More about the encephalogram
The essence of the examination is to record the electrical activity of neurons in the structural formations of the brain.
An electroencephalogram is a kind of recording of neural activity on a special tape using electrodes. The latter are attached to areas of the head and record the activity of a certain area of the brain. The activity of the human brain is directly determined by the work of its midline formations - the forebrain and the reticular formation (connecting neural complex), which determine the dynamics, rhythm and construction of the EEG. The connecting function of the formation determines the symmetry and relative identity of signals between all brain structures.
The study is prescribed if there are suspicions of various disorders of the structure and activity of the central nervous system (central nervous system) - neuroinfections such as meningitis, encephalitis, poliomyelitis. With these pathologies, the activity of the brain changes, and this can be immediately diagnosed on the EEG, and in addition, the localization of the affected area can be established. An EEG is carried out on the basis of a standard protocol, which records measurements taken while awake or asleep (in infants), as well as using specialized tests.
The main tests include:
- photostimulation - exposure of closed eyes to bright flashes of light;
- hyperventilation - deep, rare breathing for 3-5 minutes;
- opening and closing eyes.
These tests are considered standard and are used for encephalograms of the brain in adults and children of any age, and for various pathologies. There are several additional tests prescribed in individual cases, such as: clenching your fingers into a so-called fist, staying in the dark for 40 minutes, depriving yourself of sleep for a certain period, monitoring night sleep, and passing psychological tests.
These tests are determined by a neurologist and are added to the main tests performed during the examination when the doctor needs to evaluate specific brain functions.
What can be assessed with an EEG?
This type of examination allows you to determine the functioning of parts of the brain in different states of the body - sleep, wakefulness, active physical, mental activity and others. EEG is a simple, absolutely harmless and safe method that does not require disruption of the skin and mucous membrane of the organ.
Currently, it is widely in demand in neurological practice, since it makes it possible to diagnose epilepsy and highly identify inflammatory, degenerative and vascular disorders in the brain. The study also provides identification of the specific location of neoplasms, cystic growths and structural damage as a result of trauma.
EEG using light and sound stimuli makes it possible to distinguish hysterical pathologies from true ones, or to identify simulation of the latter. The study has become almost indispensable for intensive care units, providing dynamic monitoring of comatose patients.
Process of studying the results
The analysis of the results obtained is carried out in parallel during the study, and during the recording of indicators, and continues after its completion. When recording, the presence of artifacts is taken into account - mechanical movement of electrodes, electrocardiograms, electromyograms, and induction of mains current fields. The amplitude and frequency are assessed, the most characteristic graphic elements are identified, and their temporal and spatial distribution is determined.
Upon completion, a patho- and physiological interpretation of the materials is made, and on its basis an EEG conclusion is formulated. Upon completion, the main medical form for this study, called the “clinical electroencephalographic report”, is filled out, compiled by the diagnostician based on the analyzed data from the “raw” recording.
The transcript of the EEG conclusion is formed on the basis of a set of rules and consists of three sections:
- Description of the leading types of activity and graphic elements.
- Conclusion after description with interpreted pathophysiological materials.
- Correlation of indicators of the first two parts with clinical materials.
The main descriptive term in EEG is “activity”, it evaluates any sequence of waves (sharp wave activity, alpha activity, etc.).
Types of human brain activity recorded during EEG recording
The main types of activity that are recorded during the study and subsequently subjected to interpretation and further study are wave frequency, amplitude and phase.
Frequency
The indicator is estimated by the number of wave oscillations per second, recorded in numbers, and expressed in a unit of measurement - hertz (Hz). The description indicates the average frequency of the activity being studied. As a rule, 4-5 recording sections of duration are taken, and the number of waves in each time interval is calculated.
Amplitude
This indicator is the range of wave oscillations of the eclectic potential. It is measured by the distance between the peaks of waves in opposite phases and is expressed in microvolts (µV). A calibration signal is used to measure the amplitude. If, for example, a calibration signal at a voltage of 50 µV is determined on a record with a height of 10 mm, then 1 mm will correspond to 5 µV. In deciphering the results, interpretations are given to the most common meanings, completely excluding rare ones.
Phase
The value of this indicator evaluates the current state of the process and determines its vector changes. On the electroencephalogram, some phenomena are assessed by the number of phases they contain. Oscillations are divided into monophasic, biphasic and polyphasic (containing more than two phases).
