritability and anger. The person becomes aggressive, behaves rudely with other people, is rude, interrupts, and counteracts. Often this state accompanies the delirium of saving humanity from an alien invasion or another fictitious global problem of the world level.
When depressed, the patient loses his appetite, and sometimes he does not even have the strength to get out of bed. The pace of thinking processes slows down, a person feels melancholy and engages in self-flagellation, and does not find any sources of joy in life. If help is not provided in time, then during this period the likelihood of suicide greatly increases. A subtype of depression is considered to be agitation, when the patient’s sharply depressed mood is masked by active and unproductive activity, which is chaotic in nature.
Signs of schizophrenia
Typical signs of schizophrenia in schizoaffective disorder include:
- delusional ideas;
- hallucinations.
The patient's delirium usually corresponds to his mood. With depression, ideas of one's own worthlessness and uselessness arise. Sometimes hatred appears towards family and friends, as well as towards humanity as a whole. If mania develops, the patient insists on his greatness, considers himself perfect, is confident in his own superpowers, and points to the mission entrusted to him to save the world.
Hallucinations in schizoaffective disorder are usually auditory, but can also be visual or tactile. During an exacerbation, a person sees something that is not really there or hears non-existent voices and sounds. The situation is greatly complicated by concomitant catatonia, usually in the form of stupor.
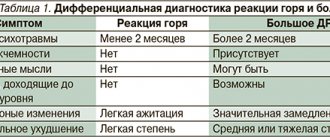
Differential diagnosis of schizoaffective disorder
Since schizoaffective disorder includes symptoms of schizophrenia and manic-depressive psychosis, it is important to distinguish between these diseases. Schizophrenia is a severe chronic mental illness in which remission is difficult to achieve and complete recovery is impossible. It differs from schizoaffective disorder in the absence of a residual defect in the period after an exacerbation. In this case, we mean passivity, apathy, desocialization, flattening of emotions.
The bipolar state is accompanied by mood swings, but does not lead to a decrease in socialization. Its similarities with schizoaffective disorder include the following symptoms:
- episodic manifestation;
- being in a depressed or highly excited state;
- severe anxiety.
The difference is that with schizoaffective disorder, productive symptoms are present simultaneously with affective deviations. Therefore, it is impossible to immediately diagnose this pathology even with knowledge and experience. This is especially difficult if the disease does not immediately develop with signs of schizophrenia and affect during the next exacerbation. It is possible to verify the presence of the disease only after some time, and this requires constant medical supervision.
Experts' forecasts
The main difference between schizophrenia and recurrent schizophrenia is the consequences of recovery from psychosis. In the second case, subject to timely and correct treatment, the patient does not experience a residual schizophrenic defect after an exacerbation. This means that his behavior will lack such manifestations as passivity, apathy, loss of social connections, irreversible emotional flattening (lack of reaction to what is happening).
As a rule, after therapy, the patient may be left with short-term and insignificant phenomena, such as increased fatigue, a feeling of inadequacy, etc. After a short time, they disappear, and the person has the opportunity to return to his previous life.
Despite the favorable prognosis, this does not make this disease easier or less significant. It is strictly contraindicated to refuse treatment or do it yourself. After a course of therapy, the patient must follow the doctor's instructions. At the same time, the patient is prescribed not only drugs that relieve and prevent possible recurrences of schizophrenic symptoms. During this period, the patient also needs to take mood-stabilizing medications.
Schizoaffective disorder: drug treatment
Therapy for schizoaffective disorder at Dr. Isaev’s clinic includes the use of medications to relieve symptoms and psychotherapy. If the patient shows severe aggression during an attack, he is hospitalized until a stable condition is achieved. Taking medications is the main form of assistance for this disease, while working with a psychologist is considered no less important, but auxiliary.
