Femoral nerve damage
The femoral nerve is formed from the roots of the lumbar spinal cord, mainly from the fibers of the third lumbar root. The nerve provides activity to the iliopsoas and quadriceps femoris muscles, as well as sensitivity to the skin of the anterior and inner surface of the thigh, lower leg and foot.
Dysfunction of the nerve is usually associated with its compression in the retroperitoneal space or at the point of its exit to the thigh - behind the inguinal ligament, near the capsule of the hip joint.
The most common causes of femoral nerve compression are:
- injuries complicated by the formation of a retroperitoneal hematoma
- pathological processes in the retroperitoneal space: tumors, abscesses
- pathology of the hip joint: dislocation of the femoral head, severe hypermobility of the joint, fracture of the femoral neck
- complications after hip surgery and kidney transplantation.
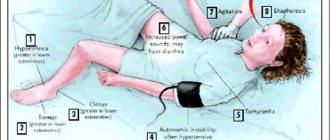
When the femoral nerve is damaged, the patient complains of pain and a crawling sensation, tingling in the lower two-thirds of the anterior surface of the thigh and on the anterior inner surface of the leg and foot. These sensations are initially mild and appear periodically, then they become constant, causing the patient significant discomfort. Later, sometimes after several months or even years, sensitivity in the corresponding areas decreases, which, most often, patients describe as numbness. Subsequently, in the absence of treatment, weakness of the muscles innervated by the femoral nerve gradually develops. Weakness of the iliopsoas muscle causes difficulty in hip flexion.
Weakness, as a rule, is not very pronounced, since the muscle is innervated by several nerves, and damage to only the femoral nerve does not always affect the work of the entire muscle and is often unnoticed by the patient in everyday life. The exception is athletes, for whom it is extremely important that every muscle works with full efficiency. If the nerve is affected at a level passing below the inguinal ligament, then very often the function of the iliopsoas muscle is completely preserved. Much more noticeable for the patient is weakness of the quadriceps femoris muscle, which is manifested by difficulty bending the leg when climbing stairs, running, and jumping.
During a neurological examination, if the femoral nerve is damaged, a decrease in the knee reflex is detected, as well as symptoms of nerve tension - Wasserman's symptom and Matskevich's symptom.
Get a free consultation by phone
Femoral nerve neuropathy
Damage (neuropathy, neuritis) of the femoral nerve is a serious disease that leads to significant discomfort. The main danger associated with this phenomenon is the inability to transmit impulses along the nerve. As a result of this pathology, a person experiences serious pain, as well as sensory disorders. In the absence of timely treatment, this pathology can lead to serious negative consequences in the form of difficulties during movement.
The anomaly in question is most often associated with muscle spasm leading to compression. The cause may also be a process of hemorrhage in the psoas muscle. This may be the result of a physical injury, or due to significant and regular overload. Hematomas and tumors can also lead to this problem. Quite often, athletes or people whose profession is directly related to heavy physical labor and regular weight lifting encounter this pathology.
Clinical picture
Patients may have symptoms such as pain, burning, numbness, coldness, or itching in the anterolateral thigh. As mentioned earlier, the LCNB provides sensory innervation to the skin of the anterolateral and lateral aspects of the thigh. Therefore, a patient with PM will experience symptoms in this part of the hip (both superficial and deep).
A person may have mild pain that resolves spontaneously or more severe pain that limits function. Patients may report pain with prolonged standing or walking. The pain may be relieved by sitting because this position reduces the tension on the LCL or inguinal ligament. This decrease in tension may be associated with a decrease in symptoms. Each patient will have a specific clinical presentation and distribution of symptoms.
Femoral nerve neuropathy, diagnosis
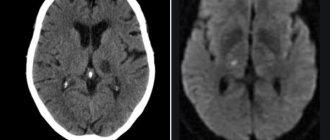
In order to correctly make a diagnosis, a specialist neurologist needs to carefully study the features of the existing problem with which the patient came in. Most often we are talking about painful discomfort during movement. In order to get a complete picture, it is mandatory to conduct an x-ray of the vertebral part of the body. Having studied the received images, the attending physician has the opportunity to obtain maximum information regarding the patient’s health condition. In the future, this will allow you to formulate the correct treatment and achieve the fastest and most effective recovery.