Rhythms of brain activity
The concept of “rhythm” in the electroencephalogram is considered to be a type of electrical activity related to a certain state of the brain, coordinated by appropriate mechanisms. When deciphering the EEG rhythm indicators of the brain, its frequency corresponding to the state of the brain region, amplitude, and its characteristic changes during functional changes in activity are entered.
Rhythms of a waking person
Brain activity recorded on the EEG in an adult has several types of rhythms, characterized by certain indicators and states of the body.
- Alpha rhythm. Its frequency remains in the range of 8–14 Hz and is present in most healthy individuals – more than 90%. The highest amplitude values are observed when the subject is at rest, in a dark room with his eyes closed. It is best identified in the occipital region. It is fragmentarily blocked or completely subsides during mental activity or visual attention.
- Beta rhythm. Its wave frequency fluctuates in the range of 13–30 Hz, and the main changes are observed when the subject is active. Pronounced fluctuations can be diagnosed in the frontal lobes under the obligatory condition of active activity, for example, mental or emotional arousal and others. The amplitude of beta oscillations is much less than alpha.
- Lambda rhythm. It has a small range - 4–5 Hz, and is triggered in the occipital region when it is necessary to make visual decisions, for example, when searching for something with open eyes. The vibrations disappear completely after concentrating your gaze on one point.
- Mu rhythm. Defined by the interval 8–13 Hz. It starts in the back of the head, and is best observed in a calm state. Suppressed when starting any activity, not excluding mental activity.
EEG is a convenient, modern and safe method for studying the brain
Electroencephalography is a convenient and simple method for assessing brain function. Like all methods based on recording biopotentials from the surface of the human body, EEG of the brain is completely safe, and is performed even on pregnant women at any stage. It is known that our nerve cells - neurons, in the process of their work, create, conduct and change the electrical current passing through them. In some ways, the way the brain works is reminiscent of the way the electrical appliances around us work. Only the current generated by neurons is extremely small, and if the current “in the socket” is measured in volts, then the current of nerve cells is measured in microvolts (which adds another “five decimal places”). Not so long ago, very large devices were used to record such small currents, and the person being examined had to be placed in a special shielded room in complete darkness, so that even the slightest influence “from outside” would not “distort” the recording of brain EEG potentials. Moreover, the first electrodes used to record EEG almost half a century ago were stuck into the skin like pins! Modern devices are so sensitive and most importantly “smart” that EEG can be recorded in almost any, almost “home” environment. It is important that a person can relax, sit (lie down) comfortably and close his eyes. Of course, everyone present during this procedure turns off their mobile phones and creates a “zone of increased silence,” however, it is no longer necessary to isolate a person in a cell; just close the window and turn off the lights.
What happens during the immediate procedure for recording an electroencephalogram ? As we agreed, a chair/chair and position are selected so that the person is as relaxed as possible. A special helmet made of silicone threads is placed on the subject’s head. It should fit tightly onto the surface of the head. The electrodes that are most often used for recording EEG in outpatient settings are called bridge electrodes; they are conveniently located, fixed using silicone threads of the helmet on the surface of the head like chess pieces. Since the brain has a fairly large surface, the researcher’s task is to record potentials evenly from the entire working (it is called convexital) surface of the brain. In order to successfully register such a weak current, the part of the electrode that is in direct contact with the skin is made of silver, and the contact site is moistened with saline solution. This is probably the only “most unpleasant” fact in the entire electroencephalography procedure: when something cold and wet is placed on the head. Although on hot summer days, subjects are usually very happy with this stage.
Next, the recording of the electroencephalogram itself begins. Depending on the clinical tasks, it can last from 5 to 20 minutes. A good rule is not only to record with your eyes closed at rest, but also to record so-called functional tests. There are three of them:
- A test with opening and closing the eyes demonstrates the brain’s reaction to an increase in the flow of information, since the person who opens the eyes involuntarily begins to examine and analyze the surrounding environment.
- A test with rhythmic photostimulation of white or red color consists of blinking a special bright lamp at a distance of 30 centimeters at different frequencies, from usually 2-4 Hz (that is, blinks per second) to 20-30 Hz. Using this test, when performing an EEG, it is possible to “catch” the so-called photoparoxysmal reactions. For example, if a person has an epileptic focus that periodically causes seizures, to prove its existence, in order to record the activity of this focus on the EEG, it must be provoked by such a flickering of light.