To treat and eliminate negative symptoms, the following are usually prescribed:
- antipsychotics, they eliminate delusions, hallucinations and other symptoms of psychosis;
- anxiolytics for sleep disturbances and severe anxiety;
- antidepressants, which stop low mood, apathy, a feeling of uselessness, the desire for one’s own death, encourage action;
- mood stabilizers to normalize mood in case of low mood or manic disorder;
- sleeping pills that help normalize a good night's rest.
Acute psychosis with this deviation is usually treated with a combination of two or more medications. But it is best for the doctor to select a dose with constant observation, and therefore the person needs to stay in the hospital for some time. After achieving remission, the patient begins outpatient treatment with periodic visits to a psychiatrist. He comes to see him or a specialist is called to his home for a routine inspection.
In our clinic, only proven, certified drugs are used to treat schizoaffective disorder. They give the desired result and at the same time have minimal side effects.
If a person has schizoaffective disorder and dependence on alcohol and psychotropic drugs, then in this case a narcologist is involved in the therapy process, since chemical addictions greatly aggravate the condition and reduce the effectiveness of treatment.
What is the essence of cognitive behavioral therapy?
The essence of CBT cannot be understood without its basic concepts, among which the most important are: • Schemas, which are deep mental attitudes responsible for a person’s attitude towards himself and the realities of life. They can be adaptive and non-adaptive (the whole world is a mess, and there is no point in trying to figure it out), positive and negative, idiosyncratic (individual) or universal. • Automatic thoughts are conclusions that form in the mind so quickly that they do not have time to be fully comprehended, but they manage to influence emotions, the adoption of one decision or another, and the behavioral response of the individual. Usually these are frequently repeated thoughts when communicating with people around you - parents, children, bosses, friends and colleagues. After automation, the brain gets used to not thinking about thoughts, but simply “retrieving” them from memory along with the emotions and action patterns they previously evoked. If the experience of an automatic thought has brought positive results, then it can be useful in making a quick decision, but if the automatic thought was initially incorrect, then following it can only do harm. That is why identifying such thoughts, extracting them from the subconscious and convincing counterargumentation makes it possible to rewrite erroneous mental attitudes and accordingly change behavior patterns. • Cognitive errors, or otherwise distorted thought patterns that incorrectly reflect existing reality. • Arbitrary conclusions are conclusions made without confirmation by facts or in the presence of facts that contradict this conclusion. • Overgeneralization. Occurs when comprehensive conclusions are drawn from a single episode. • Exaggeration and understatement of one's role and the significance of ongoing events. By exaggerating the complexity of the situation, the individual underestimates his capabilities in resolving it. • Personalization - observed when the patient considers certain external events as relevant to him, when in fact they do not concern him at all. • Maximalism - putting forward excessive demands on oneself or the world around us in the form of opposing attitudes. For example, “if I don’t make a million, then I’m a complete insignificance,” “if I don’t become famous, then this life will be a swamp,” etc. • Obligation is an overdeveloped sense of duty and responsibility, often imposed from the outside and not allowing for alternative behavior. It can seriously poison a person’s life and prevent him from self-realization. The psychotherapist faces the difficult task of determining the predominant motive that led to mental disorder and irrational behavior, especially since there may be several of them. The doctor should find out all this and develop a treatment plan already in the first sessions, and the patient’s task is to help him with this. First of all, when preparing for the visit, it is advisable for the patient to think through and formulate the final goals of treatment in advance, i.e. what he would like to achieve and/or get rid of.
Application of psychotherapy
Psychotherapy for patients with such a diagnosis is an auxiliary method of providing assistance; it accelerates the effect that can be achieved by precise selection of medications, consolidates the result, prolongs remission, and adapts the person to a society of healthy people. Talk therapy is often used for schizoaffective disorder. It allows you to better understand your condition, understand your own feelings and reduce their influence, identify negative attitudes that provoke destructive behavior, and replace them with constructive thoughts and actions. For this purpose, cognitive-behavioral techniques are used for individual lessons and work in groups. If the cause of the disease is psychotrauma at a young age, psychodynamic therapy is used.
