The functioning of the organs and systems of our body is regulated by nerve impulses - signals emanating from the brain. “Outgoing” and “incoming” impulses are transmitted along the nerves, as if through wires. Damage to the nerves disrupts this connection and can cause serious disruptions in the body's functioning. Indeed, along with disruption of nerve transmission in the affected area, cellular nutrition and blood supply deteriorate.
A condition characterized by damage to nerve fibers and accompanied by a violation of the conduction of nerve impulses along the nerve fiber is called neuropathy (neuropathy) .
If one nerve suffers, we are talking about mononeuropathy , if there is multiple symmetrical damage to peripheral nerves (for example, when the process affects both lower and/or upper limbs at once, etc.) - about polyneuropathy . The pathological process can involve both cranial and peripheral nerves.
Lesions of the peripheral nerve trunks, which are based on the infringement of a nerve enlarged as a result of inflammation and swelling in the muscle-bone tunnel, are called tunnel syndrome (there is also a name for compression-ischemic neuropathy ).
There are dozens of tunnel syndromes, the most famous of which is carpal tunnel syndrome.
1
Neuropathy. Diagnosis and treatment.
2 Neuropathy. Diagnosis and treatment.
3 Neuropathy. Diagnosis and treatment.
Causes of neuropathy
To date, the exact cause of neuropathy has not been established. The appearance and development of the disease is affected by many factors, such as diabetes, HIV infection, chronic alcoholism, organic diseases, and external factors. In addition, there are forms of hereditary pathology associated with genetic defects.
Internal pathologies that can affect the development of neuropathy:
- endocrine diseases;
- avitaminosis;
- autoimmune diseases;
- multiple sclerosis;
- rheumatoid arthritis.
External factors include:
- injuries;
- intoxication;
- infections;
- alcoholism.
Depending on the causes of occurrence, neuropathy is classified:
- post-traumatic - appears as a result of injuries to the nerve fiber and its branches (bruises, cuts, dislocations, fractures). In most clinical cases, this form of the disease affects the ulnar nerve, facial, sciatic, and nerves of the lower extremities;
- diabetic – develops in diabetes mellitus;
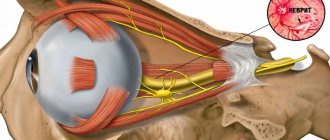
- ischemic - develops as a result of compression of nerve bundles in the spine or muscle-bone joints; As a result, the blood supply to the nerve endings is disrupted. Develops against the background of vascular diseases and large blood loss. In most cases, the optic nerve is affected;
- alcoholic – occurs due to the consumption of large doses of alcohol, the breakdown products of which complicate the metabolic process.
Treatment
Mandatory basic conditions of therapy are cessation of alcohol consumption and normalization of nutrition. Since the disease develops in the later stages of alcoholism, hospitalization in a narcological hospital is often required for complex detoxification and recovery measures. Drug therapy includes the following areas:
- Elimination of pain syndrome. In the treatment of neuropathic pain, the use of anticonvulsants and antidepressants is effective: amitriptyline, venlafaxine, duloxetine, galapentine and pregabalin. Medicines of these groups can be prescribed either separately or simultaneously.
- Eliminate oxidative stress. Alpha lipoic acid preparations reduce the amount of free radicals in tissues and stimulate the production of endogenous antioxidants. Medicines improve blood supply to nerves and nerve conduction, which reduces motor and sensory disorders.
- Correction of hypovitaminosis. B vitamins have affinity for nervous tissue and are widely used in the treatment of diseases of the nervous system. Promote regeneration, activate local metabolism and accumulation of magnesium, which plays an important role in the metabolic processes occurring in nerve cells.
Along with drug therapy, massage and exercise therapy are recommended. Regular exercise therapy prevents the development of contractures and muscle atrophy, allows you to maintain and improve motor skills, increase your ability to work, and improve your ability to self-care.
The patient is explained the causes of alcoholic neuropathy and the importance of maintaining a sober lifestyle to prevent the progression of the disease. Working with a psychologist and participating in groups helps a person cope with feelings, stabilize their emotional state and firmly take the path of abstinence. The method of treating alcoholism is selected individually. Psychological or medicinal coding is possible.
If you stop drinking alcohol, the prognosis is quite favorable. At the height of the disease, the impairments become so pronounced that sometimes a second disability group . Later, in mild cases, the symptoms disappear completely. In severe cases, residual manifestations persist in the long-term period, which do not have a significant effect on work ability or slightly limit it. Drinking alcohol or poor nutrition can trigger a relapse of the pathology.