- Three-minute hyperventilation test - during which the subject is asked to breathe deeply, evenly (but not often!) for three minutes. With such deep breathing, even a relatively healthy person may begin to feel a little dizzy, because the brain vessels reflexively dilate, and the brain begins to experience a slight “non-dangerous” hunger. Many pathological modes of brain functioning do not manifest themselves in ordinary situations, namely under stress (fatigue, illness, emotional shock) during which, just like with three minutes of deep breathing, the brain begins to experience “slight hunger.”
Then, when the recording is completed, a functional diagnostics doctor (neurophysiologist) begins working with it. By studying the characteristics of electrical signals and their changes over time (frequency, amplitude, severity in one point of the head and “unexpressiveness” in others), the doctor can draw conclusions not only about the absence or presence of epilepsy (because EEG has long been considered the gold standard for diagnosis in epileptology) , but also about the peculiarities of brain function: for example, about the balance of excitation and inhibition, the presence of inconsistency between various brain structures, the degree of maturity of the cortex in children, and much more. Objective markers of the characteristics of the electrical work of the brain on the EEG during anxiety, nervous tension, depression, stuttering, and cerebral circulatory disorders have long been described in the literature. That is why, going beyond epileptology, EEG is successfully used not only in neurology, but also in psychotherapy and psychiatry. The standards of many examinations (when conducting medical examinations for workers in hazardous industries, when issuing driver’s licenses, when a patient consults a psychotherapist, at the beginning of a neurologist’s examination of a person with a headache, etc.) include EEG of the brain as one of the first diagnostic methods.
EEG does not require any special preparation other than a “clean head” (without hairspray or other hair styling products)!
An EEG of the brain can be done for a fee at our center every working day. Tel for inquiries and appointments 246-11-51
Rhythms in sleep
A separate category of types of rhythms that manifest themselves either in sleep conditions or in pathological conditions includes three varieties of this indicator.
- Delta rhythm. Characteristic of the deep sleep phase and for comatose patients. It is also recorded when recording signals from areas of the cerebral cortex located on the border with areas affected by oncological processes. Sometimes it can be recorded in children 4–6 years old.
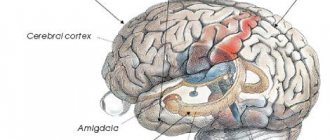
- Theta rhythm. The frequency interval is within 4–8 Hz. These waves are triggered by the hippocampus (information filter) and appear during sleep. Responsible for high-quality assimilation of information and forms the basis of self-learning.
Based on the results obtained during EEG recording, an indicator is determined that characterizes a complete all-encompassing assessment of the waves - bioelectrical activity of the brain (BEA). The diagnostician checks the EEG parameters - frequency, rhythm and the presence of sharp flashes that provoke characteristic manifestations, and on these grounds makes a final conclusion.
4.2.3. Bioelectric activity of the brain
The specificity of the spatiotemporal organization of the rhythmic components of the EEG, the analysis of background and evoked electrical activity of the brain make it possible to identify the nature of the functional maturation of subcortical structures and certain parts of the cortex in different age periods. Thus, a decrease in the theta rhythm in the EEG with age indicates a decrease in the role of nonspecific subcortical structures in the genesis of bioelectrical activity. The increase in the severity of the main rhythm of bioelectrical activity - the alpha rhythm and the formation of its spatial organization reflects the maturation of the cerebral cortex.
Analysis of the electrical activity of the brain revealed that in the early postnatal period the most functionally mature are the mesodiencephalic structures of the brain, which belong to the first functional block of the brain (Novikova L. A. et al., 1975).
The main periods that can be characterized as turning points in the dynamics of changes in the alpha rhythm are 6 years, 9-10 years. During puberty (12-14 years), regressive deviations in the EEG occur due to an increase in the power of theta activity. Spatial synchronization of resting EEG rhythms, characteristic of adults, is formed at the end of this period. This reflects the formation of a mature type of structural and functional organization of the brain, characteristic of a state of quiet wakefulness (Alferova V.V. et al., 1990).
The work of the first functional block of the brain is associated with two main types of activation:
1) general, generalized, addressed to the entire brain (provided by the subcortical sections of the first block of the brain and underlies functional states);
2) specific, local, directed to specific structures (provided by the cortical sections of the first block of the brain and serves as the basis for the implementation of mental functions) (Khomskaya E.D., 2002).