If the patient is unable to express all his problems, art therapy is of great help. Taking part in art, music, or dance can help you express yourself and cope with current triggers for your attacks. Family therapy plays a leading role in the treatment of schizoaffective disorder, which allows one to influence the home environment. Thanks to the participation of loved ones in the treatment process, they can understand:
- the feelings that the patient experiences;
- what actions on their part help or hinder recovery;
- what needs to be done to make positive changes.
Many relatives behave incorrectly towards a mentally ill person. With their hypertrophied care, they cause or strengthen his feeling of inferiority. Understanding his problem, but at the same time constantly recognizing himself as weak and incompetent, the patient only aggravates his difficult situation. Thanks to family psychotherapy, a person understands how his condition and signs of the disease can affect those who live nearby. After treatment, all family members begin to act together, directing their efforts to eliminate existing difficulties and problems, and work on a strategy to prevent the next exacerbation of the pathology.
A person who has been diagnosed with schizoaffective disorder, if he contacts Dr. Isaev’s clinic in a timely manner, has the opportunity to completely get rid of the manifestations of the disease. Qualified specialists help a person with this diagnosis reduce the number of attacks and increase the time of remission for a long time.
Psychotherapeutic techniques aim to remove not only causative factors, but also reduce the likelihood of stressful effects. Work with a specialist begins after the acute attack has stopped, otherwise the doctor will not be able to achieve full contact and awareness of the problem. In general, the prognosis for this disease is favorable, but the outcome depends on the timeliness of the start of treatment and the characteristics of affective and schizophrenic manifestations.
The use of psychotherapy significantly increases the effectiveness of drug treatment. The specialist’s job is to detect hidden factors that provoke attacks, eliminate them or reduce their impact. A person is aware of the reasons for the development of deviations and understands their destructiveness. Family psychotherapy also plays a significant role, thanks to which mutual understanding between the patient and close relatives improves.
Previously (before 1983) in Russian psychiatry, attacks of a schizoaffective structure were considered as a favorable (undifferentiated) course of paroxysmal-progressive schizophrenia [5]. In ICD-10 [4], adopted for use in the practice of domestic psychiatry, schizoaffective disorder (SAD) is allocated to a separate diagnostic heading - F25, but retains its place in the section “Schizophrenia, schizotypal and delusional disorders” (F2).
Depending on the dominant affect in the structure of the attack, taking into account schizophrenic symptoms, SAD is divided into manic, depressive and mixed types. The depressive type of schizoaffective disorder (F25.1) includes primarily depression with the presence of at least two of the three characteristic (typical) depressive symptoms (low mood, loss of interests and ability to enjoy, severe fatigue, even with little effort - F32) or concomitant behavioral disorders within a depressive episode. Along with severe depression, at least one (preferably two) typical symptom of schizophrenia from the list “a-d” (F.20) must be present. In DSM-IV-TR [15], similarly to ICD-10, a psychotic state with the simultaneous presence of depressive, manic or mixed affective disorder and symptoms of schizophrenia is accepted as the main symptom of SAD. At the same time, in the clinic of schizoaffective disorder of the depressive type, the severity of depression must meet the criteria for a depressive episode. The presence of hallucinations and delusions is recognized as possible (for at least 2 weeks).
The purpose of this study was to study the psychopathological structure of the first manifest attacks of SAD, taking into account the characteristics of the pre-manifest period.
Material and methods
A group of patients of 48 people, 34 women and 14 men, diagnosed with the depressive variant of SAD according to ICD-10 (F25.1) was studied. The larger number of women in the present study was due to the fact that the collection of material was mainly carried out in the women's department of the regional clinical psychiatric hospital No. 1 (although the predominance of women was also noted in the literature [1]).
The criteria for inclusion in the study were the manifest (first) attack of SAD with the presence of depressive symptoms and one or more schizophrenic symptoms from the list “a-d” (F20) with a duration of the psychotic state of at least 1 month. Notable is the fact that the plot of hallucinations and/or delusions corresponds (congruently) to depressive affect in the structure of the attack. The exclusion criteria corresponded to ICD-10 in category F25 with special attention to the presence of delusional symptoms at the pre-manifest stage, including those interspersed with “purely” affective disorders. Patients with productive symptoms without concomitant depressive disorders at the active stage of the attack were also excluded.
