Sometimes, due to a variety of reasons, numbness in certain parts of the body may occur.
If this happened once, for example, as a result of an uncomfortable position in a dream, then there is nothing wrong with it.
But if loss of sensitivity occurs quite often and lasts a long time, then this is an alarming symptom that requires immediate medical intervention.
Hypesthesia is a dulling of sensations , a weakening of sensitivity in certain parts of the body, as a result of which a person loses the ability to adequately perceive the action of external stimuli, as well as respond to changes occurring in his body.
This is due to a disruption in the functioning of human nerve endings. Often the disease can appear during pregnancy, and after childbirth it disappears on its own.
The disease manifests itself as follows:
- a person does not feel anything when he touches objects;
- he feels the pain dulled, even if it is quite strong;
- cannot determine temperature differences;
- If the vagus nerve is damaged, hearing may be impaired.
Often the disease makes itself felt when metabolic processes are disrupted, resulting in fluid accumulation in the fingers and hands.
Hepatic encephalopathy - causes and symptoms, treatment methods, prognosis and prevention of the disease.
How does brain astrocytoma, whose life prognosis is extremely unfavorable, stand out from other brain tumors? Is there a chance of salvation?
Surgical treatment of obliterating diseases of the lower extremities
Surgical treatment is prescribed to patients who can safely undergo major vascular intervention and whose severe symptoms do not respond to atraumatic treatment methods.
The goal is to reduce symptoms, cure the ulcer, and prevent amputation. Since many patients suffer from concomitant coronary artery disease, in light of the danger of acute coronary syndrome, they fall into the high-risk category of surgical treatment, therefore, the functional state of the patient’s heart is usually assessed before surgery. Thromboendarterectomy (surgical removal of an obstructing object) is performed for short, limited lesions in the aorta, iliac, common femoral, or deep femoral arteries.
Revascularization (eg, femoropopliteal anastomosis) using synthetic or natural (often saphenous vein or other vein) materials is used to bypass occluded segments. Revascularization helps prevent limb amputation and reduces lameness.
- Causes of hypoesthesia
- Symptoms of obliterating diseases of the lower extremities
- Mental changes. Nervous exhaustion. Asthenia. Depression. Psychosis
- Causes
- Types of hypoesthesia
- Numbness and decreased sensitivity
- What causes numbness in the fingertips?
- Prevention
- 3 Carpal tunnel syndrome
- How to prevent the problem
- 5. Psychotherapy
- Causes of hyperacusis
- Symptoms of mental hyperesthesia
- Etiology and pathogenesis
- Causes of development and treatment of hypoesthesia
In patients unable to undergo major surgery, sympathectomy may be effective when distal occlusion causes severe ischemic pain. Chemical sympathetic blockade is similar in effectiveness to surgical sympathectomy, so the latter is rarely performed.
Amputation is a last resort prescribed for intractable infection, intractable pain at rest and progressive gangrene. The amputation should be as distal as possible, sparing the knee for optimal use of the prosthesis.
Causes of hypoesthesia
https://www.youtube.com/watch?v=ytadvertiseru
Hypoesthesia is a disease that does not occur just like that. Therefore, most likely such abnormalities in the body indicate a more serious illness. Let's look at what diseases can be preceded by hypoesthesia:
- Problems with blood circulation.
- Formation of a malignant tumor in any organ.
- Diabetes mellitus, which lasts for several years.
- Headache.
- Lack of vitamins.
- Neglect of a healthy lifestyle and abuse of bad habits.
- Pinched nerve.
- Pathologies that arise at the genetic level.
Naturally, these are not all diseases, but they most often lead to numbness of the limbs and changes in the body.
Hypesthesia often appears in people who lead a sedentary lifestyle or perform monotonous, repetitive work. This pathology also accompanies diabetes mellitus, which affects the body's metabolic processes.
A common cause of the disease is insufficient concentration of B vitamins in the human blood. Such hypoesthesia is accompanied by increased irritability of the patient, frequent dizziness, fainting and improper functioning of the digestive system.
Loss of sensation in the scalp can occur due to improper functioning of the cardiovascular and nervous systems.
In addition, migraines, head injuries, coronary heart disease, alcoholism, and heredity can be factors that provoke the appearance of numbness.
In addition to the reasons listed above, hypoesthesia can be caused by rheumatoid arthritis. The nerve is pinched by the deformed joint, causing the well-known numbness.
These symptoms require immediate diagnosis in a medical facility and the prescription of drug therapy.
What is the essence of the disease?
Hypoesthesia is any disorder that is associated with sensitivity. As a result, a person stops responding to external stimuli that can harm the body. Violations can be of a completely different nature. For example, a person may stop feeling pain or any touch; sometimes hearing, smell, and body temperature are impaired.
It often happens that the disease manifests itself during pregnancy. This is hypoesthesia of the lower extremities, because due to the increased weight of a woman, a greater load is placed on the legs. In this case, the doctor can only offer to alleviate the condition, because after childbirth everything will go away on its own. Some people face the problem of numbness in their hands precisely after sleep, which is associated with the accumulation of fluid, and this, as a rule, is a consequence of metabolic disorders in the body.
https://www.youtube.com/watch?v=upload
There are several types of hypoesthesia, so it’s worth dwelling on each of them separately:
- The polyneuritic type most often affects the upper and lower limbs of a person. The problem lies in the pathologies of the peripheral nerves.
- Conductive hypoesthesia manifests itself on one side, which is opposite to the one that was affected. We can say that this is precisely the main insidiousness of the disease.