Major changes in the brain's activation system also occur gradually. Initially, a generalized form of brain activation is recorded. By the age of 7-10 years, a transition occurs from a generalized to a regionally specific form of activation. At 11-14 years of age, regressive dynamics in the functioning of the regulatory system are observed, associated with changes in the hormonal profile of the body. From the age of 14-15 years, the reactivity of the activation system is restored and the nature of its functioning approaches the adult level (Gorev A.S., 1990).
The central sections of the analyzing systems are located in the second functional block of the brain. All analyzing systems are capable of functioning from the first days of a child’s life, but by the time of birth, remote analyzers are the least ready.
The formation of the visual system is currently best analyzed.
According to psychophysiological data, significant changes in visual perception occur in the period from 3-4 to 6-7 years.
Evoked potentials (EPs) in the projection cortical area to simple and formalized visual stimuli, which are found in a newborn child, are initially local in nature and can be regarded as a sensory-specific response. They reflect the presence of sensation and the possibility of primary analysis of the stimulus.
By the end of the first year of life, the structure of EP becomes close to that of an adult; by the age of five, the time parameters of the evoked response (latency period and duration of individual phases) also decrease.
At 3-4 years of age, the structure of EP in the caudal areas of the cortex has a similar character in response to complexly structured stimuli. This may indicate that the projection cortex and posterior associative areas (zone TGJ) are equally involved in their analysis, that is, the posterior associative areas, as well as the primary fields, perform a sensory function, duplicating the function of the projection zone.
After 5-6 years, the structure of the evoked potential in the TPO becomes not always similar to the structure of the EP in the projection zone. This corresponds to psychological and psychophysiological data, according to which at the age of 5-7 years, significant shifts in visual perception occur, associated with facilitation of the process of developing standards, including complex, previously unfamiliar stimuli.
Decoding of electroencephalogram indicators
In order to decipher the EEG and not miss any of the smallest manifestations in the recording, the specialist needs to take into account all the important points that may affect the indicators being studied. These include age, the presence of certain diseases, possible contraindications and other factors.
Upon completion of the collection of all research data and their processing, the analysis is completed and then a final conclusion is formed, which will be provided for making a further decision on the choice of therapy method. Any disturbance in activity may be a symptom of diseases caused by certain factors.
Alpha rhythm
The normal frequency is determined in the range of 8–13 Hz, and its amplitude does not go beyond 100 μV. Such characteristics indicate a healthy state of a person and the absence of any pathologies. The following are considered violations:
- constant fixation of the alpha rhythm in the frontal lobe;
- exceeding the difference between the hemispheres by up to 35%;
- constant violation of wave sinusoidality;
- presence of frequency dispersion;
- amplitude below 25 μV and above 95 μV.
The presence of disturbances in this indicator indicates a possible asymmetry of the hemispheres, which may be the result of oncological tumors or pathologies of cerebral circulation, for example, stroke or hemorrhage. A high frequency indicates brain damage or TBI (traumatic brain injury).
A complete absence of the alpha rhythm is often observed in dementia, and in children, deviations from the norm are directly related to mental retardation (MDD). Such a delay in children is evidenced by: disorganization of alpha waves, shift of focus from the occipital region, increased synchrony, short activation reaction, overreaction to intense breathing.
These manifestations can be caused by inhibitory psychopathy, epileptic seizures, and a short reaction is considered one of the primary signs of neurotic disorders.
Beta rhythm
In the accepted norm, these waves are clearly detected in the frontal lobes of the brain with a symmetrical amplitude in the range of 3–5 μV, recorded in both hemispheres. A high amplitude leads doctors to think about the presence of a concussion, and when short spindles appear, to the occurrence of encephalitis. An increase in the frequency and duration of spindles indicates the development of inflammation.
In children, the pathological manifestations of beta oscillations are considered to be a frequency of 15-16 Hz and a high amplitude present - 40-50 µV, and if its localization is the central or anterior part of the brain, then this should alert the doctor. Such characteristics indicate a high probability of delayed development of the baby.
Delta and theta rhythms
An increase in the amplitude of these indicators above 45 μV on a constant basis is characteristic of functional brain disorders. If the indicators are increased in all brain regions, then this may indicate severe dysfunction of the central nervous system.
If a high amplitude of the delta rhythm is detected, a tumor is suspected. Inflated values of the theta and delta rhythm recorded in the occipital region indicate a child’s lethargy and a delay in his development, as well as impaired circulatory function.