The vast majority (89.6%) of patients had secondary specialized or incomplete higher and higher education. Before the manifest attack, 43.8% continued to work, 10.4% were on maternity leave; the number of university students, less often college and school students, was 14.6%; 31.2% stopped working at the pre-manifest stage. Of those employed, the majority worked in the service sector or performed the duties of skilled workers; much less often they were engaged in teaching or entrepreneurial activities, or worked as employees or scientists. 20 (41.6%) patients were married, 5 (10.4%) were divorced, 1 (2.1%) were widowed. More than half (52.1%) had children: one child - 14 patients (29.3%), two - 9 (18.7%), three - 2 (4.1%).
All patients were in the hospital during the examination period. The onset of the manifest depressive variant of SAD in the majority (77.1%) of patients occurred in adulthood (after 20 years), in 22.9% - during adolescence (from 17 to 20 years).
The average age of patients at the time of manifestation of an attack of SAD was 30.5±1.5 years. The duration of the active course of the attack was less than 1 month in 11 (22.9%) patients, 2 months in 16 (33.3%), 3 months in 5 (10.5%) and more than 3 months in 16 (33.3%) ).
A psychopathological analysis of premorbid personality characteristics and pre-manifest manifestations of psychosis was carried out, and the mental status of patients at the time of the attack and the immediate postpsychotic period was assessed. The database consisted of 65 features.
When statistically assessing the results, we used the non-parametric χ2 test with Yates correction (nominal, binary data) [6], Fisher’s test (if the expected frequency is less than 5) [7]. In order to determine the influence of risk factors on the formation of a clinical group, linear discriminant analysis was used. The calculation was carried out using the Statistica 6.0 program (“Stat Soft”).
Results and discussion
Based on a retrospective analysis of the pre-manifest stage of depressive SAD, the vast majority of patients - 79.2% - were diagnosed with affective disorders. Depressive states were
place in 23 (47.9%) patients. It turned out that in these cases, psychogenic provocation was noted quite often - in 16 (69.6%) patients ( p
<0.028). Bipolar disorders developed more rarely than depressive patients at the pre-manifest stage of SAD - in 12 (25.0%) patients, and hypomania, even more rarely - in 3 (6.3%). In the last two cases, the disorders arose autochthonously. According to N.D. Lakosina et al. [3], affective disorders in the form of hypomania or subdepression are detected in 59.6% of patients with SAD.
In this study, there was no dependence of the occurrence of an attack of BAD on the season, although there was a tendency for depressive BAD to develop more often in the fall compared to spring and summer.
Let us draw attention to the fact that the active manifestation of depressive BAD was immediately preceded by provoked or autochthonous affective disorders. Moreover, with a high degree of confidence ( p
<0.0001) the absence of an interval between pre-manifest disorders and the attack predominated, and pre-manifest affective disorders delayed from the manifest attack for a period of 1 month to 1 year or more were significantly less common. The presence of pre-manifest affective disorders indicates premorbid stress vulnerability of some patients with manifest depressive MAD. Attention was also drawn to the fact that there was no seeking medical help at the pre-manifest stage.
In 15 (31.3%) patients at the pre-manifest stage, pathological interests and hobbies were identified in the structure of non-psychotic affective disorders. Their content varied somewhat depending on the valence of the affect. So, in the case of a depressed state, this could be a passion for computer games (online games) and immersion in them, attempts at spiritual self-improvement in the knowledge of philosophical teachings, many hours of listening to hard rock, interest in “health-improving” literature and attending relevant courses. During the period of hypomania, a sudden love arose, including through the Internet, a passion for astrology, palmistry in order to find out one’s future, a craving for artistic creativity (for example, an active performance as a dancer in an erotic bar); attending expensive courses with the goal of “getting to know yourself as a person, learning to make the right decision and avoiding wrong ones, improving relationships with others and loved ones”, intensifying participation in business with the attitude of “making more profit” to the detriment of all other interests, including caring for the family ( “even children are not interested”). The significant frequency (51.2%) of the occurrence of pathological interests and hobbies in SAD (mixed and manic types were studied) has already been noted in the works of domestic authors [8].
