It is generally accepted that joint diseases most often occur after injuries. In athletes, arthrosis is caused by frequent overloads; in overweight people, it is caused by heavy weight. Treatment of osteoarthritis may be necessary for diabetes and osteoporosis, against the background of hormonal changes or unfavorable heredity. All this is true, if not for one “but”.
Recent discoveries by scientists indicate that one of the main causes of degenerative changes in joints is psychogenic in nature. We are talking about chronic stress in which the patient lives. Why does this happen and can it be avoided?
Do you live in constant stress? Expect joint problems
The mechanism of arthrosis development due to stress
With prolonged experiences in the human body, the level of corticosteroid hormones increases. Biochemists are convinced that their excess stops the production of hyaluronic acid, an important component of synovial fluid, or joint lubrication. Gradually, dehydration and drying out of the cartilage occurs, which becomes thinner and cracks - arthrosis is evident!
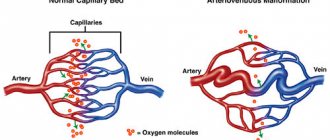
A large amount of stress hormones worsens the permeability of capillaries, and with it the blood flow in damaged vessels. If, against such a hormonal background, trauma or microtrauma to the joint occurs, this accelerates the deformation of the cartilage.
Start thinking positively, get rid of chronic stress - it will be easier to cope with arthrosis!
How does stress cause back pain?
There are many theories about the causes of stress-related back pain. It is important to note that the overriding principle of all of these theories is that psychological and emotional factors cause certain physical changes that result in back pain.
In most theories of stress back pain, the cyclic pain gets worse as it continues, leading the patient to become restless and have trouble performing daily activities.
Cyclic pain is characterized by:
- The patient becomes unnecessarily limited in performing many functions of daily living
- This decrease in activity is due to the patient's fear of pain or injury.
- This fear may be exacerbated by the doctor's (close) recommendations to take it easy due to the presence of diagnosed small structural changes (which in fact may have nothing to do with back pain)
- Restrictions in movement and activity lead to impaired physical condition and weakening of muscles, which in turn leads to increased back pain
Of course, this cycle leads to increased pain, increased fear, and even greater physical maladjustment, along with other reactions such as social withdrawal, depression and anxiety.
Which negative emotions are especially harmful to joints?
Medicine does not give an exact answer to this question. The information presented below is the result of individual studies and can be excellent food for thought for those who are concerned about their health.
- Coxarthrosis
Scientists have noticed that treatment for arthrosis of the hip joint is usually required by people who are pleasant in communication, not prone to conflicts, restrained and calm. Irritation, anxiety, and suppressed anger provoke the release of corticosteroids into the blood, which interfere with the production of synovial fluid. Internal tension in the nervous system causes spasms and hypertonicity of the skeletal muscles, especially strong in the hip area, which strongly “pinches” the damaged joint. This accelerates its deformation.
In Western countries, where it is customary to smile to hide your weaknesses, the percentage of people with coxarthrosis is constantly growing. After all, suppressing emotions often leads to a severe depressive-stressful state.
Coxarthrosis often affects reserved, non-conflict people who tend to suppress their emotions
- Gonarthrosis
Knee arthrosis occurs, according to researchers, as a result of severe stress or difficult experiences. This happens, for example, after a divorce, dismissal from work, loss of loved ones or other difficult stages in life.
Gonarthrosis is diagnosed in people who are emotionally tired, who instead of interest in life have fatigue accumulated over the years. This category includes, for example, women “50+” who are forced to work, manage the household and deny themselves everything. Even when they do not yet need treatment for osteoarthritis, since their knees are still healthy, they still walk with difficulty, as if “with weights on their legs.”
How to become energetic and cheerful again? How to regain your vital energy? We present 10 ways to get rid of lethargy, laziness and apathy, and therefore give a worthy rebuff to arthrosis:
A person without vital energy stoops, his legs swell, blood circulation in them is disrupted - vascular thrombosis or varicose veins occurs. The knee joints gradually lose flexibility, and the cartilage in them loses moisture (due to the lack of normal blood supply). The cartilage tissue dries out and cracks - arthrosis begins.
Gonarthrosis in men develops against the background of hyper-responsibility. However, since representatives of the stronger sex more often allow themselves “little joys,” they face the problem of treating severe arthrosis less often than women. In turn, it has been noted that the final stages of this disease are observed mainly in intelligent but critical people prone to chronic dissatisfaction.