Symptoms of neuropathy
The clinical picture of the disease can be very different and affect any place in the body. Depending on the nature of the lesion, neuropathy is divided into:
- sensory – impaired sensitivity of the affected organ. The patient may feel numbness of the limbs, tingling, crawling without causing irritation, burning, pain, unsteadiness of gait;
- peripheral - a violation of the conduction of impulses from the central nervous system to organs that are connected to the affected nerve fibers. Accompanied by tingling and tingling at the site of the damaged nerve, numbness of the limbs, decreased sensitivity to pain and temperature changes. Expressed by burning pain, loss of balance, loss of coordination;
- motor – defective motor activity. With this form, a decrease in sensitivity is not observed. The patient unintentionally makes uncontrolled movements of the limbs, muscle reflexes partially disappear, and muscle weakness gradually begins to appear. Accompanied by pain and, at the initial stage, convulsions;
- autonomous - affects internal organs. It is considered the most dangerous, because As the disease progresses, the functioning of certain organs and systems is disrupted. The function of swallowing, urination, and defecation may be impaired.
The disease manifests itself in different ways, the most characteristic symptoms are:
- impaired sensitivity of the damaged area;
- pain syndrome of varying severity and intensity;
- muscle weakness;
- spasms and cramps;
- difficult movements.
Diagnostics
Neuropathy is considered a rather difficult disease to diagnose. The disease may not make itself felt for a long time and may not manifest itself with certain symptoms. Therefore, the doctor needs to collect a complete history to make a correct diagnosis.
At the appointment, it is important for the patient to tell the neurologist about their lifestyle, whether they took medications and what kind, whether they had viral diseases, whether there are chronic and hereditary pathologies, whether surgical treatment was performed. After an oral interview, the doctor examines the patient and palpates the nerve trunks, identifying pain and thickening along their course. Tapping is carried out along the nerve endings and tingling sensations are detected in the sensitive area. Next, the patient needs to undergo a series of instrumental studies and laboratory tests:
- clinical and biochemical blood test;
- elastography;
- ultrasonography;
- CT scan;
- electromyography;
- MRI and X-ray;
- consultation of related specialists (ophthalmologist).
Numerous and confusing anatomical variants of the peripheral nervous system make it difficult to understand its structure, so only a highly qualified specialist can diagnose the disease. The best neurologists with many years of practice work in our center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency. Modern equipment and our own clinical diagnostic center allow us to quickly and accurately identify the problem, which speeds up the process of starting treatment. A prompt response to a problem helps to avoid irreparable processes in the body and eliminate the development of pathology.
DISEASE OF MANY NERVES: WHAT YOU NEED TO KNOW ABOUT IT
Anna Borisovna, what is polyneuropathy and how common is this disease? — From Greek, the name of this disease is translated as “disease of many nerves.” This very accurately defines the essence of the disease. After all, polyneuropathy is a pathological process that represents multiple lesions of the peripheral nervous system.
The disease occurs frequently. Thus, according to European registers, the overall prevalence of peripheral neuropathies in populations averages 2,400 per 100 thousand, and among elderly people reaches 8,000 per 100 thousand people. The primary incidence of neuropathies usually does not exceed 40 cases per 100 thousand per year.
In Russia, the diagnosis of “polyneuropathy” is made in at least 60% of patients with signs of damage to the peripheral nervous system.
How does this disease manifest itself? — Clinical manifestations of polyneuropathy are usually diverse and have varying degrees of severity.
Many patients complain of weakness of the upper and lower extremities, difficulty breathing, and some have difficulty chewing and speaking.
A frequent manifestation of polyneuropathy is disturbances in urination (especially often in the form of urinary incontinence), erection and digestion in the form of constipation.
Decreased sensitivity and discomfort in the limbs in the form of pins and needles, burning and swelling can also be symptoms of polyneuropathy.
Often patients are bothered by a number of vegetative symptoms. For example, orthostatic hypotension. It manifests itself as a sharp decrease in pressure when changing body position. Naturally, this immediately causes weakness and dizziness, even to the point of fainting.
Also with polyneuropathy, there is trembling of the fingers, involuntary muscle twitching, pallor and sweating, which does not depend on temperature and physical effort, shortness of breath, rapid heartbeat accompanied by arrhythmia, impaired coordination of movements and even slow healing of wounds.