Assessment of the severity of depression at the active stage of the course of depressive SAD was carried out from the perspective of ICD-10 criteria (F32-F34)[]. Half of the patients - 25 (52.2%) were diagnosed with an intermediate degree of severity - between severe and moderate depressive episode (DE). The basis for this was the presence in the patient of all three typical symptoms of depression mentioned above and from two to three of its other manifestations from the ICD-10 list; in one observation, a combination of two typical and six additional symptoms of depression was classified as an intermediate degree of severity of DE. In foreign literature [16], there are indications of the possibility of identifying an intermediate (transitional) severity degree of major depression or major DE.
In other cases, patients had mild (16.6%), severe (12.5%) and moderate (8.3%) severity of DE. The presence of subdiagnostic manifestations of DE was noted in 5 (10.4%) cases.
A significant frequency of individual subdiagnostic manifestations of generalized anxiety disorder (GAD) associated with diagnostically delineated depression was revealed. In this case, DSM-IV criteria were used. It was not possible to use the diagnostic rubric for GAD in ICD-10 (F41.1) due to the confusion of the criteria for GAD and non-fabular (floating) anxiety. Such manifestations of GAD as sleep disturbance (83.3%), fatigue (66.6%), and difficulty concentrating (52.1%) overlap with the manifestations of depression itself. The symptom of muscle tension is not typical for patients with the depressive variant of SAD. The accumulation of manifestations of autonomic hyperactivity in patients also turned out to be uncharacteristic. Thus, individual manifestations of vegetative anxiety were noted in 38 patients, and in 16 of them - in the form of one symptom.
At the onset of the attack, a significant place could be occupied by motor excitement (restlessness), when the patient, according to relatives, rushes around the room or spends days in meaningless movement around the apartment. At the height of the attack, psychomotor retardation was clearly manifested, which was accompanied by complaints about thinking disorders: “I can’t quickly formulate a thought,” “thoughts flow slowly,” “it takes me a long time to think.” The patients' voice was quiet, their answers were monosyllabic with long pauses; patients rarely changed their body position during conversation. With such psychomotor slowness, especially at the height of the attack, patients complained of a “sad, melancholy mood”, said that they “have no desires, don’t want anything”, “decreased mood”.
According to the picture of the psychotic attack, patients with manifest depressive SAD could be divided into two groups: 1st - with a monomorphic attack structure - in 14 (29.2%) patients, 2nd - with a polymorphic clinical attack structure - in 34 (70, 8%) patients. The monomorphic clinical structure of the attack in 10 cases was limited to verbal hallucinosis (true or pseudohallucinatory variants), one of the schizophrenic symptoms necessary for diagnosing SAD from the ICD-10 list; in 1 case there was functional verbal hallucinosis, in 3 cases the delusional register of psychotic symptoms predominated (acute sensory delirium or delusional somatopsychic depersonalization syndrome). In the case of the polymorphic structure of manifest depressive SAD, in most cases - in 27 (79.4%) patients, the mental status was determined by verbal hallucinosis - its true and pseudohallucinatory variants (35.3 and 44.1%, respectively); in isolated observations there was verbal functional hallucinosis (2.9%). A feature of the polymorphic structure of the attack is the combination of manifestations of verbal hallucinosis in the form of the main syndrome with the episodic occurrence at the onset and during the active stage of the attack of episodes of acute sensory delirium (delusional mood, symbolic meaning, intermetamorphoses, acute paranoid, delirium of staging), visual-figurative delirium of the imagination, individual manifestations of mental automatism syndrome or delusional episodes with the plot of damage, damage, imaginary pregnancy, confabulatory delusions. Among the optional syndromes, along with verbal hallucinosis, which determines the clinical picture of the attack, episodic occurrence of visual and olfactory hallucinations, hallucinations of the imagination, and in a single observation - visceral hallucinations were identified. Much less frequently (3 patients), the main clinical manifestations of polymorphic structural depressive disorder were determined by the delusional register of disorders. There was a clear syndromological phasing in the formation of delusions of staging, combined manifestations of delusions of corruption with misomania; hypochondriacal delusions with hallucinations of the imagination. In 2 observations, with a polymorphic structure of manifest depressive PAR, there was an oriented oneiroid with the presence of verbal pseudohallucinosis or mental automatism syndrome.