- The radicular type is directly related to loss of sensitivity, and this cannot be ignored. All roots that are connected to the spinal cord are affected. When the lesion concerns only one root, symptoms cannot be noticed.
All types of hypoesthesia have their own distinctive symptoms, which are simply impossible not to pay attention to.
If symptoms begin to appear very often, then you should definitely consult a doctor. First, when sensation is lost, hypoesthesia may indicate malignant formations that precede the development of cancer and other serious diseases. The doctor will be able to prescribe an x-ray or CT scan for his patient. Electroneuromyography is also actively used today. The doctor will also be able to prescribe the following diagnostic methods:
- Blood analysis.
- Dopplerography. Using this diagnostic method, it is possible to identify vascular diseases such as atherosclerosis, varicose veins and thrombosis. Foot hypoesthesia may indicate these pathologies.
All diagnostics are prescribed only after visiting a neurologist and therapist. Based on the results obtained, specialists will be able to prescribe treatment.
Symptoms of obliterating diseases of the lower extremities
As a rule, occlusive diseases of the lower extremities cause intermittent claudication: a disturbing painful sensation, muscle spasm, discomfort or fatigue in the legs, which occurs during walking and decreases with rest. Symptoms of lameness usually occur in the lower legs, but may occur in the thighs, buttocks, or (rarely) arms. Intermittent claudication is a manifestation of exercise-induced reversible ischemia, similar to angina pectoris. As occlusive diseases of the lower extremities progress, the distance that a patient can walk without developing symptoms may decrease, and patients with severe disease may experience pain during rest, which is evidence of irreversible ischemia. Rest pain usually occurs in the distal parts of the limb, when raising the leg (often pain occurs at night) and decreases when the leg is lowered below cardiac level. The pain may feel like a burning sensation, although this is not typical. Approximately 20% of patients with lower extremity occlusive disease have no clinical symptoms, sometimes because they are not active enough to cause leg ischemia. Some patients have atypical symptoms (eg, nonspecific decreased exercise tolerance, pain in the hip or other joints).
Mild disease often does not cause any clinical manifestations. Moderate and severe degrees usually lead to a decrease or disappearance of the peripheral (popliteal, dorsum of the foot and back of the leg) pulse. If it is impossible to detect a pulse by palpation, Doppler ultrasonography is used.
When the limb is below the level of the heart, a dark red discoloration of the skin (called dependent erythema) may appear. In some patients, raising the leg causes pallor of the limb and aggravates ischemic pain. When the leg is lowered, venous filling time increases (>15 s). Swelling usually does not occur if the patient keeps the leg motionless and in a forced position to reduce pain. Patients with chronic occlusive disease of the lower extremities may have thin, pale skin with thinning or loss of hair. There is a feeling of coldness in the distal parts of the legs. The affected leg may sweat excessively and become cyanotic, likely due to increased sympathetic nervous system activity.
As ischemia progresses, ulcers may appear (usually on the toes or heel, sometimes on the calf, thigh, or foot), especially after local trauma. The ulcers are often surrounded by black necrotic tissue (dry gangrene). They are usually painful, but patients with peripheral neuropathy due to diabetes or chronic alcoholism may not feel this. Infection of ischemic ulcers (wet gangrene) develops frequently and leads to rapidly progressive panniculitis.
Mental changes. Nervous exhaustion. Asthenia. Depression. Psychosis
Depression and asthenia are frequent companions and a supporting factor in many chronic diseases. They are caused not just by a decrease in mood, but also by a biochemical imbalance of the central nervous system, incl. disorganization of the serotonin systems of the brain. A kind of vicious circle “illness-depression-illness” is formed. In most cases, a good treatment result is based on working with this vicious circle, i.e. on the treatment of the underlying disease and restoration of regulatory processes in the nervous system, incl. and serotonin regulation.
Under the influence of antidepressant treatment, immunity indicators and blood biochemistry, blood pressure, ECG, EEG change for the better, and sleep improves. The restoration of lost movement functions occurs faster, and spasticity also decreases.
Reasons for mental changes
There are several main reasons for depression in diseases of the nervous system:
- Immune and infectious aggression against the nervous system;
- Prolonged stress caused by illness;
- Long-term unpleasant symptoms (pain, weakness, etc.);
- Unpleasant medical procedures;
- Cerebrovascular accident;
- Forced change in lifestyle;
- Side effects of certain medications (for example, interferons).
Symptoms of mental changes
Personality change. The development of personality changes can be found in almost any brain disease. It is characterized by a sharpening (strengthening) of some personal characteristics to the detriment of others or the appearance of pathological personality traits. Thus, pathological aggressiveness, greed, suspicion, negativism and depression, euphoria, a pathological tendency to flat jokes, hypo- or hypersexuality, neglect of hygiene, excessive religiosity, etc. may appear. The ability to adequately assess one’s own actions decreases, hence conflicts with other people and troubles with the law. With a long course of the disorder, especially in the absence of treatment, a decrease in intelligence is possible.
Psychosis. In the long-term period of traumatic, infectious and intoxication diseases that cause the death of brain cells, periodic organic psychoses may develop. Often psychoses occur at regular intervals (sometimes they have a clear seasonality).
Possible symptoms:
- Twilight stupefaction with excitement;
- Hallucinations;
- Rave;
- Insomnia;
- Autonomic disorders (changes in blood pressure, body temperature, menstrual cycle, etc.).
Treatment of personality disorders
We recommend seeking help if you experience symptoms of a personality disorder. In our clinic, treatment is carried out in several directions at once:
- Preventing the death of brain matter. In addition to treating the underlying disease, nootropic drugs, antioxidants, and polypeptide drugs are used.
