Similarities with psychopathy
Clinical manifestations of psychopathic-like disorder may resemble other diseases on the psychiatric spectrum.
However, there are no severe disturbances in the form of hallucinations or delusional syndrome. Often, parents of sick teenagers consider behavioral changes to be part of puberty. That is, the resulting pathology cannot be considered schizophrenia in the classical version, which was observed in the USSR. In 1997, the International Classification of Diseases, 10th revision, included it in section F21 “Schizotypal disorder” under code F21.4.
Forms
The list of symptoms above shows that psychopathic-like schizophrenia is not easily differentiated from other disorders and conditions that may not be associated with psychopathic disorders. To make the diagnosis easier, doctors have identified 4 forms of pseudopsychopathic schizophrenia. They are called syndromes - hysterical, increasing schizoidization, epileptoid and unstable behavior.
Hysteroid syndrome
The hysteroid form is more often detected in women who previously had hysteroid character accentuation. Typically, such individuals crave to be the center of attention. They are characterized by egocentrism, fear of being in an awkward situation, demonstrative behavior, etc. With the development of schizophrenia, the following signs are observed:
- theatricality;
- pretentiousness;
- tendency to lie;
- antics;
- coldness towards loved ones;
- selfishness;
- sudden mood swings;
- ridiculous statements;
- cruelty.
These symptoms become especially noticeable against the background of complete well-being. They inevitably become the cause of conflicts with others, including loved ones who do not understand how to further interact with the person.
In boys, hysteroid syndrome with psychopathic schizophrenia is observed only in 5% of cases.
Hysterical behavior becomes stereotypical. The patient often plays a role without noticing that everyone is laughing at him.
Increasing schizoidization syndrome
The schizoid type of disorder is characterized by such symptoms as:
- isolation;
- interruption of social contacts;
- emotionlessness;
- skipping school or work;
- unusual hobbies;
- pretentiousness of behavior and appearance.
The patient becomes embittered. He criticizes everything and wants to abstract himself from society; he develops strange hobbies, such as picking up animal excrement or fingernails. He may watch the same movie all day long or do unusual physical exercises. If they make comments to him or prevent him from behaving in this way, he snaps. At the same time, the patient may not even understand the topic that he is passionate about.
Such teenagers often run away from home, without any conflict with their relatives. An exemplary student may suddenly start drinking alcohol or become addicted to smoking. However, alcoholism and drug addiction rarely develop with this syndrome.
Epileptoid syndrome
This form of psychopathic schizophrenia is the most dangerous for others, since its typical symptom is outbursts of aggression. Main features:
- coldness and cruelty;
- sudden outbursts of anger;
- loss of disgust;
- unmotivated attacks on people and animals;
- eating inedible objects;
- sexual disorders;
- tendency towards hypochondria.
Such patients are very suspicious. They do not trust either his relatives or the doctor who is treating him, which significantly complicates his treatment.
The patient is very cruel, and the cruelty is savage, terrible and absurd. He either cannot explain the reason for his action, or gives stupid arguments.
It is worth noting that this syndrome is not characterized by boiling anger leading to an explosion. The patient is embittered almost constantly.
Unstable behavior syndrome
Unstable behavior in pseudopsychopathic schizophrenia is also more common in men, and is characterized by the following symptoms:
- inactivity;
- alcohol and drug abuse;
- sexual behavior disorders;
- indifference to friends and relatives;
- constant protests are usually illogical.
The syndrome of unstable behavior is similar to the hebephrenic form of schizophrenia and heboid syndrome, but no serious personality destruction is observed. Often, such patients, especially teenagers, are at home less often, associate with antisocial people, drink, smoke and commit crimes, including sexual ones. At the same time, emotional detachment and disinterest can be traced in all their actions.
Sexual deviations are especially unusual in this syndrome. They are not limited to the typical signs that are characteristic of other psychopathy - transient homosexuality, promiscuity and early sexual activity. A teenager with unstable behavior syndrome may call on his own mother for intimacy and cohabitation.
Diagnostics
To make a correct diagnosis, the doctor conducts a full examination. If the person is a minor, then in the presence of a guardian. Parents of the patient usually seek help when they begin to notice sudden changes in personality and behavior.
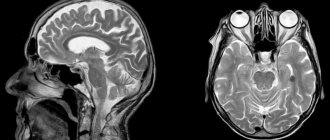
In addition to identifying diagnostic criteria, the following examinations are carried out:
- Collection of complaints, including from others.
- Anamnesis - from deep childhood to the present moment; it is often necessary to clarify information about the parents (burdened heredity).
- Physical examination to exclude significant signs of damage to internal organs and the central nervous system. You should also make sure there are no injection marks.
- Experimental psychological examination.
- Additionally, standard clinical and laboratory diagnostics are carried out: general blood and urine tests, indicators of changes in liver activity, electrocardiography (ECG), electroencephalography (EEG).
If necessary, the patient is consulted by related specialists to exclude other causes of symptoms. In the future, comprehensive assistance may be needed in the presence of concomitant somatic diseases. Instrumental examinations are not usually carried out.
Signs
The clinical picture is determined by the form of development of psychopathic schizophrenia. The set of symptoms may be different, but typical signs can still be identified. These include:
- cruelty, unmotivated aggression;
- the appearance of strange hobbies;
- antisocial behavior;
- breaking contacts with family and friends;
- loss of interest in favorite activities;
- poor relationship with parents;
- isolation, desire for loneliness;
- grandiose ideas of religious or philosophical content;
- tendency to use alcohol and drugs.
