Definition
Neuroepithelial cysts (NCs) , also called neuroglial or glioependymal cysts, are developmental anomalies resulting from the absorption of part of the developing neuroectoderm, from leptomeningeal neuroglial heterotopia, or from folds of the choroidal pia mater in the case of choroidal sulcal cysts. NCs can be classified according to location into intraventricular, choroidal sulcus, and intraparenchymal cysts.
Magnetic resonance imaging (MRI) in St. Petersburg
MRI of the brain. T2-weighted axial tomogram. Arachnoid cyst. Color processing of the image.
Most brain cysts are developmental anomalies. Some formations that arise due to developmental disorders have features similar to cysts.
Epidermoid cysts (epidermoids) are benign congenital formations. They originate from ectopic epidermal cells and develop during the closure period, 3-5 weeks. embryogenesis, as a consequence of the incomplete separation of neuronal and integumentary ectoderm. The incidence is approximately 1% of intracranial lesions. Usually diagnosed between the ages of 25 and 45. The localization of epidermoids can be any, but the typical ones are the cerebellopontine angle (the third most common formation in this area), the prepontine cistern, the parasellar region, the quadrigeminal tract and the ventricular system, very rarely in the hemispheres, spinal cord and intradiploid. They grow intra- or extradurally, expansively, slowly, squeezing the brain stem and intracranial nerves, but without destroying the bone. Sometimes vessels and nerves are involved. Based on the nature of their growth, they can be classified as tumor-like formations. Aseptic inflammation often develops around the epidermoids, and when ruptured, the contents (fat, keratin) break into the cerebrospinal fluid spaces. Clinical manifestations depend on location and mass effect.
MRI of the brain shows a nonspecific picture and depends on the contents of the cyst. If it does not contain fat, then it has a cerebrospinal fluid signal intensity. In this case, the epidermoid cyst is difficult to distinguish from the arachnoid cyst, although, as a rule, it is not so homogeneous. On FLAIR MRI and diffusion-weighted MRI images, the contents of the epidermoids are lighter than the cerebrospinal fluid content. Fat contents, such epidermoids are also called cholesteatoma, lead to a high signal on T1-weighted MRI of the brain. Apparently it is caused by lipids, but not cholesterol. On T2-weighted MRIs of the brain it is less intense than cerebrospinal fluid. The contours of the epidermoids are always clear. Cholesteatomas make up only 3-5% of epidermoids. In 15-20% of cases, calcification occurs along the periphery of the cyst. Contrasting walls are rarely observed.
MRI of the brain. T1-weighted coronal and sagittal MRI. Epidermoid cyst of the left temporal lobe.
Dermoid cysts are less common than epidermoid cysts, accounting for about 0.3% of intracranial formations. Usually detected between the ages of 10 and 20 years. Morphologically, they are distinguished from epidermoids by the presence of ectodermal elements - hair follicles, sweat glands, etc. Typically they are located along the midline (in contrast to epidermoids, which are often extra-axial): in the suprasellar cistern, subfrontally, around the pons and, very rarely, parapinially, periorbitally, in the fourth ventricle, in the cauda equina region and intradiploid. They are distinguished from epidermoid cysts on MRI of the brain only by the pronounced heterogeneity of the structure; in addition, they are always bright on T1-weighted MRI of the brain due to the high content of lipids. When there is a rupture and breakthrough into the subarachnoid space, a level appears in it; on T1-weighted MRIs of the brain, light fat floats on the cerebrospinal fluid.