- Relief of depression and agitation, sleep disorders. Here, mainly nootropics with a calming effect, antidepressants and antipsychotics are used, in the correct combination that preserves normal vital functions.
- Working with a psychotherapist to understand and correct social and personal problems.
Causes
Hypesthesia often appears in people who lead a sedentary lifestyle or perform monotonous, repetitive work. This pathology also accompanies diabetes mellitus, which affects the body's metabolic processes.
A common cause of the disease is insufficient concentration of B vitamins in the human blood. Such hypoesthesia is accompanied by increased irritability of the patient, frequent dizziness, fainting and improper functioning of the digestive system.
Loss of sensation in the scalp can occur due to improper functioning of the cardiovascular and nervous systems.
Another reason for the appearance of numbness is the so-called tunnel syndrome, which is compression of the nerve endings that pass through narrow places in the human body.
In addition, migraines, head injuries, coronary heart disease, alcoholism, and heredity can be factors that provoke the appearance of numbness.
In addition to the reasons listed above, hypoesthesia can be caused by rheumatoid arthritis. The nerve is pinched by the deformed joint, causing the well-known numbness.
These symptoms require immediate diagnosis in a medical facility and the prescription of drug therapy.
Forecast of hypoesthesia
The prognosis will also depend entirely on what caused the condition. Without treatment, almost all of these diseases lead to disability. Therefore, at the first signs of a change in sensitivity, you should immediately consult a doctor and be sure to identify the underlying disease.
It should be noted that many diseases can be treated, you just need to respond to the symptoms in time and consult a specialist. When the pathologies are severe, a person’s reluctance to be treated can lead to disability and even death. Hypoesthesia on the left side is considered especially dangerous, as it indicates heart problems. In any case, the prognosis can be quite favorable, but only if the person consults a doctor in time and begins treatment.
Types of hypoesthesia
Facial hypoesthesia
May be a consequence of vascular or neurological pathologies. If loss of sensation is observed on only one side, this may indicate trigeminal neuralgia.
If the affected area appears red or a rash appears on it, then the cause may be the development of shingles.
If you are looking for a rehabilitation center for recovery, we recommend the rehabilitation center, which provides rehabilitation after a stroke, neurological diseases and chronic pain.
Hand hypoesthesia
If hypoesthesia of the hands is observed for two or more minutes, this may indicate diseases of the nervous system or vascular pathologies.
The condition can also be caused by a tumor, circulatory problems in the brain, or multiple sclerosis.
Hypoesthesia of the legs
This pathology may be a consequence of poor circulation in the lower extremities, which causes nerve damage. If hypoesthesia of the legs is accompanied by severe pain, this may indicate vascular diseases - obliterating endarteritis, venous insufficiency, atherosclerosis.
If hypoesthesia is accompanied by shooting pain in the leg or lower back, then sciatica is the likely cause.
Treatment of the disease
Having determined the symptoms of hypoesthesia, as well as its localization, it is necessary to urgently begin treatment without delay.
The selection of medications is carried out depending on what exactly caused the disease.
For example, if there is hand hypoesthesia associated with metabolic disorders, the doctor may prescribe a course of vitamin and mineral complexes.
Also, to treat numbness, a course of corticosteroids is sometimes used to relieve the exacerbation of the disease.
If the sensitivity of the legs is impaired, a warm shower and evening walks are usually used.
Additional treatment methods include :
- phonophoresis;
- electrophoresis;
- ultrasonic waves;
- darsonval;
- paraffin and ozokerite wraps;
- radon baths and mud;
- massage;
- yoga classes;
- acupuncture.
There is also the opportunity to use traditional medicine. You just have to keep in mind that self-medication is fraught with consequences, so you should always consult with your doctor.
Here are a few popular recipes for hypoesthesia :
- If your fingers are affected, you can take half a glass of sugar and vegetable fat and mix. Apply in circular motions to affected areas. After this, add 2 tablespoons of salt to a liter of warm water and dip your fingers in it for 45 minutes.
- If your legs are numb, honey wraps will be helpful. Sore legs should be lubricated with honey and wrapped in natural fabric. The course of treatment is 3–4 procedures.
- You can also take half a liter of vodka and 50 g of bush lilac flowers, leave for a couple of weeks, and then apply compresses to numb legs. Repeat for two weeks.
Before the treatment has its effect on the patient, he should exercise maximum caution so as not to accidentally harm himself.
So, if attacks are provoked by external factors, such as ambient temperature, time of day or physical condition, then they should be avoided if possible.
If you often experience numbness in your face, you need to be careful when eating, as you may accidentally bite your tongue or cheek.
If you have hypoesthesia, which manifests itself in the form of insensitivity to temperatures, you need to be extremely careful near heat sources, since during an attack you can involuntarily get burned.
Numbness and decreased sensitivity
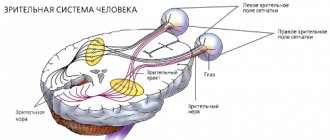
Numbness and decreased sensitivity are private companions of suffering in the nervous system. Decreased sensitivity and numbness occur for a specific reason: signals from the body's sensory receptors do not reach the brain or are not perceived by it. Why this happens can be found out during a neurological examination and through instrumental studies, incl. electroneuromyography and evoked potential studies. These neurophysiological studies test the entire sensory pathway, from the sensory receptor of the body to the cerebral cortex
It is important to find the cause of the sensory disorder and confidently treat a specific and understandable disorder or disease
To restore impaired sensitivity, in addition to treating the underlying disease, we will offer you magnetic stimulation. This treatment method makes recovery faster and easier. We recommend that you contact a neurologist to determine the cause of numbness and treatment.