EEG in psychiatry and neurology
The EEG is an extremely sensitive voltmeter. Typical EEG signals fluctuate over a wide range. Electrical potentials measured between any two EEG electrodes fluctuate rapidly, usually many times per second. These EEG signals are the result of net field potentials generated by excitatory and inhibitory postsynaptic potentials in vertically oriented cortical pyramidal cells.
The EEG of an awake and relaxed healthy adult typically exhibits predominant frequencies of 8 to 13 oscillations per second (8 to 13 Hz alpha activity). As soon as a person focuses their attention on something or experiences stress, the frequency increases to the beta range (above 13 Hz). When an adult begins to experience feelings of sleepiness, EEG rhythms slow down to the theta band (4 to 8 Hz) and finally to the delta band (below 4 Hz) during sleep. The appearance of high-amplitude theta or any delta during wakefulness is a definite pathology. Excessive beta activity during wakefulness is associated with anxiety disorders, it is not considered an EEG abnormality (by modern standards) and cannot be used to diagnose anxiety conditions.
The prevalence of EEG abnormalities in psychiatrist patients is significantly increased and ranges from 20% to 68%. EEG findings in psychiatric populations include generalized or focal slowing of cortical activity and various focal or generalized paroxysmal bursts on the EEG. One reason that these patients have such a wide range of EEG abnormalities may be due to the fact that the EEG signal is quite sensitive to many variables (eg, metabolic, vascular, endocrine, etc.) that affect CNS function. In addition, EEG discharges without overt seizures (i.e., isolated epileptic discharges) may have psychopathological manifestations such as emotional lability, irritability, or impaired impulse control.
Most often, two types of abnormalities are detected on the EEG: a slowdown of normal rhythms and the appearance of abnormal paroxysmal (episodic) electrical activity, suggestive of an epileptic process. Both types of abnormalities may be focal and suggestive of a localized disease process, or generalized and more diffuse, suggestive of a degenerative or metabolic process. If slowing is suspected, the patient should remain awake during the EEG recording; if paroxysmal activity is suspected, an EEG should be performed both during sleep and while awake.
Borderline personality disorder
Studies have shown that in patients with borderline personality disorder the frequency of significant and less severe EEG abnormalities is significantly higher than in patients with dysthymic disorder. Abnormalities (mainly slowing of cortical activity) were most often bilateral and had a frontal, temporal, or frontotemporal distribution. Patients with borderline personality disorder have been found to have a much higher prevalence of symptoms typically seen in complex partial seizures or episodic loss of control than patients with unipolar depression. Similarly, in patients with borderline personality disorder, the prevalence of paroxysmal EEG activity was significantly higher, particularly manifesting as sharp posterior waves (indicative of an epileptic profile).
Autism Spectrum Disorders
Epilepsy is common in children with autism spectrum disorder (ASD). A significant proportion of children with autism have abnormal EEGs, even those who have never had a seizure. EEG abnormalities can range from mild slow abnormalities to frank epileptiform discharges (epileptiform discharges may only be detected during sleep and may sometimes require long-term monitoring).
The question of whether therapeutic treatment has an effect on the elimination of EEG peaks and psychopathological symptoms in children with pervasive developmental disorders and autism remains open.
Panic disorder
The most common mental disorder that should be distinguished from temporal lobe epilepsy is panic disorder. Here the seizures were shorter and more stereotypical than panic attacks. In addition, aphasia and dysmnesia accompanied seizure activity in some patients. This differentiation can be diagnostically challenging because patients with documented complex partial seizures of temporal origin may have associated nonictal episodic emotional symptoms, including phobia, true panic attacks, and anxiety.
The researchers compared the symptoms of panic disorder-agoraphobia with those of complex partial seizures. Because of the similarities, they concluded that both disorders may share a common neurophysiological substrate.
Aggression
The prevalence of abnormal EEGs in aggression varies widely, from 6.6% in patients with rage and episodic violent behavior to 53% in patients with antisocial personality disorder. Anticonvulsants can block epileptiform EEG secretions and can lead to significant clinical improvement in individuals exhibiting aggressive behavior. Addition of carbamazepine for the treatment of patients with “violent schizophrenia” with repeated violent episodes who also demonstrate temporal lobe abnormalities on EEG but who do not have a history of seizure disorder. have shown their effectiveness. Other studies suggest that anticonvulsant therapy may have a beneficial effect on aggressive tendencies regardless of the presence or absence of EEG abnormalities.