Lipoma is an accumulation of embryonic fat cells mixed with collagen in the subarachnoid space. Lipomas originate from the remains of the primitive embryonic membrane. This malformation of the meninges is associated with impaired differentiation of the mesenchyme into the pia mater and subarachnoid space. The incidence of lipoma is less than 0.5% of intracranial lesions. Typically, lipomas are localized in the corpus callosum, in the interhemispheric fissure, the pituitary infundibulum and the hypothalamus, less often around the cerebellar vermis and the quadrigeminal plate and the cerebellopontine angle. Lipomas of the corpus callosum are combined with its agenesis and in 60% of cases with spread to the choroid plexus. On MRI of the brain, the lipoma is clearly defined, without swelling around it or mass effect, and does not destroy the bone. The structure of the formation is often homogeneous, with fatty signal intensity - that is, clearly hyperintense on T1-weighted MRI and slightly less intense in relation to the cerebrospinal fluid on T2-weighted MRI. Sometimes there are heterogeneous lipomas with areas of low signal from calcifications and vessels passing through it. If the diagnosis is in doubt, a fat-suppressed MRI of the brain should be performed or a CT scan can be done. On CT, the lipoma is always sharply hypodense and may contain calcium inclusions.
MRI of the brain. Sagittal T1-weighted MRI. Lipoma of the corpus callosum.
Ependymal cysts are very rare. They are congenital lacerations within the ventricles or cisterns. On an MRI of the brain, the outline of the cyst is clear, the signal is of cerebrospinal fluid intensity or slightly lighter due to the absence of pulsation and protein impurities, the structure is homogeneous. Unlike cysts of the transparent septum, it is not split, but displaced.
Arachnoid cysts are accumulations of cerebrospinal fluid between the layers of the split arachnoid membrane. An arachnoid cyst is usually not accompanied by other malformations. A small part of arachnoid cysts is of acquired origin - a consequence of leptomeningitis, surgery or hemorrhage. The incidence is approximately 1% of intracranial lesions. The sex ratio is M:F as 4:1. Typical localization is the middle cranial fossa (in the area of the Sylvian fissure 50%), interhemispheric fissure, cerebellopontine angle (11%), behind the clivus or at the level of the quadrigeminal (10%), in the area of the cerebellar vermis (9%), less often in the area interpeduncular and prepontine cisterns (3%), as well as suprasellar and chiasmal cisterns. Retrocerebellar arachnoid cysts are quite often found behind the cerebellum and are distinguishable from mega cisterna only by the unchanged posterior cranial fossa. The contents of the cyst are pure liquor, the walls are smooth, clearly defined, and there may be septa inside the cyst. Small arachnoid cysts are very difficult to see. By changing the width of the window and its level on T1-weighted MRI images, you can notice that the cyst is slightly lighter than the cerebrospinal fluid. Differential diagnosis from epidermal cysts is best achieved using the FLAIR MRI sequence. Epidermal cysts become bright, in contrast to hypointense arachnoid cysts.
Neuroglial (neuroepithelial) cysts are congenital cysts of various etiologies, localized in the brain parenchyma or in the area of the choroid plexus of the ventricles. Usually round, with smooth walls. Very often, such cysts are combined with developmental anomalies: the absence of a transparent septum and polymicrogyria. On MRI of the brain, the contents of the cysts are cerebrospinal fluid, sometimes with a small admixture of protein.
A special article is devoted to leptomeningeal cysts.
A colloid cyst is a congenital neuroepithelial formation. The colloid cyst is lined with epithelium and has a fibrous capsule. They make up about 1-2% of volumetric intracranial formations. Usually diagnosed between 30 and 50 years of age. An MRI of the brain shows that the cyst is always located in the anterior-superior segment of the third ventricle between the foramina of Monro. Its outline is clear, its shape is round, and its contents are heterogeneous. The size ranges from 3 mm to 4 cm, with larger sizes it closes the foramina of Monroe and causes occlusive hydrocephalus. A signal of envy from the admixture of protein in the liquor. In the presence of protein mucoid contents, the cyst is hyperintense on T1-weighted MRI and hypointense on T2-weighted MRI, but there are variants that are hyperintense on both types of tomograms, ring-shaped or mixed. No contrast is observed.
CT and MRI of the brain. Colloid cyst of the third ventricle.