Swing to the right: hemihypesthesia, parahypesthesia superior and inferior, hypoesthesia of one limb
Different diseases are characterized by different sensory disturbances (types of numbness). Possible causes of numbness or decreased sensitivity:
- Brain disease is characterized by impaired sensitivity or numbness of the extremities of the opposite half of the body: numbness of the right arm or leg when the left parts of the brain suffer, numbness of the left arm (leg) - the right.
- Spinal cord disease is characterized by impaired sensitivity below the site of injury, accompanied by tissue numbness.
- Polyneuropathy is characterized by sensory disturbances of the “gloves and socks” type.
- With a disease of one or another peripheral nerve, symptoms of numbness in the area of its innervation are characteristic: a feeling of numbness of the skin (including the head: facial skin, lips, tongue, etc.), numbness of the hand or fingers (fingertips, little finger, big toe), numbness of the foot.
Decreased sensitivity and numbness (as a symptom) in one or another part of the body may be associated with:
- With disruption of the conduction of nerve impulses from receptors that perceive sensations. This is possible when the receptors themselves die, the peripheral nerves, spinal cord or brain suffer;
- With the destruction of the area of the cerebral cortex that receives sensitive impulses.
More often we see a violation of all types of sensitivity at once, accompanied by partial or complete numbness of any part of the body. But only one or a few types of sensitivity may be affected. Thus, there may be a disturbance in the perception of only tactile, pain, temperature, joint-muscular sensations, sensations of pressure, movement, etc. This is typical for demyelinating diseases and polyneuropathy.
We will offer you treatment for numbness or decreased sensation based on our diagnostic findings.
Mental hypoesthesia
Mental hypoesthesia is a weakening of sensitivity up to its loss, i.e. anesthesia. The definition of “mental” indicates that the disorder is not associated with neurological pathology, conductive or central, nor is it associated with damage to the receptors of the corresponding sensory organs. Let us add one more important note to what has been said. In this fragment of the text, it is impossible not to touch upon the topic of the pathology of self-perception, that is, the loss of the ability to recognize certain sensations. It is quite difficult to distinguish between where there is a violation of the very process of formation of sensations, and where sensations are fully formed, but are not realized.
Moreover, both types of violations may well be combined with one another, and it is difficult to formulate any specific judgments here. Nevertheless, we will indicate two signs that allow, although not always, to make an appropriate distinction. Firstly, disturbances of the sensations themselves can be identified by objective research methods. For example, with the loss of pain sensitivity, the application of painful stimuli is not accompanied by the appearance of a sensation of pain. The loss of awareness of the feeling of pain is different in that the sensation of pain, as it turns out, is preserved to one degree or another. Secondly, the disturbance of sensations is often not noticed by the patient and is detected only during a special examination.
| | Our clinic accurately diagnoses such conditions. |
Often this disorder does not bother patients. In the case of a disorder of self-awareness, the patient will most often notice the fact of the disorder himself, and perhaps draw the doctor’s attention to it. In addition, such a disorder is often accompanied by a more or less pronounced reaction of suffering. In the following clinical illustrations of hypoesthesia, testimonies of patients exhibiting symptoms of impaired self-perception especially often appear.
A decrease in the intensity of sensations can occur in different analyzers and manifest itself in each of the above modalities. In accordance with this, we will indicate the symptoms of the disorder.
Mental hypalgesia and analgesia - reduction and loss of pain sensitivity. The term indolence is used less frequently. Loss of pain sensitivity, including persistent ones, is especially often detected in an acute psychotic state with symptoms of confusion, catatonia, delusions and hallucinations. The fact that the pain sensations in catatonic patients are preserved is evidenced by the vivid reaction of the pupils to pain - when painful stimulation is applied, the patients’ pupils dilate.
This symptom in catatonic patients was first described by O. Bumke (1903). Such patients often commit acts of self-harm and suicide with extensive self-injury to various organs, including internal ones, without any awareness of pain. Thus, the patient, on the orders of the “voices,” cut both of his legs “like sticks” without feeling any pain. Pain sensitivity is restored as the mental state improves. Awareness of pain is also lost in patients with severe depression, in a state of passion, when consciousness is stunned, in a hypnotic trance, in intoxication, or during meditation. The mechanisms of analgesia in this case are most likely heterogeneous. Thus, the loss of the feeling of pain during deafening of consciousness is possibly associated with the shutdown of higher levels of personality, in particular self-awareness, as well as a dysfunction of the cortical structures of pain.
Confusion of consciousness inevitably entails confusion of self-awareness, as is clearly seen in oneiroid, and, consequently, leads to a disturbance in the perception of various manifestations of the Self, including analgesia. In depression, awareness of pain is likely to be more affected. Pain sensitivity sometimes decreases due to depersonalization. Patients feel their own pain as if it belongs to someone else or is perceived somewhere far away and thus seems to lose its severity. Loss of superficial pain sensation (“quick pain”) occurs in patients with progressive paralysis, most likely due to damage to nerve cells and pain pathways.
Hysterical analgesia is explained by a selective focus of attention or, in the terminology of psychoanalysis, with the repression of the feeling of pain. This happens because hysterics benefit from disruption in one way or another. In any case, most doctors, following P. Janet and Z. Freud, still share such accusations of patients. During sleep, pain sensitivity often decreases - hypnoanalgesia. This is probably due to “sleepy inhibition” of nerve cells. A phenomenon such as audio analgesia—a decrease in pain sensitivity under the influence of loud sounds—has also been described. Audioanalgesia appears to be a consequence of reciprocal intermodal sensations. With tabes dorsalis, Abadi's symptom occurs - the absence of a pain response in response to compression of the heel tendon. Similar assumptions can be made for the following types of loss of sensitivity.