Are there any painful sensations? — Pain due to polyneuropathy is a classic example of neuropathic pain syndrome. And this pain is not associated with a malfunction of any organ. It manifests itself against the background of damage to the nerve fibers of certain parts of the central or peripheral nervous system. Because of this, incorrect signals are sent to pain centers. A clear example of neuropathic pain is phantom syndrome. This condition is characterized by the fact that the amputated limb continues to hurt.
Neuropathic pain always causes persistent and very intense pain. And at the same time, it is practically not relieved by traditional analgesic medications. Such persistence of neuropathic pain naturally causes a lot of negative emotions in patients. Periodically recurring attacks become so painful that they provoke emotional imbalance and depression. There are often cases when polyneuropathy leads to partial loss of ability to work and even disability.
Are the causes of polyneuropathy known? — Based on their occurrence, there are seven main groups of neuropathies:
- Inflammatory and infectious polyneuropathies. They occur against the background of diphtheria, HIV or other diseases.
- Toxic polyneuropathy - most often are the consequences of chronic poisoning with alcoholic beverages, chemical compounds, incl. household, and even medications, if they are used for other purposes.
- Post-traumatic polyneuropathy. First, damage occurs due to cuts, bruises and fractures. Then scar processes occur in the area of wound healing, which compress the nerves.
- Hereditary polyneuropathies (Charcot-Marie-Tooth polyneuropathy, etc.) are systemic diseases that are characterized by damage to several organ structures.
- Autoimmune polyneuropathies are formed against the background of autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, etc.
- Diabetic polyneuropathy of the lower extremities occurs in people suffering from diabetes mellitus for a long period of time.
- Paraneoplastic polyneuropathy. This diagnosis is made against the background of an existing cancer of any location.
Which doctor and for what symptoms should you contact? — At the first manifestations of sensitivity disorders, pain and weakness in the limbs, you should contact a neurologist or neurologist-algologist. Let me remind you that an algologist is a specialist who studies and, above all, treats pain and pain syndromes. This area of medicine is still relatively young, but pain treatment centers are already operating in a number of clinics.
What diagnostic methods are used? — The examination plan is always drawn up individually depending on the specific clinical case. But in any case, the examination of a patient with polyneuropathy begins with a consultation with a neurologist, during which the doctor analyzes complaints and collects an anamnesis of the disease, assesses the neurological status.
The main method of instrumental diagnosis of peripheral nerve damage is electroneuromyography . Using this method, the fact of nerve damage is not only confirmed, but its nature is also determined.
In complex diagnostic cases, the doctor may recommend ultrasound of peripheral nerves, MRI of the plexuses, diagnostic lumbar puncture, morphological examination of the nerve (biopsy) , etc.
To clarify the reasons that caused widespread damage to peripheral nerves, a thorough examination is necessary, incl. comprehensive laboratory blood test (general and biochemical blood test, study of hormones, vitamins, etc.).
If hereditary polyneuropathy is suspected, molecular genetic analysis and consultation with a geneticist are necessary.
Also, to identify the underlying disease, which can cause damage to peripheral nerves, an instrumental general somatic examination , incl. cancer screening (CT lung, ultrasound of the mammary glands, mammography, ultrasound of the prostate and scrotum, esophagogastroduodenoscopy of the digestive system, colonoscopy, ultrasound of the abdominal and pelvic organs, etc.).
What treatment is given? — Only comprehensive treatment can help cope with polyneuropathy. It should include therapy for the underlying disease, auxiliary drug symptomatic therapy with drugs of various groups and non-drug treatment methods (physiotherapeutic treatment, physical therapy, reflexology, balneotherapy, psychotherapy, etc.). This approach in practice makes it possible to achieve highly effective treatment.
In modern neurology, based on many years of experience, treatment for the painful form of peripheral polyneuropathy has been developed. In particular, along with drug therapy, the possibilities of non-drug treatment methods are widely used. transcranial magnetic stimulation and cognitive behavioral therapy have proven to be the best , followed by exercise therapy .
What is transcranial magnetic stimulation? — Transcranial magnetic stimulation is used in the treatment of neuropathic pain syndrome. This procedure is based on the rhythmic effect of a magnetic field on the peripheral nervous system. It allows you to achieve positive health results completely painlessly. Magnetic influence is carried out using alternating current, it affects the cerebral cortex, after which it affects the central nervous system.