For individual disorders, significant statistical differences were noted between the group of patients with a mono- and polymorphic clinical picture. In group 1 of patients, schizoid (sensitive variant) premorbid personality traits were significantly more common (χ2=4.58, df=1, p
=0.03), stress-provoked affective disorders at the pre-manifest stage (χ2=7.2, df=1,
p
=0.007), while the latter were more often represented by depressive disorder (χ2=5.8, df=1,
p
=0.016) and in the form of a single depressive episode (χ2=7.8, df=1,
p
=0.005).
On the contrary, in patients with a polymorphic attack structure, bipolar affective disorder occurred significantly more often at the pre-manifest stage (χ2 = 3.98, df = 1, p
= 0.046) in the form of dual affective phases (
p
= 0.04).
Features of pre-manifest affective symptoms depending on the monomorphic or polymorphic structure of the manifest depressive mental disorder are presented in Table.
1 and 2 .
Comparative syndromological characteristics of manifest depressive SAD, depending on the mono- or polymorphic structure, are given in Table. 3
.
Let us dwell on some of the features of verbal hallucinosis that occurred in the patients we observed. We are talking about the “symptom of openness” or, rather, the consciousness of the openness of one’s thoughts according to the mechanism of inference [11]. Patients, for example, said: “the neighbors voiced my thoughts - whatever I think about, they already know and answer me” or “the voices of my husband’s relatives behind the wall know my thoughts - I just think about it, and they already tell me in advance what will happen "
Episodes of delusional mood as initial manifestations of delirium of the imagination [11] during a depressive manifest attack of SAD with a polymorphic clinical picture were characterized by a “premonition of bad things,” or the patient “caught” the condemning glances of others on himself—“they don’t look at me like that.” Otherwise, it is a feeling that relatives in the family can harm a child just brought from the maternity hospital; as if “the furnishings in grandma’s apartment have changed: the mirror hangs in a different place than before; The furniture is not placed where it usually is”; upon returning to her apartment, the patient could not recognize the front door - “its shape and color of the door had changed.” Delusions of symbolic meaning in the structure of the polymorphic clinical picture of the manifest depressive variant of SAD, as well as all the types of delusions mentioned above, were an episode.
In most cases, the plot of episodes with visual-figurative delusions of imagination in the clinic of depressive SAD, which was polymorphic in clinical structure, had a dramatic but ordinary content. In the domestic literature [2] there are indications of the possibility of the emergence, along with megalomanic and everyday content, of delusions of imagination. This could be a short-term, transient “feeling of being in a cemetery” (funeral of a mother, daughter-in-law), accompanied by a feeling of cold, wind, while the patient saw trees around her, heard the crying of others, or this “feeling of darkness around her and dead relatives nearby” with a request for close people to turn on the light, otherwise, it’s a feeling of being buried alive - “it’s cold, they’re throwing earth at me” with a request for help from others; drowning - “I feel like I’m dead, I feel water around me, I can’t take a breath - water gets into my mouth”; dying - “it seemed like I was dying, I saw a picture in my head: a corridor with a bright light.” These could be flashes of flame in the evening hours (“fire all around”) with double orientation - the feeling that the patient is on the street and at the same time understands that she is in the apartment. The scale of psychotic experiences in the case of diagnostically outlined visual-figurative delusions of the imagination (oriented oneiroid) included “the expectation of war and disaster”, “the struggle of world powers for human resources, energy and land”; the patient found himself in the center of these events with the need to choose someone's side in the conflict. This could be a reincarnation with the loss of her physical “I”, reincarnation and return to her physical body, while the patient did not completely lose orientation in the environment, for example, she made demands on the medical staff - “do something with me, I have become different."