Mental anakusia and hypoacusia are loss (weakening) of the sensation of sound. Dulling of the acuity of perception of acoustic stimuli. It is especially common in depression. The sounds seem to patients to be weakened, indistinct, poorly modulated, coming as if from afar: “My ears feel stuffy, like there’s cotton in them, I don’t seem to hear enough, I can’t understand what they’re saying to me, sometimes I ask again.” With hysteria, functional deafness occurs, usually combined with loss of the ability to speak - surdomutism.
Mental anopsia and hypoopsia are loss (weakening) of photosensitivity. Depressed patients often report that bright lighting seems dim, dull, evening to them, everything is perceived as in a haze, through a veil, a veil, a curtain, as through a window on a rainy day, or as if the eyes were curtained, covered with a film. The contours of objects are not clearly perceived, they are seen as unclear, blurry, lacking clear outlines, fluctuating in the wrong light. At the same time, color perception also suffers. Colors seem faded, faded, pastel, shades of different colors are difficult to distinguish. With hysteria, functional amblyopia is observed - motivated blindness. The symptom of looking into the eyes is also characteristic: the patient looks directly into the eyes of the interlocutor, even if he changes his location.
Mental ageusia and hypogeusia are loss (dulling) of taste sensations. Described mainly in depression. Food seems tasteless, bland, and monotonous to patients: “It’s like you’re chewing grass or rubber. No matter what you eat, everything seems equally tasteless. If you don’t look at what’s on the table, it seems like you won’t be able to discern what kind of food it is... I don’t feel a sweet taste, the food seems bitter.” Ageusia can be partial, affecting only some submodal taste sensations. Objectively, taste sensitivity may not be impaired.
Mental anosmia and hyponosmia - loss (dulling) of olfactory sensations: “I don’t understand whether it smells like something or not... I can’t distinguish odors, like with a runny nose, it’s as if they’re not there at all... I don’t smell perfume... Food doesn’t seem to smell or smells somehow differently". Detailed questioning may reveal different shades of what patients describe as loss of smell. An objective test often does not reveal a violation of the sense of smell.
Mental anathia and hyponaphy - loss (dulling) of tactile sensations:
“The skin on my cheek is numb, my cheek feels like it’s made of wood, I touch it, but she feels almost nothing... The skin under the kneecaps seems to be frostbitten. I touch it, press it, but I don’t feel it... I don’t feel anything with my lips, it’s as if they’re not mine, as if they were glued... I wash myself in the morning, but I don’t feel the water with my hands, as if I’m rubbing with dry palms.” Areas of loss of sensitivity have different localization and configuration that do not coincide with the anatomical zones of innervation. In the Middle Ages in Europe, areas of skin anesthesia were considered “marks of the devil,” and such patients usually faced torture and the stake. If we consider such a disorder to be hysterical, then it is difficult to imagine what the “secondary benefit” could be here, supposedly characteristic of patients. In hysterical surdomutism, we add, tactile hypoesthesia of the skin of the ears and ear canals is simultaneously detected.
Mental apallesthesia and hypopallesthesia are loss (weakening) of vibration sensations. This is apparently indicated by the following reports from patients: “Everything inside froze, stopped... I don’t feel my heart beating, there seems to be no pulse... It’s like there’s nothing inside, there’s emptiness.”
Mental abathesthesia and hypobathesthesia - loss (weakening) of kinesthetic sensations: “My legs are like cotton wool, I don’t feel them well... My arms are numb, as if they were numb, as if I had been resting them... The movements are light, imperceptible, as if the joints are lubricated... I do everything with some incredible ease, effortlessly, my arms dangle as if on hinges.” Sometimes the perception of the position of body parts is disrupted: “I close my eyes and can’t understand how my arms lie, whether my legs are bent or extended, whether my fists are clenched or not... I don’t feel which way I turned my head, whether I’m sitting or lying.”
Mental abaresthesia and hypobaresthesia - loss (weakening) of sensations of pressure and weight: “I don’t feel the weight of the load... It seems to me that I can’t close my eyes and determine whether the bucket is full or empty... I can’t figure out whether I can handle this load or not... I seem to myself weightless... I seem to be so light, I’ll jump now and fly... My body seems to be as light as feathers. I’m afraid someone will sneeze or the wind will blow and I’ll be carried away... I squeeze my leg or arm, but I don’t feel it... They squeeze my arm with a tourniquet, but I don’t feel the pressure.”
Mental astatesthesia and hypostatesthesia - loss (weakening) of the static feeling: “The car accelerates, and I feel the acceleration only with my back... The plane falls into a hole, I only feel weightlessness, but there is no sensation of falling... It happened that you spin, stop and everything turns in the other direction. But now there is no such thing.”
Mental athermesthesia and hypothermesthesia - loss (weakening) of temperature sensitivity: “I can’t feel whether it’s hot or cold... I burned my hand and didn’t even feel it... I can’t feel with my hands whether the ice is cold... I don’t wear mittens or gloves, my hands don’t freeze... In winter, It’s frosty, I walk around without a hat and I don’t feel cold... I don’t feel the temperature. The thermometer says it’s about 40, but I don’t feel it at all.”
Back to contents
What causes numbness in the fingertips?
Paresthesia of the fingertips is usually bilateral. The most common cause of numbness in the fingertips is polyneuropathy. This is a simultaneous lesion of many peripheral nerves. The most vulnerable are the distal (that is, the most distant) areas. This explains the numbness of only the fingertips. In advanced stages, paresthesia spreads to the entire hand and above.