Rathke's pouch cyst is a rare formation from the remains of embryonic ectoderm (Rathke's fissure), located between the lobes of the pituitary gland. It is detected at any age, but more often at 50-60 years. Clinical manifestations are associated with mass effect. A scan of the brain reveals a small (3-5 mm) cyst with a clear contour, without swelling around, and homogeneous in structure. The signal depends on the content. With serous contents, the signal is typically liquid; with mucoid cysts, the cyst is light on T1-weighted MRI. In rare cases, the cyst reaches large sizes and even extends beyond the saddle. The cyst wall is sometimes enhanced by contrast.
MRI of the brain. T2-weighted coronal MRI. Rathke's pouch cyst.
The pineal cyst is located in the projection of the pineal gland. Occurs with a frequency of 4-11%. The sizes usually do not exceed 1 cm, but occasionally they are found in larger sizes. In such cases, it causes occlusive hydrocephalus. In the brain, it has all the signs of a cyst with an admixture of protein in the fluid, that is, a little light on T1-weighted. Rarely, hemorrhagic contents occur. The cyst can be contrasted along the periphery.
MRI of the brain. Sagittal T1-weighted MRI. Pineal cyst.
Midline cysts—cavum septi pellucidi, cavum Vergae, and cavum veli interpositi—are normal structures of the fetal brain. Within 6 months after birth, in most people they disappear, but they can persist and are visualized on an MRI of the brain. Apparently, these cavities have no clinical significance and are incidental findings during tomography. The septum pellucida cyst (also called the V ventricle) is the medial wall of the lateral ventricles and is bounded anteriorly by the genu of the corpus callosum, superiorly by the corpus callosum, and posteriorly by the pillars of the fornix. Verge's cavity is a posterior continuation of the septum pellucida cyst and is located between the bodies of the ventricles. Usually both cysts are combined. The intermediate velum cyst is located in the roof of the third ventricle (tela choroidea), between the triangles of the lateral ventricles at the level of the foramina of Monro. It is bounded superiorly by the corpus callosum, posteriorly by the quadrigeminal cistern, and inferiorly by the third ventricle.
During MRI in St. Petersburg, we pay attention to the possibility of not only congenital, but also rare conditions, which include brain cysts
- consequences of stroke
- tumor cysts
- parasitic cysts
MRI of the brain. Coronal T1-weighted MRI. Multilocular hydatid cysts.
Brain cysts are equally visible in high-field and low-field open MRI. MRI of St. Petersburg provides the location of choice for MRI.
Leave feedback.
MRI in St. Petersburg USA
Morphology
Intraventricular neuroepithelial cyst
Intraventricular neuroepithelial cysts arise from the choroid plexus, usually at the level of the glomerulus in the triangle of the lateral ventricle. In such a location, they are often bilateral, and usually do not require any treatment. However, they can increase due to the secretive activity of the hair epithelium.
Fig. 1 Bichat's fissure cyst (choroidal fissure cyst)
Due to the relationship between the choroidal fissure and the choroid plexus, cysts associated with the choroidal fissure are considered to be of neuroepithelial origin, although they have also been classified among arachnoid cysts. Because they are located close to the hippocampus, which is often compressed, they can cause complex partial seizures.
Fig.2 Intraparenchymal NC
Intraparenchymal neuroepithelial cysts are very rare. Differentiation from dilated perivascular spaces (see below) may not be possible on imaging, although location in the pericommissural or periventricular regions and multiplicity strongly favor dilated perivascular spaces. Sometimes, high-resolution MRI can detect a tiny band corresponding to the vessel's entry space. In the absence of such functions, they may be considered intraparenchymal NCs. Several histologically proven cases showed glio-ependymal elements along the cyst wall
Liquid collectors for anatomical variants
Fluid reservoirs, sometimes cystic in appearance, may result from accumulation of CSF in non-arachnoid cavities, which represent paraphysiologic developmental variations. These volumes usually cause slight deformation of adjacent structures, and, as a rule, are found in oligosymptomatic or completely asymptomatic children. These conditions include pseudocystic dilatation of the perivascular (ie, Virchow-Robin) spaces, cavities of the septum pellucida, cavities of Verges, and the spaces of the velum intermedius.