What treatment methods are used in pain centers? — The multidisciplinary team of specialists at pain treatment centers also have other methods of rehabilitation treatment in their arsenal: magnetic therapy, electrotherapy, massage in an electrostatic field, breathing exercises, oxygen inhalation, dry carbon dioxide bath, hyperbaric oxygen therapy (a method of saturating the patient with oxygen under high pressure in hyperbaric chambers). hyperbaric chambers), aromatherapy.
It is good when the treatment of a patient with chronic neuropathic pain syndrome is divided into three stages.
- The first stage begins with a consultation with a neurologist-algologist, who conducts a comprehensive diagnosis and identifies the cause of pain, makes a diagnosis and prescribes drug and non-drug therapy, and, if necessary, refers rehabilitation specialists (physiotherapist, physical therapy doctor, reflexologist) to consultations.
- In addition to the first stage of treatment, the neurologist-algologist determines indications and contraindications for the second stage of treatment using interventional methods. This is local drug injection therapy (therapeutic and diagnostic blockades), which are performed together with an anesthesiologist-resuscitator.
- The third stage could be spinal neurostimulation. It is carried out using a small device - an electrical pulse generator, which is implanted subcutaneously in the spinal cord.
Is it possible to use folk remedies for polyneuropathy? - Definitely, “No”! At the first symptoms, a consultation with a neurologist is necessary to prescribe a comprehensive examination to identify the causes of polyneuropathy and prescribe further therapy.
Will lifestyle changes help? - Yes, sure. After identifying the main cause of polyneuropathy, the attending physician will give recommendations for lifestyle correction depending on the underlying disease.
What can be recommended as prevention? — Prevention is possible for some diseases that may be complicated by polyneuropathy. For example, diabetes. Adequate blood glucose control will reduce the risk of diabetic polyneuropathy or slow its progression.
What consequences and complications do polyneuropathy lead to? — It depends on the type of polyneuropathy and the disease that causes it. Sometimes the consequence of polyneuropathy is complete paralysis of the limbs or respiratory organs. In addition, progressive polyneuropathy causes excruciating pain and severe sensory disturbances. People lose the ability to walk and care for themselves; the resulting helplessness, in turn, leads to anxiety and depression. The functioning of internal organs may also be disrupted.
But all this can be avoided if treatment is started in a timely manner.
Can polyneuropathy become a trigger for other diseases? — Most often, damage to peripheral nerves is itself a consequence of the serious diseases described above. But polyneuropathy can also become a provocateur. For example, psychosomatic manifestations. In addition, pain syndrome, which often occurs against the background of damage to peripheral nerves, can negatively affect the condition of the cardiovascular system.
What mistakes do patients who have signs of polyneuropathy make? — The biggest mistake is that many do not pay attention to the first manifestations of the disease (numbness, tingling, etc.), but come to a specialist already in the advanced stage of the disease, when excruciating pain begins to bother them. But it’s no secret that it’s easier to cope with any illness at the very beginning of its development.
How important is treatment adherence? - Extremely important! Often, an adequate analgesic effect can only be achieved with a combination of drugs for the treatment of chronic neuropathic pain. This requires the neurologist-algologist to be highly qualified to select the dose and monitor this treatment regimen, and for the patient to strictly adhere to the doctor’s prescriptions.
Can COVID-19 cause polyneuropathy? — As with any other severe viral infection, COVID-19 can affect the peripheral nervous system. Although, of course, at the moment there is not enough information about the coronavirus and no hasty conclusions can be drawn. It is possible that the appearance of polyneuropathy during the treatment of COVID-19 is also caused by the toxic effects of drugs used in therapy.
Well, those who already have a history of “polyneuropathy” need to be especially careful in protecting themselves from possible infection.
Prevention
The main task of prevention is the timely treatment of infectious and systemic diseases. Patients with diabetes mellitus and other predisposing pathologies must regularly visit a doctor and strictly follow his prescriptions and recommendations. Other preventive measures come down to simple rules:
- give up bad habits;
- lead an active lifestyle with moderate physical activity;
- follow a proper and balanced diet;
- wear comfortable clothes and shoes that do not put pressure on your feet and ankles;
- Spend more time outdoors and take walks.
![Rice. 2. The role of vitamin B12 in the synthesis of the myelin sheath of nerve fibers [45] 2. The role of vitamin B12 in the synthesis of myelin sheath [45]](https://lovetherapy.ru/wp-content/uploads/ris-2-rol-vitamina-v12-v-sinteze-mielinovoj-obolochki-nervnyh-330x140.jpg)