Causes of numbness in fingers and toes:
- diabetes;
- chronic renal and liver failure;
- systemic connective tissue diseases;
- toxic damage (alcohol, medication, infectious).
Diabetic neuropathy is clinically manifested in 50% of patients with diabetes. In the early stages, the myelin sheath is affected, after which the nerve fiber itself is destroyed. In addition to numbness, the patient is bothered by burning pain in the fingers, tingling, and chilliness.
Polyneuropathy in chronic renal and liver failure is characterized by the development of sensory and motor disorders.
Neuropathy develops while taking various medications:
- amiodarone;
- isoniazid;
- gold preparations;
- procainamide;
- drugs used for chemotherapy for cancer.
Drug-induced numbness subsides after appropriate therapy is stopped. The symptom worsens when treatment is resumed.
Paresthesia in the distal extremities may occur due to arsenic poisoning. The patient is bothered by severe pain in the fingertips. An objective examination reveals hypoesthesia or anesthesia.
Lead polyneuropathy develops over several weeks after exposure to a toxic substance. Numbness is preceded by intoxication syndrome, sleep disturbance, memory impairment, and irritability. Along with paresthesia, movement disorders develop.
Among infectious diseases, damage to peripheral nerves is most clearly represented in diphtheria. Polyneuropathy is caused by the action of a bacterial toxin and an autoimmune syndrome. Pathology develops 4-7 weeks after infection. Numbness from the fingers of the upper and lower extremities quickly spreads proximally with the development of deep paresis.
Prevention
Prevention of such a pathological process is as follows:
- quitting smoking and excessive alcohol consumption;
- timely treatment of diseases of any etiology;
- moderate physical activity;
- daily walks in the fresh air;
- balanced diet.
It is important to understand that you cannot self-medicate, and if you feel unwell, you should immediately consult a doctor. Is everything in the article correct from a medical point of view?Answer only if you have proven medical knowledgeYesNo
Is everything in the article correct from a medical point of view?Answer only if you have proven medical knowledgeYesNo
Diseases with similar symptoms: Cerebral edema (overlapping symptoms: 10 out of 20)
... Migraine (overlapping symptoms: 8 out of 20)
... Chronic fatigue syndrome (overlapping symptoms: 8 out of 20)
... Vitamin deficiency (matching symptoms: 6 out of 20)
...Venous dysgemia (overlapping symptoms: 6 out of 20)
...Which doctor should I contact?
If you suspect a disease such as hypoesthesia, you should consult a doctor:
A neurologist is a doctor who diagnoses and treats diseases associated with the central and peripheral nervous system. Read >
Best Neurologists in Ekaterinburg
A pediatrician is a pediatrician who specializes in child health, diagnosis, prevention and treatment of diseases in children. Read >
Best Pediatricians in Ekaterinburg
A therapist is a general specialist whose competence includes issues of early diagnosis and treatment of many diseases. Read >
Diagnostic techniques
If hypoesthesia occurs frequently and lasts more than 2–3 minutes, you should immediately contact a neurologist for examination. It includes the following procedures:
- initial examination, identification of complaints, symptoms, clarification of the patient’s lifestyle and adherence to his bad habits;
- a general blood test to detect iron deficiency or pernicious anemia;
- a blood test for cholesterol and lipoprotein, which makes it possible to identify a tendency to form atherosclerotic plaques;
- computed tomography (CT) and x-ray - these studies will help determine the presence of bone fractures that have caused damage to nerve fibers, and will also help diagnose osteochondrosis, arthritis and other pathologies;
- electroneuromyography, which will make it possible to find the place where the nerve is damaged;
- Doppler ultrasound examination, which makes it possible to detect vascular pathologies such as varicose veins, atherosclerosis, thrombosis and others.
How to prevent the problem
Dental hyperesthesia (hereinafter referred to as DZ) affects mainly people aged 30 to 60 years (most of them are women). GZ are caused by non-carious defects:
- pathological abrasion of enamel;
- wedge-shaped damage, erosion;
- any other injuries associated with violation of the integrity of tooth enamel, its thinning and exposure of dentin.
GZ often becomes a complication of cervical caries, leading to gum recession, demineralization (thinning) of tooth enamel and “exposure” of dentin
The cause of hyperesthesia of hard dental tissues is also cervical caries. This dental problem leads, first of all, to demineralization of tooth enamel (since it becomes thinner as a result of instability to “attacks” of acids), and then to tooth decay. Unprofessional treatment of various oral diseases can also provoke dental hypersensitivity. Thus, the fight against caries and poor-quality filling (etching) of canals are often “triggers” for the development of dental disease.
Damage to the integrity of the tooth in the form of splits, cracks, and broken parts of the crown also results in increased sensitivity of the enamel to “attacks” of irritants.
Other factors causing HS:
home or professional teeth whitening (leads to the loss of micro- and macroelements by the enamel, thins the enamel) - with such procedures regularly, teeth begin to react to even minimal exposure to irritants; inflammatory and dystrophic pathological changes in the periodontium lead to exposure of the cervical zone of the teeth and to enamel hypersensitivity; the use of toothbrushes with hard bristles, careless use of floss (threads), poor-quality prosthetics (filling) - all this results in recession (traumatic damage) of the gums and is fraught with gum disease in the long term.
Hypoplasia of tooth enamel
- endocrinopathies;
- psychoneuroses;
- acute and chronic diseases of the gastrointestinal tract (GIT);
- metabolic disorders (eg, diabetes, obesity);
- hormonal changes (including age-related).