Osteoarthritis of the knee often develops against the background of emotional fatigue or hyperresponsibility
Types of neuropathy
The types of neuropathy are determined depending on the number of nerves affected. If only one nerve is involved in the pathological process, they speak of mononeuropathy. This type of disease, compression-ischemic neuropathy, most often occurs in large nerve trunks - the femoral, sciatic, trigeminal or radiocarpal nerve. The pathology is relatively easy to diagnose; symptoms appear in the direction of the location of the nerve trunk in the tissues.
Another type is ischemic neuropathy, but it only affects the optic nerve. In fact, this is his heart attack, leading to a decrease in visual acuity, even to blindness. Separately, there is post-traumatic neuropathy, which occurs as a result of a fracture, compression of a limb, sprain or other injuries.
With polyneuropathy, entire groups of peripheral nerves are affected. The disease can occur simultaneously in several limbs, often symmetrically on different halves of the body, and is accompanied by a large number of symptoms. Depending on the causes, the following types of polyneuropathy are distinguished:
- metabolic – occur due to metabolic disorders, there are diabetic, uremic, hepatic;
- infectious-toxic – develop due to viral diseases (AIDS, leprosy, Lyme disease);
- toxic - nerve fibers are damaged by poisons, heavy metals, alcohol, possible with an overdose of medications;
- hereditary - it includes inherited genetic diseases and syndromes: Refsum's disease, Roussy-Levi syndrome, Charcot-Marie-Tutte amyotrophy;
- nutritional – occur in people with malnutrition and a deficiency of certain vitamins;
- autoimmune - are formed when the immune system attacks its own nerve fibers, these include Miller-Flesher syndrome, paraneoplastic neuropathies in cancer, paraproteinemic polyneuropathies.
Neuropathies are divided into several types, depending on the nature of the damage to the nerve trunk. They can be axonal, when the inner part of the nerve is damaged, and demyelinating, in which the sheath is destroyed and the transmission of the nerve impulse is disrupted.
The following emotions are especially dangerous:
- internal irritation;
- chronic resentment towards others, loved ones or the whole world;
- discontent.
When a person feels these emotions, he experiences a spasm of the anterior thigh, which accompanies gonarthrosis in 100% of cases. At first, the spasm does not make itself felt, but then it “tightens” the knees and prevents their free movement. As a result, either a rupture of the meniscus or deformation of the cartilage occurs.
Knees often bother people who are prone to criticism, self-criticism and dissatisfaction.
Symptoms of polyneuropathy
The reason for contacting a neurologist is causeless pain or a feeling of discomfort. Symptoms of neuropathy depend on the type of disease, whether the inner part of the nerve or just its sheath is involved in the pathological process.
The following symptoms should alert you:
- sudden tingling or burning sensation;
- muscle weakness;
- disturbance of temperature sensations;
- inability to perform certain movements of the limbs;
- gait disturbances;
- visible muscle atrophy, body asymmetry.
Sometimes pathological hypersensitivity appears when a slight touch of a certain part of the body causes severe pain, but with significant impact there is no sensation. Pain sensitivity may completely disappear, so, for example, a minor injury or cut will not be noticed. But due to a violation of innervation, such a wound takes a long time to heal and often turns into a trophic ulcer.
In advanced cases, autonomic disorders appear, blood pressure may increase or decrease, the functioning of the digestive tract changes, the blood supply to the skin deteriorates, it looks pale, dry and atrophic.
Often a person gets used to these sensations and because of this postpones a visit to the doctor. This increases the risk of progression of the disease that causes pathology of the nervous system. Meanwhile, the body's protective resources are depleted. With neuropathy, a painless myocardial infarction can occur, since due to damage to the sensory nerves the person will not feel pain.
Early diagnosis of these conditions can be done using the Medmarvel diagnostic complex, which is installed in medical offices 36.6. Within 10 minutes you will be able to find out if you have early, initial, not yet pathological, manifestations of neuropathy.
How important is psychological attitude in the treatment of arthrosis?
Practice shows that those who can restructure their thinking in a positive way succeed in treating arthrosis. Negative emotions increase the production of stress hormones, while positive ones, on the contrary, help activate the body's defenses.
The effect of any treatment largely depends on the patient’s mood. It is not surprising that even the highly effective intra-articular injections Noltrex have different effects on people with an identical diagnosis. For one person, two injections are enough to completely restore mobility and get rid of pain, while another needs 4-5 injections.
The disease recedes before the patient’s optimistic mood
Today, the theory about the connection between arthrosis and stress has not yet been scientifically substantiated, but scientists have every reason to believe that this factor is of great importance not only in the development of the disease, but also in its treatment. Learn to think positively, look for positive moments in life, say “no” to dissatisfaction, criticism and other negative emotions - you will be surprised by the results!
