Tranquilizers are a group of psychotropic drugs with an anti-anxiety effect, relieving anxiety and internal tension, anxiety, tremors and muscle tension of neurotic origin, and a feeling of fear. Some drugs in this group, in addition to their normalizing psycho-emotional state and nighttime sleep effect, can have a tonic effect.
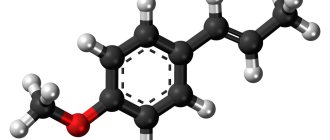
Among tranquilizers (from the Latin tranquillo - to calm down) there are typical and atypical ones, which do not have pronounced non-core effects and do not cause dependence when taken for a long time. Based on their chemical structure, anxiolytics are divided into benzodiazepine derivatives (chlordiazepoxide, diazepam, phenazepam, oxazepam, medazepam, midazolam) and drugs of other chemical groups (meprotane, benactizine, phenibut, mebicar, benzoclidine).
The pharmacodynamic activity of all anxiolytics comes down to five main components: sedative, anti-anxiety, hypnotic, relaxant and anticonvulsant. Each specific drug has its own degree of severity of a particular therapeutic effect, which determines its clinical use (for example, in psychiatry, neurology, cardiology, gastroenterology, otolaryngology, anesthesiology).
Anxiolytics are prescribed to relieve states of agitation (1) and asthenia (2) accompanying various mental disorders:
- anxiety, panic, fear, irritability, dysphoria, problems with going to bed, decreased sleep duration, autonomic lability, autonomic crises;
- asthenia, chronic fatigue, hypochondria, problems with attention and remembering information, decreased intellectual activity, weakness, fatigue, lethargy, apathy, irritability, lack of vigor after sleep.
As a rule, the above conditions occur against the background of the following mental disorders:
- neuroses and neurosis-like conditions (F40–F48);
- behavioral disorders in children and adolescents (F91);
- personality disorders (F60–F69);
- fears and phobias (F40);
- insomnia (F51);
- panic attacks (F41);
- generalized anxiety disorder (F41.1);
- mixed anxiety and depressive disorder (F41.2);
- schizotypal disorder (F21);
- acute psychoses (F23, tranquilizers are prescribed as part of complex therapy);
- anorexia (F50.0–F50.1 and bulimia (F50.2);
- psychosomatic diseases (F04–07; F44.4–F44.7; F45; F50–F53).
In the practice of a neurologist, tranquilizers can be prescribed, for example, when states of agitation and asthenia occur due to traumatic brain injuries, strokes accompanied by increased muscle tone, epilepsy, and spinal osteochondrosis. Other somatic doctors prescribe anxiolytics for the treatment of functional disorders in the gastrointestinal tract (gastroenterologist), cardiovascular system (cardiologist), urinary system (gynecologist, urologist), withdrawal states and consequences of organic damage to the central nervous system (narcologist, toxicologist).
Carbamazepine
It is effective against all symptoms when withdrawing from binge drinking and can be the drug of choice when interrupting mild to moderate binge drinking. The lack of interaction with alcohol allows the drug to be used even if it is present in the blood. It has been established that Carbamazepine affects the neuronal transmission of GABA, glutamate, norepinephrine, acetylcholine and dopamine. Monotherapy with carbamazepine is effective for mild to moderate withdrawal syndrome; for severe withdrawal, benzodiazepines are recommended. The undoubted advantage of carbamazepine is the absence of a euphoric effect and the risk of dependence on the drug.
Basics of treatment of neuroses
In psychiatry, tranquilizers are used for anxiety disorders, anxiety disorder with panic attacks, phobias, and to relieve stress-induced mental reactions, such as grief.
Tranquilizers are used occasionally, mainly to relieve episodes of panic or when anxiety increases to a degree that disrupts the patient's behavior.
To reduce the risk of developing addiction, tranquilizers should be used in short courses (from two weeks to a month). If it is impossible to complete treatment after 4 weeks, it is recommended to take short breaks of 2-3 days during the week. Thus, anxiolytics can be used quite safely for up to several months.
Usually the drugs are used in the evening, before bedtime, given the hypnotic effect of most tranquilizers. The exception is “daytime” tranquilizers (gidazepam), which can be used at any time of the day.
Proprothene-100
To date, the most studied of the antibody drugs is Proproten-100, which contains potentiated antibodies to the brain-specific protein S-100 (AS-100). The drug Proproten has been studied at all levels of organization of neuronal structures: cellular, intercellular (synaptic), structural, systemic. The most specific of the studied effects can be considered the sensitizing effect of AS-100 on the cell membrane of neurons. The unusual biological effect at the clinical level is manifested by a balanced effect on the mental status of patients. Depending on the initial condition of the patients, the drug has both a sedative and a stimulating effect.