Experts have not established the final cause of dental hypersensitivity; this phenomenon is usually regarded as polyetiological (occurs as a result of the simultaneous action of several factors).
Prevention of hyperesthesia involves the regular use of special oral care products, which help prevent pronounced pain in the teeth when in contact with irritants. When the pain subsides, medicated toothpastes are replaced with hygienic ones.
Competent home and professional oral care is the best prevention of hyperesthesia
Pastes whose action is aimed at preventing hypersensitivity must necessarily contain the following active ingredients:
- sodium fluoride compounds;
- strontium chlorides;
- citrates;
- potassium compounds.
The full list of active ingredients and their concentration depends on the manufacturer. It is better to change toothpastes from time to time in order to increase the effectiveness of the use of these therapeutic and prophylactic agents. After leveling the symptoms of gastrointestinal tract, preference should be given to toothpastes with a low content of abrasive particles or cleansing gels. Toothbrushes should be “equipped” with soft or very soft bristles (depending on the severity of the pain syndrome).
The use of floss and toothpicks should not be associated with injury to the gingival papillae. Modern scientific research is aimed at creating a material that would fill holes in damaged dentin that are open to irritants. Recently, British scientists managed to develop coated silicon nanoparticles. In the future, they will be used for the prevention of caries and restorative therapy of hypersensitive teeth.
Patients with sensitive teeth should prefer brushes with soft bristles.
So, hyperesthesia is called increased sensitivity of dental units when in contact with various irritants. This problem can have either a “local” origin (complication of caries, dystrophic, inflammatory processes in the periodontium), or be a consequence of hormonal and metabolic disorders in the body.
Hypoesthesia of the leg (hips, legs, feet)
In most cases, hypoesthesia of the leg occurs against the background of the development of lumbosacral osteochondrosis and its complications. Bilateral hip hypoesthesia is the first clinical sign of cauda equina compression. This may be a symptom of a coccyx injury or arthrosis of the sacrococcygeal joint. Unilateral damage is typical for compression of the radicular nerve in the L5-S1 space. With tunnel syndromes, hypoesthesia of the feet, sagging of the arches and the development of transverse, longitudinal or mixed flat feet may appear.
When hypoesthesia of the lower leg appears, it is important to exclude vascular pathologies, such as:
- varicose veins of the lower extremities with severe swelling of the lower third of the leg;
- atherosclerosis (the formation of cholesterol plaques primarily occurs in the large blood vessels of the lower limb);
- obliterating endarteritis (more often formed in men aged 30 to 45 years who smoke);
- diabetic angiopathy.
When the first signs of hypoesthesia of the lower extremities appear, you should consult a neurologist. This doctor will be able to determine the exact cause of the sensitivity disorder during the initial examination.
Psychotherapy
51. Hypesthesia (2):
- reduction of pain sensitivity
- weakening of temperature sensitivity
- feeling of pain when exposed to temperature
- sensation of pain upon tactile influence
- absence of all types of general sensitivity
52. Anesthesia (3):
- loss of pain sensitivity
- loss of temperature sensitivity
- feeling of pain when exposed to temperature
- sensation of pain upon tactile influence
- loss of all types of general sensitivity
53. Hyperesthesia (2):
- increased pain sensitivity
- increased temperature sensitivity
- feeling of pain when exposed to temperature
- sensation of pain upon tactile influence
- "crawling" sensation
54. Hyperpathy (2):
- weakening of the sensitivity threshold
- increased sensation with an unpleasant emotional connotation
- sensation after cessation of irritation
- paroxysms of nociceptive pain
- paroxysms of neuropathic pain
55. Allodynia (2):
- weakening of the sensitivity threshold
- increased sensation with an unpleasant emotional connotation
- feeling of pain when exposed to temperature
- sensation of pain upon tactile influence
- 5. nociceptive pain
56. Causalgia (3):
- loss of pain sensitivity
- loss of temperature sensitivity
- feeling of pain when exposed to temperature
- spontaneous or caused by non-painful irritation intense pain
- local autonomic disorders
57. Neuralgia (2):
- loss of all types of sensitivity
- peripheral paresis
- spontaneous or caused by non-painful irritation, short-term (seconds) intense pain
- short-term pain similar to an electric shock
- 5. local autonomic disorders
58. Studies of tactile sensitivity (2):
- tuning fork with frequency 128 Hz
- tuning fork with frequency 256 Hz
- synthetic threads (Frey's hairs)
- Weber compass
- thermopen
59. Two-dimensional spatial sensitivity is (1):
- stereognosia
- graphesthesia
- hypoesthesia
- hyperesthesia
- anosognosia
60. Vibration sensitivity studies (1):
- tuning fork with frequency 128 Hz
- tuning fork with frequency 256 Hz
- synthetic threads (Frey's hairs)
- Weber compass
5. thermopen
61. An early sign of damage to the posterior cords of the spinal cord is a decrease in (1):
- vibration sensitivity
- joint-muscular feeling
- pain sensitivity
- temperature sensitivity
- stereognostic sense
62. When peripheral nerves are damaged, the first types of sensitivity usually decrease (1):
- vibration sensitivity
- joint-muscular feeling
- pain sensitivity
- temperature sensitivity
- stereognostic sense
63. Study of joint-muscular feeling (2):
- tuning fork with frequency 128 Hz
- assessment of the sensation of passive movements in the terminal phalanges of the fingers and toes
- synthetic threads (Frey's hairs)
- assessment of limb position sensation
Quantitative sensory testing evaluates function
(1):
- thin fibers of peripheral nerves
- thick fibers of peripheral nerves
- myelin sheath of peripheral nerves
- posterior cord of the spinal cord
- lateral cords of the spinal cord
72. On the DN4 scale, the correspondence of pain is determined (3):
- burning sensation
- painful feeling of cold
- painful sensation of warmth
- sensation of current passing
- painful sensation of touch
73. The DN4 scale determines whether pain is accompanied by (2):
- ataxia
- paresis
- pelvic disorders
- numbness
- itching
74. On the DN4 scale, it is determined whether the pain can be increased in the area of its localization (1):
- holding a brush in this area
- active movement of the limb
- passive movement of a limb
- walking
- long standing
Causes of hyperacusis
The development of pathology is associated with discoordination of the processes of excitation and inhibition in the auditory pathways. The limbic system plays a role in this. An increase in noise is observed during strong emotions: stressful situations, experiences, but the impulses from the ear have the same strength. This leads to increased anxiety and stimulates the limbic and sympathetic systems.