Treatment methods for leg pain
If alarming symptoms appear, you should contact a therapist or specialized specialist (neurologist, endocrinologist, infectious disease specialist, traumatologist, etc.). Further treatment strategy is based on eliminating the cause of the disease and symptomatic therapy.
Our clinic uses methods of hardware treatment for leg pain, manual therapy, massage, and physiotherapy. The doctor suggests a suitable method of therapy after reviewing the diagnostic results and assessing the patient’s complaints.
Treatment of leg pain using kinesitherapy involves the use of special equipment - European suspension systems. This method is based on the healing power of movement and helps relieve pain, swelling, and improves blood circulation in the extremities.
Manual therapy is effective for pain in the legs of vertebrogenic etiology, that is, caused by a hernia or protrusion of the lumbar disc. In such cases, treatment is carried out using American systems, which are highly effective.
Massage is an effective method of treating leg pain, which helps relieve muscle spasms, increase elasticity and muscle tone, relieve pain and normalize tissue trophism. Therapy is carried out in a course.
Various types of physiotherapy are used to treat leg pain:
- shock wave. It has both a therapeutic and analgesic effect in the treatment of pain in the legs associated with diseases of the joints, ligaments, tendons, after operations and injuries, as well as in diseases of the feet, especially heel spurs (complete cure);
- ultrasonic;
- magnetic therapy;
- phonophoresis;
- electrophoresis;
- quantum therapy;
- electrotherapy;
- cryotherapy.
You can learn more about treatment options for leg pain and what options are right for you at your appointment. Don’t put off solving the problem until later, make an appointment with a specialist as early as possible.
Diagnosis and treatment of restless legs syndrome
It is customary to prescribe medications for RLS in cases where it significantly disrupts the patient’s vital functions, causing persistent sleep disturbance, and non-drug measures are not effective enough. In mild cases, you can limit yourself to taking sedatives of herbal origin or prescribing a placebo, which can give a good, but sometimes only temporary effect.
In more severe cases, it is necessary to choose a drug from four main groups: benzodiazepines, dopaminergic drugs, anticonvulsants, opioids [17].
Benzodiazepines accelerate the onset of sleep and reduce the frequency of awakenings associated with PDC, but have relatively little effect on the specific sensory and motor manifestations of RLS, as well as PDC. The most commonly used benzodiazepines are clonazepam (0.5–2 mg at night) or alprazolam (0.25–0.5 mg). With long-term use of benzodiazepines, there is a danger of developing tolerance with a gradual decrease in effect and the formation of drug dependence. The negative aspects of the action of benzodiazepines also include the possibility of developing or increasing drowsiness during the day, decreased libido, increased sleep apnea, episodes of confusion at night, as well as worsening cognitive impairment in the elderly. In this regard, benzodiazepines are currently used sporadically in mild or moderate cases - during periods of deterioration, and in severe cases requiring constant treatment, they are prescribed only when dopaminergic drugs are ineffective [16, 17].
Dopaminergic drugs (levodopa and dopamine receptor agonists) are the mainstays of treatment for RLS. They affect all the main manifestations of RLS, including the maximum concentration limit. Dopaminergic drugs are so effective in RLS that a positive reaction to them can serve as an additional criterion for diagnosing RLS, and its absence, as, for example, in Parkinson's disease, should be considered a basis for revising the diagnosis. The effect of dopaminergic drugs in RLS occurs in doses that are significantly lower than those used in Parkinson's disease. Apparently, dopaminergic drugs are equally effective in both primary and symptomatic variants of RLS [6].
Levodopa has been used for RLS since 1985, when its effectiveness in this category of patients was first shown. Currently, levodopa is prescribed in combination with DOPA decarboxylase inhibitors benserazide (Madopar) or carbidopa (Nakom, Sinemet). Treatment begins with 50 mg of levodopa (approximately 1/4 tablet of Madopar “250”), which the patient should take 1–2 hours before bedtime. If the effectiveness is insufficient, after a week the dose is increased to 100 mg, the maximum dose is 200 mg. Taking levodopa provides an adequate effect in 85% of patients. In many patients, it remains effective for many years, and in some patients its effective dose may remain stable and even decrease [10]. Levodopa medications are usually well tolerated by patients with RLS, and side effects (nausea, muscle cramps, tension headaches, irritability, dizziness, dry mouth) are usually mild and do not require discontinuation of the drug. Given the rapid onset of effect and the lack of need for dose titration, levodopa may be considered the treatment of choice for intermittent worsening symptoms.