Sensitizing agents
They are used in coding against alcoholism to create a so-called chemical barrier that makes it impossible to drink alcohol, and to develop in the patient a sense of fear of the possible unpleasant consequences of drinking alcohol. The most common sensitizing agent used in the treatment of alcohol dependence is teturam (Antabuse, disulfiram). The previously widely prescribed sensitizing drugs metronidazole, furazolidone, and nicotinic acid are now rarely used. Disulfiram has been used to treat alcohol dependence since the 1940s. It is assumed that the therapeutic effects of Teturam are due to the fear of Teturam Alcohol Reaction (TAR). The mechanism of action of this drug is based on blocking the enzyme acetaldehyde dehydrogenase, as a result of which the oxidation of alcohol is delayed at the acetaldehyde stage. Before treatment with Teturam, the patient is warned about the possible adverse effects of drinking alcohol.
The drug Disulfiram for coding against alcohol dependence, valid for up to 1 year:
Currently, a fairly common method of treatment is intramuscular implantation of the drug Esperal, which is produced in sealed ampoules containing 10 tablets of 0.1 g of teturam. As a rule, this method is used when other therapeutic measures are unsuccessful. The patient and his relatives are explained that the drug implanted into the tissue will be constantly absorbed into the blood, and if the patient drinks even a small amount of alcohol, he will experience serious consequences, including death.
The use of Teturam has many contraindications due to the pronounced toxicity of the drug. Against the background of its use, various side effects often develop in the form of allergic reactions, toxic hepatitis, and teturama psychosis. Disulfiram may worsen symptoms of schizophrenia. A necessary condition for treatment is the patient’s good health, high motivation, and regularity of taking the drug. It should be especially noted that it is inadmissible to prescribe disulfiram without the patient’s knowledge (for example, adding it to food) due to the danger of the consequences of a teturam-alcohol reaction.
Herbs and fees
It should be noted that there are a fairly large number of folk remedies that can be used for heavy drinking. Some of the herbal medicines in the form of special filter bags are sold in modern pharmacies. These include:
- Stopped. The composition includes a large number of herbs: tansy, centaury, thyme, wormwood and others. They can improve digestion, choleretic processes, psycho-emotional background, and also significantly reduce the craving for drinking alcohol.
- Aralia tincture. Helps restore adrenal function and strengthen the nervous system.
All of them are sold without a prescription.
Need some advice?
OR CALL A DOCTOR
CALL!
+7
Opioid receptor blockers
Advances in the study of the neurochemical mechanisms of alcohol dependence have made it possible to propose a number of new medications for its treatment. Thus, it was found that there is an endogenous opioid system in the brain, which produces morphine-like compounds (enkephalins and endorphins) that cause euphoria and analgesic effects. Drugs that are opioid antagonists block opioid receptors and thus prevent the pleasurable effects caused by drug use. Although alcohol is not an olioid receptor agonist, many of its effects are mediated through the endogenous opioid system. Experiments have shown that opioid receptor antagonists block the reinforcing effects of alcohol. Thus, naltrexone prevented the increase in dopamine levels caused by alcohol administration, and this effect was dose-dependent. Dopamine is known to be involved in the reinforcing effects of alcohol. The duration of remission in patients taking naltrexone as maintenance treatment was longer than in patients taking placebo. It should be kept in mind that naltrexone is effective as an anti-relapse drug if taken regularly over a 12-week course. Naltrexone is especially recommended for patients with strong, uncontrollable cravings for alcohol (compulsive behavior). At the same time, treatment with the drug requires high motivation. The effectiveness of treatment increases significantly in combination with supportive psychotherapy. The drug nalmefene is structurally similar to naltrexone. Unlike naltrexone, it is not hepatotoxic. In addition, nalmefene is a universal opioid receptor antagonist that blocks three types of opioid receptors.
Acamprosate (acetylhomotaurine). To date, the exact mechanism of action of the drug has not been established. It is known to modulate the activity of glutamate and GABA receptors. Chronic alcohol intoxication leads to a decrease in the activity of the inhibitory GABAergic system and an increase in the activity of the excitatory glutamate system in the brain. These disorders persist for a long time after stopping drinking alcohol. Acamprosate is structurally similar to GABA and increases the activity of the GABAergic system, increasing the number of GABA binding sites on the synoptic membrane. Acamprosate reduces the activity of the glutamate system by affecting N-methyl-D-aspartate (NMDA) receptors and calcium channels. Acamprosate was first used in clinical practice in France in 1989. Currently, the drug is approved in more than 30 countries; the total number of patients who have undergone treatment exceeds 1 million. Experiments have shown that acamprosate reduces alcohol consumption in conditions of free access, without affecting eating behavior, has no narcotic potential and has no other pharmacological effects other than those that help reduce alcohol consumption.