The listed symptoms can hardly be called specific. They may indicate a bad upbringing, a difficult character, the influence of antisocial personalities on a person, etc.
However, with the development of pseudopsychopathic schizophrenia, such changes in behavior are striking, since before this the person was completely different. He can grow up in a prosperous family, study well and play sports, but at some point he begins to change for the worse for no apparent reason. In such cases, they usually say that the person “seems to have been replaced.”
Treatment
The approach to treatment depends on the severity of the disorder. First of all, the current exacerbation is stopped until the patient’s condition is completely stabilized. Next, a rehabilitation program necessary for the person’s painless return to society is selected on an individual basis.
The most optimal is a combination of pharmacological effects and psychotherapy. Drugs are selected individually, taking into account the dominant symptoms and tolerability of the active substances. The following groups of medications are used to relieve psychopathy:
- neuroleptics – eliminate severe behavioral disorders;
- mood stabilizers – stabilize mood and psycho-emotional background;
- tranquilizers – quickly relieve anxiety and tension;
- antidepressants - in the presence of concomitant symptoms, as well as monitoring of remission;
- drugs for symptomatic therapy in the presence of concomitant diseases.
In mild cases, outpatient management of patients (at home) with a mandatory visit to a psychotherapist is permissible. The ineffectiveness of the measures taken is an indication for hospitalization in a hospital, where the treatment regimen will be adjusted. Such patients are not restricted in their movements around the hospital premises.
The most effective psychotherapeutic direction is cognitive behavioral therapy. Family and group sessions are also organized for adolescent patients. During treatment, other techniques may be used (play, art/zoo therapy, occupational therapy).
Suicide
Suicidal tendencies in psychopathic schizophrenia are observed in 41% of patients. In this case we are talking primarily about teenagers. But often everything is limited by thoughts. No action is taken. Moreover, many patients do not even tell anyone about them at the moment they appear in their heads. They find out about this later, when the attack passes and the teenager shares his thoughts with doctors.
Patients say that they are visited by the idea of entrusting their fate to chance, to fate. For example, a teenager is standing at a metro station waiting for a train. Suddenly the idea comes to his mind to throw himself under the rails, but at the same time he decides that he will do this only if there is an even number on the scoreboard.
Sometimes suicidal feelings are combined with harshness towards oneself, which is meaningless. The patient can completely undress and lie down in a snowdrift to freeze, or put something heavy on his throat, etc. Often such attempts to die are thwarted by relatives or those who happen to be nearby.
Forecast
It is important for parents to understand that the cause of a teenager’s antisocial behavior is illness, and not alcohol or “bad company.” With timely consultation with a doctor, pseudopsychopathic schizophrenia can be successfully treated with the help of pharmaceuticals and psychotherapeutic consultations.
Despite the chronic course, the prognosis is favorable. After achieving stable remission, a person returns to a normal standard of living, no different from other members of society. When the first signs of exacerbation appear, you just need to contact your doctor, who will help prevent the symptoms from worsening.
Approximately 40% of patients experience suicidal behavior, thoughts about which they keep to themselves for a long time. Attempts to accomplish what is planned usually end in failure, but the risk of self-harm is high, especially during demonstrative behavior. Therefore, it is important to monitor the person’s activities more closely until stable remission is achieved.
Risk factors
The causes of schizophrenia remain unknown to science. Its psychopathic form is no exception. We can only say that it is an endogenous disorder. However, doctors still identify a number of factors that contribute to the development of pseudopsychopathic schizophrenia. Among them:
- disruption of the functioning of neurotransmitters in the central nervous system;
- brain damage - organic or intoxication;
- hereditary conditioning;
- genetic mutations.
The disorder is most often diagnosed in teenage boys. But the exact risk groups are difficult to determine due to the lack of understanding of the mechanism of disease formation. Scientists only note that there is no connection with family relationships and upbringing.
Bibliography:
- Lichko A.E. ‹‹Schizophrenia in adolescents››. Psychopathic-like form of sluggish schizophrenia.
- Lichko A.E. ‹‹Psychopathy and character accentuations in adolescents››. Psychopathic-like form of sluggish schizophrenia.
- Drobizhev Mikhail Yuryevich, Kalinina Elena Valerievna, AntokhinEvgeniy Yuryevich, Sorokina Ekaterina Yuryevna PRACTICE OF APPLYING ANTIPSYCHOTICS AND CORRECTORS IN PSYCHIATRY. First results of the ANCORPSI program (ANTipsychotics and CORRECTORS in PSYCHIATRY) // Social and clinical psychiatry. 2015. No. 2.
Clinical case
The disease manifested itself 5 years ago. During this period, the patient was hospitalized in a psychiatric hospital twice. Each time - for 1-2 months. Before this, he demonstrated inappropriate behavior, annoyed people with conversations about the meaning of life, shirked work, said that he was writing a book and plans to change the world. He was constantly in conflict with his relatives, and in the hospital he was florid and showed exaggerated swagger.
Hallucinations and delusions are absent in psychopathic schizophrenia, which distinguishes it from other forms of schizophrenic disorders.
After treatment with pills, he became collected. He could work in low-skilled jobs, but had a penchant for alcohol, believing that alcohol helps to gain inner freedom and looseness. The likelihood of relapse remained high.