ADHD
Most patients with ADHD respond positively to psychostimulants. Therefore, EEG may be useful when there is no response to treatment. A number of studies have identified variable rates of EEG abnormalities in children with ADHD. In 9% of children, abnormalities with background slowing of electrocortical or paroxysmal discharges were detected. In another study, in a sample of children with ADHD, 31% had abnormal routine EEGs. Of the children with abnormal EEGs, 84% had bursts or spikes; others had excessive cortical slowing. Some authors have reported a 7% incidence of certain abnormalities suggestive of a seizure disorder and an additional 19% of mild abnormal breathing abnormalities that are not diagnostic of a seizure disorder in children with ADHD.
Atypical bipolar disorder with rapid cycling
The researchers reported a 7% incidence of specific abnormalities suggestive of a seizure disorder and an additional 19% of mildly abnormal breathing abnormalities not diagnostic of a seizure disorder in children with ADHD.
Decoding values in different age intervals
An EEG recording of a premature baby at 25–28 gestational weeks looks like a curve in the form of slow flashes of delta and theta rhythms, periodically combined with sharp wave peaks 3–15 seconds long with a decrease in amplitude to 25 μV. In full-term infants, these values are clearly divided into three types of indicators. During wakefulness (with a periodic frequency of 5 Hz and an amplitude of 55–60 Hz), the active phase of sleep (with a stable frequency of 5–7 Hz and a fast low amplitude) and quiet sleep with flashes of delta oscillations at a high amplitude.
Over the course of 3-6 months of a child’s life, the number of theta oscillations is constantly growing, while the delta rhythm, on the contrary, is characterized by a decline. Further, from 7 months to a year, the child develops alpha waves, and delta and theta gradually fade away. Over the next 8 years, the EEG shows a gradual replacement of slow waves with fast ones - alpha and beta oscillations.
Until the age of 15, alpha waves predominate, and by the age of 18, the BEA transformation is complete. Over the period from 21 to 50 years, stable indicators remain almost unchanged. And from 50, the next phase of rhythmicity restructuring begins, which is characterized by a decrease in the amplitude of alpha oscillations and an increase in beta and delta.
After 60 years, the frequency also begins to gradually fade, and in a healthy person, manifestations of delta and theta oscillations are noticed on the EEG. According to statistics, age indicators from 1 to 21 years, considered “healthy,” are determined in subjects 1–15 years old, reaching 70%, and in the range of 16–21 – about 80%.
In what cases is an EEG of the brain done?
Electroencephalography is done after concussions or if cyst formation is suspected. Studies are indicated for neurological manifestations in the form of numbness in the arms, legs, and sudden fainting. An EEG is also done for hypertension.
Electroencephalography is not done during an exacerbation of respiratory diseases or with a stuffy nose.
How does EEG equipment work?
EEG equipment is connected to electrodes that read any impulses. At the same time, the information is transmitted to the encephalograph. It contains programs that process incoming signals.
How is the procedure performed?
To conduct an EEG, the doctor puts a special device on the patient’s head. It has built-in electrodes, the number of which depends on the age of the patient. For children under 18 years of age, 12 are used, for adults - 20 and one unpaired one, which is applied to the crown. If epilepsy is suspected, the doctor attaches separate additional sensors to the temporal region.
The electrodes are lubricated with a special substance that quickly conducts electricity. They are connected to the electroencephalograph by wires. When you turn on the device, the electrodes first amplify the signals that come from the brain. The pulses are then transmitted to a computer for further processing.
During the procedure, the signals are displayed on the monitor as a wave-like line. This allows doctors to immediately determine cell activity. Information on the monitor simultaneously indicates foci of inflammation, tumors and areas where organ function is impaired. The duration of the procedure is up to 10 minutes.
Preparation for the procedure
Before the EEG, you must wash your hair thoroughly. Do not use styling products (foam, varnish, etc.). Before the procedure, all metal objects (piercings, hair clips, etc.) are removed. Two days before the EEG, you need to stop drinking alcohol and drinks that stimulate the nervous system. Chocolate is excluded from the diet.
Before the EEG procedure, you must inform the doctor about taking medications (sleeping pills, anticonvulsants, etc.). If it is impossible to suspend treatment during decoding, notes are made about the use of specific medications. You cannot eat or smoke 2 hours before the procedure.