Episodes of delirium with a plot of damage reflected a pathoplastic family or professional conflict situation, as well as pronounced asthenia as one of the manifestations of depression (“I didn’t do anything, but was already tired after 15 minutes”) and in none of the observations did they exhaust the clinical picture of acute polymorphic in structure depressive schizoaffective attack. The determining factor in these cases was verbal hallucinosis without any continuity in the content of the voices in relation to the delusional plot of damage. Transient ideas of damage arose, for example, in the context of the beginning of the privatization of a house and land (“the neighbors are rearranging pegs, limiting the area of my plot, doing this at night, covering my house with garbage”) and existed with verbal hallucinosis commenting on the patient’s behavior, or arose during emerging from an attack with a complex polymorphic structure (“my son is in cahoots with his sister - they decided to put me in the hospital in order to take possession of the apartment”). The delusion of intermetamorphosis was represented by the phenomenon of a negative double, and it could, as it were, precede the development of an acute attack or be the final one at the exit from it, and also arise in the structure of an episode with the plot of the delusion of a staging. The latter occurred both at the hospital stage and during the stay in the department.
Among our observations there was also a small group - 7 (20.6%) patients with the presence of subcatatonic symptoms in the structure of a polymorphic attack. In this case, transient subcatatonic episodes occurred at the onset of the attack. According to relatives, these were short-term episodes of immobility for several minutes (“freezing”), for example, in one position with a lack of reaction to external stimuli, or episodes of freezing in one position were replaced by motor excitement. Otherwise, these were more extensive episodes in the form of freezing while eating, washing dishes, or holding the lower limb raised and bent at the knee joint in one position. In isolated cases, subcatatonic symptoms were included in the clinical picture of delineated oriented oneiroid. The inclusion of these observations in the category of depressive SAD, from our point of view, was possible due to the distinct depression in the structure of the attack and the correspondence of the content of the visual-figurative delusions of the imagination to the dominant affect.
The general group of patients was also analyzed in relation to the presence or absence of mixed affective disorders at various stages of the attack. These types of attacks occurred in 25 (52.1%) and 23 (47.9%) patients, respectively. In 4 cases, there was a sudden replacement of the depressive component of psychosis by an episode of elevated mood with possible appropriate and productive activity. Thus, one patient began to actively participate in the preparation and holding of a charity evening for several days in order to raise money for an orphanage; another - for several days, experiencing “euphoria”, became active in everyday life, expressed a desire to relax at the dacha; in the third case, a depressive state was observed in the morning and during the day, which in the evening was replaced by mild hypomenia with the need for vigorous activity (“general cleaning of the apartment”), which corresponds to the concept of “conditional bipolarity” [10]. In the fourth case, the patient, according to relatives, for a short time became smiling, cheerful, and tried to hum and dance to the music. In a larger number of observations (9), hypomania (including the type of conditioned bipolarity) occurred at the end of an attack, immediately after the reduction of depressive and productive symptoms. Moreover, in 4 patients, after recovery from an attack or in the immediate post-psychotic period, bipolar affective disorders were noted. Along with mixed affective disorders in the form of a bipolar variant, the presence of mixed affective symptoms proper was revealed. This was mixed depression [12-14] at the height of the attack or mixed depression at the height of the attack and an alternating variant [9] at the stage of reduction of depressive and productive symptoms (2 observations), an alternating variant at the onset of an attack (1 case) and at the end of it (3 patients), but without concomitant productive symptoms.