Increased sound sensitivity can develop at any age. It happens:
- partial: certain sounds cannot be tolerated;
- complete: all loud sounds cause pain and anxiety.
The causes of hyperacusis are varied:
- Infectious diseases of the brain: meningitis, encephalitis.
- Head injuries.
- Neurological diseases: neuroses, panic attacks.
- Vascular pathologies: stroke.
- Paresis of the stapedius muscle.
- Meniere's disease.
- Brain tumors.
Each of these conditions is accompanied by signs of the underlying disease. There are several degrees of discomfort:
- There are sensations of tingling and popping in the ears, pressure when exposed to low-frequency noise.
- Additionally, low and high frequencies of noise cause concern, there is a tickling sensation, and speech intelligibility decreases by 10–30%.
- Pain in the ears occurs, patients ask others to speak more quietly, speech intelligibility is reduced by 40–80%.
- The patient cannot tolerate noise and quiet sounds, and is accompanied by vegetative and emotional disorders. Speech is 100% unintelligible.
Symptoms and signs of the disease
Hypoesthesia can be recognized by the following signs:
- high frequency of disease attacks;
- insensitivity to temperature changes;
- numbness in the head, neck, back, as well as paralysis;
- weakness and speech disorders;
- loss of smell;
- short-term loss of consciousness, difficulty breathing;
- dizziness and gait disturbance;
- burning, itching, tingling sensation and rash;
- numbness of the limbs while walking;
- pain in the lumbar region, muscle spasms;
- with facial hypoesthesia, vision and hearing may deteriorate, and the temperature may rise;
- Involuntary bowel movements or emptying of the bladder may occur.
Symptoms of mental hyperesthesia
Mental hyperesthesia often occurs. This is a pathology in which symptoms such as emotional instability and excessive irritability are felt. The patient reacts too violently and inadequately to various external stimuli
It does not matter which receptors or sense organs are irritated: olfactory (weak odors), auditory (rustling, ticking of a clock), tactile (prick, light touch). The patient becomes emotionally unstable, easily excited, and cannot control his own emotions adequately
In some cases, patients experience many unpleasant, pointless sensations that arise in different parts of the body and cannot be localized. Too frequent occurrence of symptoms indicates additional diseases that the patient has. That is why, before starting treatment, their presence should be refuted or confirmed.
Etiology and pathogenesis
Hemihypesthesia develops when one of the links of the reflex arc is damaged. With damage to the upper parts of the nervous system (cerebral cortex, medulla oblongata), a decrease in sensitivity occurs on the opposite side due to the intersection of the pathways. So, if a person was struck by a left-sided stroke, then hemihypesthesia will be right-sided.
If the disturbances occurred at the level of the spinal cord, then loss of sensitivity covers the side that was affected.
Reasons for decreased sensitivity include:
- stroke;
- head and spinal column injuries;
- neuroinfections and inflammatory lesions;
- ischemia of a portion of the brain or spinal cord;
- compression of fibers by neoplasms or spinal hernia;
- degenerative processes in the central nervous system and brain.
Damage to nerve structures due to sensory disorders
Most often, hemihypesthesia develops after an acute disruption of blood supply to the brain. Moreover, in the case of a stroke in the right sections, sensitivity is lost on the left side of the body, and vice versa. Superficial sensations are reduced on the affected side in spinal cord injuries.
Deep sensitivity is lost on the side of the same name if the violation occurs below the level of the medial lemniscus - to the chiasm.
Hypesthesia of the hands (fingers and hands)
Hand hypoesthesia is a common symptom of the development of tunnel syndromes. If the carpal valve or carpal tunnel is damaged, hypoesthesia of the fingers occurs, and if the ulnar nerve is damaged, the entire hand on the affected side may become numb.
In addition to tunnel syndromes, hand hypoesthesia accompanies brachial plexitis or plexopathy. When any of the three branches extending from the brachial nerve plexus is compressed, sensory disturbances in the hand and forearm may occur. Then the loss of sensitivity spreads to the shoulder.
With hypoesthesia of the hands, it is important to begin differential diagnosis with a comprehensive examination of the condition of the cervical spine. There may be two pathological factors that have a negative impact on the process of innervation of the upper extremities:
- with osteochondrosis complicated by protrusion and disc herniation, pressure is exerted on the radicular nerve responsible for the innervation of the arm;
- With posterior vertebral artery syndrome, the blood supply to the brain structures responsible for conducting sensory impulses from the upper extremities is disrupted.
Therefore, it is necessary to conduct a comprehensive diagnosis. Depending on the identified pathology, an individual course of therapy is prescribed.