Rhythms of activity
The final result of electroencephalography is derived from biorhythms at different periods, depending on the situation. Characteristics of the main signals of brain activity:
The alpha rhythm (9-13 Hz, with an oscillation amplitude of 5-100 μV) is present in almost every healthy person during rest. As soon as the eyes open and visual images begin to enter the brain, the a-rhythm decreases. With a further increase in the activity of the organ, the signals disappear completely. The fading of signals is caused by stress, fear, and activation of the nervous system.
The beta rhythm (13-39 Hz with an oscillation amplitude of up to 20 μV) appears during active thought processes. Normally, the waves are quite weak; their excess indicates the brain's response to stress.
The theta rhythm (4-8 Hz, with an oscillation amplitude of 20-100 μV) reflects slow consciousness (drowsiness, half-sleep). In a healthy person, when falling asleep, the theta rhythm increases in quantity. Mental disorders, concussions, and neurological diseases also contribute to wave amplification. The theta rhythm increases during twilight states and heavy emotional stress.
The delta rhythm (0.3-4 Hz, with an oscillation amplitude of 20-200 μV) indicates deep sleep or immersion in anesthesia. As neurological diseases progress, the waves intensify.
In addition to those listed, there is a gamma rhythm with a frequency of up to 100 Hz. The kappa rhythm is formed in the temporal regions when mental activity is observed. The mu rhythm indicates mental stress. These waves are not of great importance in diagnosis, since they usually appear in a state of overstrain of brain activity, where a high concentration of attention is required.
Carrying out electroencephalography in children
EEG in children is performed in the first year of life during sleep. The procedure helps to assess the state of the brain and analyze its development at the cellular level. At the same time, abnormalities are identified that can be treated before they begin to progress into serious diseases.
The most common diagnosed pathologies
Thanks to the electroencephalogram, diseases such as epilepsy or various types of traumatic brain injury (TBI) are quite easily diagnosed.
Epilepsy
The study allows you to determine the localization of the pathological area, as well as the specific type of epileptic disease. At the time of a convulsive syndrome, the EEG recording has a number of specific manifestations:
- pointed waves (peaks) - suddenly rising and falling can appear in one or several areas;
- the combination of slow pointed waves during an attack becomes even more pronounced;
- sudden increase in amplitude in the form of flashes.
The use of stimulating artificial signals helps in determining the form of epileptic disease, since they provide visibility of hidden activity that is difficult to diagnose with EEG. For example, intense breathing, requiring hyperventilation, leads to a decrease in the lumen of blood vessels.
Photostimulation is also used, carried out using a strobe (a powerful light source), and if there is no reaction to the stimulus, then most likely there is a pathology associated with the conduction of visual impulses. The appearance of non-standard vibrations indicates pathological changes in the brain. The doctor should not forget that exposure to powerful light can lead to an epileptic seizure.
When is EEG indicated for children?
The technique allows you to determine the state of the baby’s nervous system. It is based on the transmission of electrical impulses by neurons that create bioelectrical activity in the brain. What is it - EEG for children? The electroencelograph displays the received information in the form of curved lines during different periods of activity. If the doctor has sent your child for examination, you should not refuse to conduct the examination. It is painless and at the same time quite informative for identifying brain pathologies of various types.
The doctor prescribes an EEG for the child in the following cases:
- with periodically recurring loss of consciousness;
- if the child falls out of reality;
- after moderate traumatic brain injury;
- in an epileptic clinic;
- persistent sleep disorders;
- if oncological processes are suspected;
- to monitor the rehabilitation process after undergoing neurosurgery;
- in case of congenital pathology (eg hydrocephalus);
- for cerebrovascular accidents;
- for disorders in the neurological status (cerebral palsy, other motor disorders);
- for autism spectrum disorders;
- developmental delay, both in the mental and physical spheres.
Electroencephalography shows the localization of foci of epileptiform activity, the degree and dynamics of the disease, and the effectiveness of the selected therapy. Therefore, the scope of its application is very wide.
Sometimes the doctor sends the child for an EEG even in the absence of certain somatic pathologies. Indications for its implementation are deviations in behavior, development inappropriate for age, poor memory and lack of concentration, hyperactivity. At school age, in case of excessively rapid fatigue, an electroencephalogram of the brain may also be prescribed for children.
The method is widely used to diagnose epilepsy.