Expansion of perivascular spaces (PVS or Virchow-Robin spaces)
Perivascular spaces are tiny spaces that surround the arteries, arterioles, veins, and venules that penetrate the brain parenchyma. Contrary to what was commonly thought, the SVCs are not continuous with the subarachnoid space. Rather, they are separated by a single (cortex) or double (basal ganglia) layer of pia mater that invaginates with penetrating arteries.
Thus, the pia mater separates the PVC from the subarachnoid space, and the PVC is not filled with CSF, but rather with interstitial fluid, with the pia mater acting as a regulatory interface between the two compartments. PVAs are also functionally important in the elimination of high molecular weight substances from the brain. Thus, blocking such pathways can lead to the accumulation of these substances in the extracellular spaces of the brain.
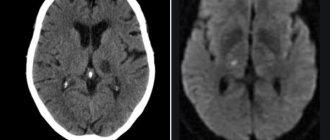
On imaging, PVP appears as smoothly demarcated, circular, linear parallel areas that are similar in signal intensity to CSF. So they are ↓ on CT, ↓ on T1, ↑ on T2, and ↓ on FLAIR. There is no perifocal gliosis. They tend to cluster around the anterior commissure and inferior parts of the basal ganglia, as well as in the external capsule.
Fig.3
Periventricular regions, especially posteriorly around the triangles, are another typical location of prominent VVP. Unlike other regions, the periventricular VVP may be surrounded by a hyperintense rim on FLAIR in the pediatric age group. This may reflect incomplete myelination of the white matter (ie, terminal zones) or possibly spongy changes. In white matter, their orientation is typically radial, reflecting the course of penetrating arteries within the brain parenchyma.
The normal diameter of PVP does not exceed 5 mm under normal conditions. However, there are known cases of frank dilatation of the RVP, which can occur in the absence of any pathological condition as an anatomical variant. “Giant” PVS can be up to 3 cm in diameter and may be difficult to distinguish from neuroepithelial cysts on imaging. Recognition of radial orientation or direct central visualization on high-resolution MRI is helpful for correct diagnosis. Occasionally, expansion of the PVP may be widespread and involve both hemispheres of the brain.
Several pathological conditions can be characterized by dilatation of the PVP. In the pediatric age group, this includes storage diseases such as mucopolysaccharidoses (ie types I and II). In these disorders, blockage of the PVP is thought to result in the accumulation of abnormal materials in the PVP. In such cases, the PVP expansion noticeably includes, in addition to the periventricular white matter, the corpus callosum. Thus, the discovery of several callosal PVAs should prompt metabolic studies. In addition, VVP can provide a route for the spread of a number of diseases, including infections, inflammation, demyelination and tumors.
Cavity of the septum pellucida and Verge's cavity
The septum pellucidum is a thin two-layer curtain located between the anterior parts of the corpus callosum above, and the anterior columns of the fornix and anterior commissure below.
The septum pellucidum cavity (SCP) is a virtual midline. The cavity between the two layers of the septum under the corpus callosum. The continuation of the cavity into the space between the hippocampal commissure below, and the callosal isthmus and splenium above, is called Verge's cavity (VC).
PPP is present in the majority (i.e. 97%) of individuals, in 85% at 2 months and 41% at 3 months postnatal age, while it is found in 12%-20% of mature brains. CV is found in 100% of fetuses at 6 months of pregnancy but only in 30% of individuals subsequently; the incidence in mature brains is 1%-3%. Frank dilatation of the PPP and CV often represents an incidental finding in neuroimaging performed for a number of reasons.
Headaches are a common concern, although it is difficult to correlate headaches with dilated PPP/PV. An increase in the prevalence of abnormal PPP/PV has been noted in patients with schizophrenia and other affective disorders since childhood. An increased prevalence of abnormal PPP has also been implicated as a marker of neurodevelopmental delay.