In order to confirm the validity of identifying the typology of manifest depressive disorder based on the criterion of the absence or presence of mixed affective disorders in the structure, a linear discriminant analysis procedure was applied with the sequential inclusion and exclusion of features included in the main database. Of the 65 signs, 13 of the most informative ones were identified, allowing one to differentiate the two above-mentioned clinical groups. These signs include manifest schizophrenia in first-degree relatives, the number of mentally healthy relatives; verbal pseudohallucinosis throughout the attack; premorbid features in the form of avoidant (anxious) personality disorder; a number of socio-demographic indicators (presence of children, professional employment, fact of leaving work at the pre-manifest stage); bipolar and depressive disorders at the pre-manifest stage (autochthonous and provoked occurrence), etc. The greatest contribution to the division of clinical groups according to the criterion of the absence or presence of mixed affective disorders is made by the sign “verbal pseudohallucinosis” in the structure of the manifest manifestation of depressive BAD. The quality of discriminant analysis (Wilks' Lambda value was 0.29, F (13.34) = 6.23, p
<0.00001) indicates the correctness of the undertaken separation of patients.
In the clinical structure of the polymorphic depressive variant of SAD with the presence of mixed affective disorders, a number of features of verbal pseudohallucinosis were noted. This refers primarily to its dominance in the psychopathological space of the attack. This refers to the duration of pseudohallucinosis at the active stage of the attack, detailed plot development and systematization of delirium, congruent with the content of auditory hallucinations. Manifestations of verbal pseudohallucinosis may be accompanied by visual pseudohallucinations during a significant period of active psychosis. So, for example, one of the patients has images of influential political, military and religious figures of the past in her head - “I see and hear them in my head, I talk to the images”; Subsequently, the content of pseudohallucinosis acquires a megalomaniac connotation - “the patient must give birth to 16 girls” and at the same time, in accordance with the content of the voices, do not forget to “brush your teeth and wash your face.” In the case of religious and mystical content of auditory hallucinations (voices) or close to megalomaniac content, patients obey their imperative content - “cast out evil spirits, demons from loved ones” by sprinkling with holy water, bringing the icon closer to the face; ready to sacrifice domestic animals; one of the patients, obeying the imperative content of the voices, could hit someone close to her, took a bath in her underwear, broke a telephone, a TV, and ruined a family portrait.
Summarizing the analysis of a non-selected contingent of patients with manifest depressive BD, carried out in everyday psychiatric practice, we can identify a number of options for the structure of attacks: mono- and polymorphic attacks depending on the number of productive (psychotic) symptoms, with the presence or absence of mixed affective symptoms in the form of hypomania , bipolar disorder, mixed depression and an alternating version of mixed affective disorder (without concomitant productive symptoms). Pre-manifest affective disorders were also noted. At the same time, in 47.8% of patients with mixed affective disorders in the structure of manifest depressive MAD, bipolar disorders or isolated episodes of hypomania were detected at the pre-manifest stage. This gives reason to assume that for a certain part of patients with manifest depressive SAD, the tendency towards bipolarity, inherent in the pre-manifest stage, finds its expression at various stages of the course of the attack itself.
[]In the literature [17], a psychometric assessment (PHQ-9 questionnaire) was also used for this purpose.
Questions and answers
Can schizoaffective disorder be completely cured?
With a mild form of the pathology, stable remission can be achieved for many years. Properly selected therapy can stop their manifestations even with severe attacks and preserve the person’s ability to work. In general, the prognosis in each specific case is individual and depends on many factors.
Is it possible to identify schizoaffective disorder in a loved one?
The symptoms of this disease are very similar to other mental disorders, so only an experienced doctor can make a diagnosis. To do this, it is best to hospitalize the patient and observe him over time.
Etiology of the disease
Despite many studies in the field of mental disorders, the cause of the development of schizoaffective psychosis is still not clear. It is believed that hereditary predisposition plays an important role - people whose immediate relatives suffered from schizophrenia are at risk.
The characteristics of a person’s character, his reaction to stress, and problematic life situations also matter. In addition, experts note that the disease is more often diagnosed in women.