In difficult cases, when there is a need to verify the diagnosis, an examination such as an EMG may be prescribed. With its help, you can determine the speed of impulses passing along the thigh nerve, as well as record a number of other signs that facilitate diagnosis.
Causes of Roth-Bernhardt syndrome and methods of its treatment
Roth Bernhardt's disease was first described by the Russian scientist Roth and the German Bernhardt at the end of the 19th century. Another name is myalgia paresthetica. The disease is a compression of the lateral nerve of the skin of the thigh. The external nerve is a conductor of impulses from the outer and posterior zones of the thigh, ending near the knee. The nerve may have anatomical pathology. The disease itself is caused by abnormal structural features of the hip; it can be unilateral and in 20% of cases bilateral.
Factors leading to illness
Factors influencing congenital disorders:
- Manifestation of the disease in the area of attachment of the inguinal ligament to the bone due to poor blood circulation.
- The appearance of a canal when the groin ligament bifurcates, where the nerve is pinched.
- Congenital sharp fracture of the nerve.
- Nerve close to the ilium, etc.
In addition to congenital, the disease can be acquired and manifests itself with age. This is facilitated by:
- Pressure on the lateral nerve caused by wearing tight clothing or a belt;
- Pregnancy, as the forward curve of the spine increases and the inguinal ligament becomes tense;
- Excess body weight, where the most problem areas are the stomach and thighs;
- Hernias in the groin;
- Neoplasms in the abdominal area;
- Pathological fluid in the abdominal cavity;
- Hematomas in the retroperitoneal region;
- Swelling and increased tissue size associated with surgical procedures or inflammation;
- Diabetes, lack of microelements, typhoid fever and other diseases in acute and chronic forms;
- Rachiocampsis
. _
Signs of Roth Bernhardt's disease
Signs of the disease become obvious from the first moments of compression of the external nerve. Patients complain of:
- Burning;
- Numbness;
- Decreased sensitivity;
- Cold;
- The appearance of ulcers;
- Acute painful sensations;
- Skin inflammation;
- Intermittent claudication that occurs with physical activity and disappears when the person is immobile.
Ways to determine the disease
It is not difficult to identify a disease, but you need to find its root cause, on which treatment will depend. First, data is collected about the patient’s well-being and his complaints, then a visual and palpation examination is carried out. In order to make an accurate diagnosis, the following methods are used:
- Electroneuromyography is used to assess muscle activity in response to a stimulus.
- Ultrasound helps determine the area where the nerve is torn and other abnormalities.
- MRI is prescribed to obtain a three-dimensional image of the area in any projection. Most often it is performed when there is a suspicion of the presence of neoplasms and internal hematomas.
- CT also provides reliable information, but with the use of X-rays.
- X-ray of the spine.
- Autoimmune and biochemical blood tests.
If, after eliminating the obvious cause of the disease, the patient continues to complain of malaise, additional examinations are prescribed.
How is Roth-Bernhardt disease treated?
To cure the disease, a set of therapeutic and preventive measures are used to improve well-being and eliminate pressure on the nerve.
Medicines are prescribed for:
- Relieving inflammation. For this, non-steroidal anti-inflammatory drugs like Diclofenac, Indomethacin, etc. are used.
- Pain relief in the form of ointments, tablets or injections.
- Improves blood circulation.
- Obtaining the necessary elements. For this purpose, vitamin complexes are prescribed, especially those containing B12 and B1 and the minerals Mg, Ka, Cal, necessary for the heart.
- Vasodilation using Nicotinic acid, Trental, etc.
- For severe acute pain, hormonal drugs such as Prednisolone, Dexamitozone, etc. are recommended.
Physiotherapeutic treatment is prescribed in the form of:
- Hydrogen sulfide baths;
- Wraps;
- Mud treatment;
- Water massage;
- Magnetic laser procedures;
- UHF;
- Acupuncture.
The measures taken inhibit the inflammatory process, relieve pain, and improve blood flow to tissues and cells.