In the photographs, recognition of PPP/PV is simple. Dilatation of the RPP, either isolated or associated with a cyst, when it exceeds 10 mm in transverse diameter. Sagittal images separate downward displacement of the fornix from the corpus callosum, which is a typical finding.
Progressive dilatation of the vein is noted in several individuals, either as a single change or in association with ventricular dilatation.
Fig.4
Cyst of the transparent septum. Fig.4a and Intermediate sail cyst Fig.4b Fig. 4c
Intermediate velum cyst
The intermediate velum forms the roof of the third ventricle and consists of a double layer of pia mater, which constitutes the choroidal body, including the choroid plexus from the third ventricle, expanding from the pineal body to the foramina of Monro.
A velar intermedius cyst (SVIC) is a potential space placed between the posterior portion of the third ventricle below and the commissural plate above. The anatomy of the checkpoint is still a matter of debate. The CPP has been variously described as lying above the choroidal body of the third ventricle or within the bilayer of the pia mater, as well as being superior to, or containing, the internal cerebral veins.
However, all authors agree that the CP is present, despite the separately existing cavities of the septum pellucida and Verge's cavity, but is not excluded from the CSF flow paths and actually communicates posteriorly with the subarachnoid space of the quadrigeminal cistern. CPP is present in 2%-3% of children over 2 years of age and is usually an incidental finding, although there have been reports of an association with mental and motor developmental retardation, epilepsy, and infantile autism.
Cystic dilatation of the CP is best assessed on a sagittal MRI image, forming a cavity filled with CSF that lies inferior to the isthmus and splenium of the corpus callosum and does not extend ventral to the columns of the fornix. The paired internal cerebral veins are usually located near and on the lateral sides of the choroid plexus of the third ventricle, and then are directed posteriorly under the splenium of the corpus callosum and join the vein of Galen.
The presence of cystic dilatation of the CAT under the splenium of the corpus callosum is accompanied by a downward deviation of the internal cerebral veins, while the fornix remains in place. This represents a noticeable difference between the CPP and the manifestation of the Verge's cavity.
Septum pellucida cyst
If we talk about transparent septa (Verga's cyst), then these are two thin plates of the medulla with a gap, which, in fact, will be separated. This fissure is located in the area between the fornix and the anterior part of the corpus callosum. In some people, the diameter of the cyst is 1-2 mm, while in other cases the cysts grow to several centimeters. Today there are many classifications of this pathology. To begin with, it must be said that a septum pellucida cyst can be congenital (formed in the fetal brain during intrauterine development) or acquired (formed after birth, in children or adults). In addition, cysts are divided based on their location. For example, in some patients the cyst is located in the anterior zone of the interventricular septum. Sometimes it is located in the cerebellum. These factors, of course, must be taken into account when treating a cyst.
A cyst of the transparent septum mainly forms during fetal development. According to statistics, about 60% of babies (and 100% of premature babies) are born with a cyst in the brain.
As for the reasons, they look approximately the same, regardless of whether the cyst appears in adulthood or during fetal development:
- diseases accompanied by inflammation of the membranes of the brain;
- injuries and diseases accompanied by cerebral hemorrhages;
- varying degrees of concussion;
- diseases of infectious origin, especially those affecting the meninges.
In fact, in most cases, the presence of a septum pellucida cyst in the brain is not clinically evident—the patient is not even aware of the problem. Moreover, a cyst of the transparent septum of the brain, the size of which is not too large, is usually discovered by chance during the diagnosis of another disease. Sometimes a cyst
begins to compress neighboring parts of the brain, from time to time blocking the foramen of Monroe. What symptoms should you look out for? Patients typically complain of the following:
- severe headaches that appear suddenly and disappear just as suddenly;
- increased intracranial pressure;
- disruption of the hearing aid - patients note a decrease or deterioration in hearing, the appearance of tinnitus;
- some patients complain of a feeling of squeezing in the head area.