Psychotropic substances prohibited in Russia
In Russia, the group of prohibited substances includes the following:
- Ephedrine is a raw material for the production of amphetamines. The substance is produced from coniferous trees.
- Delta-9-Tetrahydrocannabinol (THC), isolated from hemp. In the USA and European countries, the drug is approved for relieving side effects of radiation therapy, in the treatment of AIDS, etc. The drugs Nabilone and Nabiximols have been developed on its basis.
- Dimethyltryptamine is isolated from the Mimosa legume plant grown in Brazil. A psychedelic that causes an altered state of consciousness is more often used in religious or psychedelic practices.
- Morphine, extracted from the opium poppy, was used as an anesthetic.
- Codeine is an opium alkaloid. In a number of countries it is used as an analgesic and antitussive.
- DMT (dimethyltryptamine) (from plants Mimosa hostilis, Psychotria viridis, etc.).
- Kavain is produced from intoxicating pepper. The name of the plant itself indicates the effect it has. – the substance relieves tension, anesthetizes, and causes mild euphoria.
This list contains addictive substances, which is why they are prohibited in Russia. Not all psychotropic drugs are narcotic, that is, addictive. But all narcotic substances are psychotropic to one degree or another. Drug addiction treatment is the first step towards getting rid of this harmful addiction, which must necessarily be followed by a period of rehabilitation. In order to get advice or find out information of interest, call the hotline number indicated at the top of the page or write to us via chat.
Serotonergic agents
The relationship between serotonin and alcohol is complex. It is assumed that alcoholics try to use alcohol to normalize low basal levels of serotonin in the brain. Serotonin has been found to be involved in the reinforcing effects of alcohol. In addition, low serotonin levels contribute to impulsive behavior that leads to alcohol consumption. Abnormalities in serotonin metabolism may be accompanied by anxiety and depression, in which case alcohol may be used as a means of self-medication. Serotonergic drugs include the serotonin reuptake inhibitors (SSRIs) sertraline (Zoloft), fluoxetine (Prozac), fluvoxamine (Fevarin), citalopram. This class of drugs was developed in the 1980s to treat depressive disorders. The mechanism of action of SSRIs is to block the reuptake of serotonin by presynaptic endings, as a result of which the level of serotonin in the synaptic cleft increases.
Other medicines
The use of doxepin recommended by some authors when withdrawing from binge drinking is considered unacceptable due to the high risk of complications - arterial hypotension, arrhythmias and toxic delirium. The administration of phenothiazine neuroleptics (aminazine and tizercin) practiced by some doctors when withdrawing from binge drinking should be considered unacceptable, because These drugs increase the likelihood of developing delirium, seizures and have a proarrhythmic effect. It is known that after the introduction of phenothiazine antipsychotics into practice for the treatment of delirium in the 50s. mortality from it increased 4 times. The co-administration of barbiturates and tranquilizers should be avoided when withdrawing from binge drinking due to excessive sedation and the combination of β-blockers and clonidine due to the risk of developing arrhythmias. A fairly common mistake when withdrawing from binge drinking is forced diuresis. From a pathophysiological point of view, this is not justified in any way, because The cause of withdrawal syndrome is the reaction of neurotransmitter systems to a drop in the concentration of alcohol in the blood, and not ethanol metabolites circulating in the blood. Accelerated elimination of alcohol during withdrawal from binge drinking at home leads to an increased risk of developing seizures and delirium. Infusion therapy with polyionic solutions is indicated for patients with severe dehydration or persistent vomiting. In most cases, oral rehydration is sufficient for recovery from binge drinking.
Serotonin tranquilizer
The drug from the second subgroup is a serotonin receptor agonist - Buspirone or Spitomin. It is able to bind to serotonin and dopamine receptors. The main effect, like that of benzodiazepine tranquilizers, is anxiolytic.
It develops more slowly, over two weeks. Buspirone does not have sedative, hypnotic and muscle relaxant effects.
In the body, the drug also binds to plasma proteins. All its metabolism occurs in the liver, and the substance is released in the form of metabolites through the kidneys.
Indicated for the treatment of various anxiety conditions and neuroses. Contraindications to taking the drug include conditions such as pregnancy and breastfeeding, severe pathology of the heart, liver and kidneys.
The initial dose for treatment is 15 mg per day, divided into three doses. If necessary, the dose can be increased to 25 mg.