Gymnastic exercises have a positive effect on recovery. The most productive block is carried out daily for 15 minutes, including the following exercises:
- The patient sits with his legs bent. Using sliding movements along the flooring, you need to straighten your lower limbs. Perform five times in two approaches.
- The patient's position is to lie on his stomach. The hands are placed on the lumbar region. Raises the shoulders along with the head, lifting them off the floor at a slow pace three times. Do it twice.
- The patient stands with his hands on his belt. Spreads his legs at a slow pace, sliding and leaving his feet on the floor. Performs four times, taking a 15-second pause between approaches.
- The patient lies on his stomach and performs arm movements six times as with the breaststroke technique.
- The patient lies on the side opposite the patient. The head is placed on the arm bent at the elbow. Raises the straight leg to a painless maximum about eight times.
During treatment, the patient is advised to:
- Refrain from uncomfortable clothes, replacing them with loose-fitting models, avoiding belts.
- Eat foods rich in microelements and vitamins, adhere to a proper sleep schedule.
- Monitor your weight, if it exceeds the norm, adjust your diet and increase physical activity.
For tumors and large-scale hematomas, operations to remove them are indicated, where a positive outcome predetermines the timely surgical manipulation.
To reach the nerve, a shallow incision is made in the skin under local anesthesia. If the operation is delayed, the growing death of nerve cells will interfere with recovery. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Treatment of the femoral nerve
After the final determination of the type of disease, the need arises to formulate a treatment course. Most often, therapeutic measures are aimed at reducing the inflammatory process, effective pain relief (femoral nerve block under ultrasound) and eliminating swelling using manual therapy and hydrotherapy methods. In some cases, it is acceptable to use physical therapy as an effective tool in the fight against the pathology in question. But it should be noted that this option is appropriate only when the disease is not advanced. After all, many patients seek professional help at serious stages of neuropathy (neuritis) of the femoral nerve, when the symptoms are quite pronounced, but this is not a difficulty for the specialists of the AndroMeda clinic.
In some cases, the only correct solution is surgical intervention for pinched femoral nerve. To do this, the attending physician must carefully examine the patient’s condition, determine the stage of development of the pathology, study his chronic diseases, and also assess his general physical condition. Surgery is most often prescribed for serious sports and other injuries, when the damage is of the most serious nature. But for this it is necessary to conduct a full examination of the body in order to gain confidence that the surgical intervention will not be harmful to the patient.
Rehabilitation is quite an important point. Patients need to pay great attention to restorative practices and follow all doctor’s orders. This will strengthen the body and restore health.
Grade
Sequential study of medical history
- PM is characterized by the presence and history of various symptoms mentioned in the “Clinical presentation” section.
Physical examination
- Palpation of the lateral part of the inguinal ligament (where the nerve crosses the inguinal ligament) is usually painful. Some patients also experience hair loss in the LCNB area because they constantly rub the area.
Additional tests
- To rule out red flags, an x-ray of the pelvic bones is performed (to rule out tumors). When a metabolic cause is suspected, blood tests and thyroid function tests are performed.
Types of tunnel syndrome
The syndrome can manifest itself in several generally accepted forms.
- In the median nerve:
- carpal tunnel syndrome (carpal tunnel, carpal tunnel);
- pronator syndrome (Seyfarth syndrome, “newlywed (honeymoon, lovers) paralysis");
- supracondylar syndrome (Coulomb, Lord and Bedosier syndrome, Straser's band syndrome).
- In the ulnar nerve:
- Guyon's syndrome (Guyon's bed syndrome, ulnar carpal syndrome, compression-ischemic neuropathy of the distal part of the ulnar nerve);
- cubital syndrome (ulnar tunnel syndrome, compression neuropathy of the ulnar nerve in the cubital canal, late ulnar-cubital traumatic palsy).
- In the radial nerve:
- syndrome of compression of the radial nerve in the armpit (“crutch paralysis”);
- syndrome of compression of the radial nerve in the middle of the shoulder (spiral canal syndrome, “Saturday night paralysis”, “park bench”, “bench” syndrome);
- compression syndrome of the radial nerve in the subulnar area (“tennis elbow”, compression neuropathy of the posterior branch of the radial nerve in the subulnar area, supinator syndrome).