Naturally, when treating a cyst, it is important to determine the primary disease and carry out appropriate treatment, be it an infection or an inflammatory process. When intracranial pressure increases, patients are prescribed drugs that normalize the circulation of cerebrospinal fluid. The treatment regimen usually includes osmotic diuretics (remove excess fluid), agents to improve blood circulation in brain tissue, and nootropic drugs. The rapid growth of a cyst if left untreated is a threat. In the end, the cyst compresses blood vessels and tissues; disruption of neuron nutrition causes degradation of certain brain structures, which is why cells gradually lose their functions. As a rule, stabilization of intracranial pressure and treatment of the primary disease is sufficient - the cyst gradually decreases and sometimes even disappears on its own. Unfortunately, this does not always happen and some patients require surgery. To begin with, using a special probe, a hole is formed in the wall of the cyst through which the fluid exits into the cerebral ventricle. In 80% of cases, this procedure allows you to get rid of tumors. Sometimes the hole between the walls of the cyst is still closed, and the doctor may decide that bypass surgery is necessary.
A source of information
"Pediatric Neuroradiology. Brain. Head, Neck and Spine" Author: Tortori-Donati, Paolo, Rossi, Andrea
The translation was performed by a radiologist, Ph.D. Evgeniy Aleksandrovich Vlasov, the presented drawings are diagnostic brain scans, taken from the personal archive of E.A. Vlasov. are not related to Pediatric Neuroradiology. Brain. Head, Neck and Spine" and can be found in the DICOM archive of the site.
Author: radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
If you still have doubts about the conclusions of your MRI, you can order a review of your study with a detailed transcript here:
Brain cyst (Cerebral cyst)
Arachnoid cyst
more often it is congenital or post-traumatic in nature. Located in the meninges on the surface of the brain. Filled with cerebrospinal fluid. According to some reports, up to 4% of the population have arachnoid cysts of the brain. However, clinical manifestations are observed only in the case of a large accumulation of fluid in the cyst, which may be due to the production of cerebrospinal fluid by the cells lining the cyst cavity. A sharp increase in the size of the cyst threatens its rupture, leading to death.
Pineal cyst
(pineal cyst) is a cystic formation of the epiphysis. Anecdotal evidence suggests that up to 10% of people have small, asymptomatic pineal cysts. Cysts with a diameter of more than 1 cm are observed much less frequently and can cause clinical symptoms. When it reaches a significant size, a pineal gland cyst can block the entrance to the cerebral aqueduct and block cerebrospinal fluid circulation, causing occlusive hydrocephalus.
Colloid cyst
makes up about 15-20% of intraventricular formations. In most cases, it is located in the anterior region of the third ventricle, above the foramen of Monroe; in some cases - in the IV ventricle and in the area of the transparent septum. The filling of a colloid cyst is highly viscous. The basis of the clinical manifestations are the symptoms of hydrocephalus with a paroxysmal increase in cephalgia in certain positions of the head. Behavioral disorders and memory loss are possible. Cases of weakness in the limbs have been described.
Choroid plexus cyst
is formed when cerebrospinal fluid fills the space between the individual vessels of the plexus. Diagnosed at different ages. Clinically manifested rarely, in some cases it can give symptoms of intracranial hypertension or epilepsy. Often, choroid plexus cysts are detected by obstetric ultrasound at the 20th week of pregnancy, then they resolve on their own and by approximately the 28th week of intrauterine development they are no longer detected on ultrasound.
Dermoid cyst
(epidermoid) is an abnormality of embryonic development in which the cells that give rise to the skin and its appendages (hair, nails) remain inside the brain. The contents of the cyst, along with the liquid, are represented by elements of the ectoderm (hair follicles, sebaceous glands, etc.). It is characterized by a rapid increase in size after birth, and therefore must be removed.