However, with long-term use in a significant proportion of patients, the effectiveness of levodopa decreases, while the duration of action of a single dose is reduced to 2-3 hours, which may be followed by a rebound increase in the symptoms of RLS and PDC in the second half of the night. In this case, it is recommended to increase the dose of the drug or add a second dose immediately before bedtime or upon awakening at night. However, with an increase in the dose of levodopa, the rebound increase in symptoms may not be eliminated, but only shift to the early morning hours, and its intensity may increase. Experience shows that a more reasonable alternative in this situation is to switch to a sustained-release levodopa preparation (Madopar GSS). A slow-release drug that acts over 4 to 6 hours to ensure good sleep throughout the night and prevent morning rebound symptoms.
In approximately half of patients, during long-term treatment with levodopa, symptoms gradually begin to appear earlier (sometimes even during the day), becoming more intense and widespread (the so-called “augmentation”). The higher the dose of levodopa, the stronger the augmentation [14], so increasing the dose of levodopa in this situation only worsens the situation, completing a vicious circle. When using Madopar GSS as a basic therapy for RLS, rebound enhancement and augmentation are observed less frequently than when taking standard levodopa drugs. In this regard, Madopar GSS is now often used as a means of initial treatment of RLS (1-2 capsules 1-2 hours before bedtime). Sometimes it is reasonable to recommend to the patient 1 hour before bedtime 100 mg of levodopa as part of a standard drug or a soluble fast-acting drug, which provides a relatively rapid onset of effect, and 100 mg of levodopa as part of a slow-release drug (for example, 1 capsule of Madopar GSS). When augmentation develops, it is recommended to either replace levodopa with a dopamine receptor agonist, or add it to it (by reducing the dose of levodopa).
Dopamine receptor agonists (DRAs) have been used for RLS shortly after levodopa was shown to be effective, in 1988. Experience shows that the effectiveness of ADR for RLS is approximately equivalent to that of levodopa. ADRs can be considered as a means of choice if long-term daily medication is required. For RLS, both ergoline drugs (bromocriptine, cabergoline) and non-ergoline drugs (pramipexole, piribedil) are used [12, 14]. Non-ergoline drugs have the advantage of being free from side effects such as vasospastic reactions, pleuropulmonary, retroperitoneal fibrosis, and fibrosis of the heart valves. To avoid nausea, ADRs are taken immediately after meals and the dose is adjusted by slow titration. Pramipexole is initially prescribed at a dose of 0.125 mg, then gradually increased until the effect is achieved (usually no more than 1 mg). The effective dose of piribedil is 50–150 mg. For bromocriptine treatment, the starting dose is 1.25 mg and the effective dose ranges from 2.5 to 7.5 mg. Cabergoline treatment begins with 0.5 mg, and its effective dose is 1–2 mg. The indicated dose is usually prescribed once 1-2 hours before bedtime, but in severe cases, additional administration of the drug may be necessary in the early evening hours. Side effects when taking ADR include nausea, fatigue, headache, dizziness, and daytime sleepiness. Domperidone may be prescribed at the beginning of treatment to prevent nausea.
With long-term use of ADR, signs of augmentation are detected in approximately 25–30% of patients, but they are almost never as severe as with levodopa treatment. If one of the ADRs turns out to be ineffective, you can try replacing it with another drug from this group. It is important to note that dopaminergic drugs, while eliminating the symptoms of RLS, do not always lead to normalization of sleep, which requires the addition of a sedative drug (benzodiazepine or trazodone).
It should be noted that, probably due to the absence of denervation and the normal number of dopaminergic neurons, dopaminergic drugs are effective in RLS at doses significantly lower than those used in Parkinson's disease. Moreover, side effects such as dyskinesia, psychosis, impulsivity, and compulsive behavior (common in Parkinson's disease) are extremely rare in RLS.
In those few cases where the patient does not tolerate dopaminergic drugs well, and benzodiazepines are ineffective or cause intolerable side effects, they resort to anticonvulsants or opioids. Of the anticonvulsants, gabapentin is currently most often used, at a dose of 300 to 2700 mg/day [9]. The entire daily dose is usually prescribed once in the evening. Opioid drugs (codeine, 15–60 mg; dihydrocodeine, 60–120 mg, tramadol, 50–400 mg at night, etc.) can significantly reduce the symptoms of RLS and PDC, but the risk of developing drug dependence makes their use justified only in the most severe cases where all other treatment methods are ineffective. The treatment algorithm for RLS is shown in the figure.
For RLS, it is possible to use some other drugs (clonidine, folic acid, magnesium, vitamins E, B, C), but their effectiveness has not been confirmed in controlled studies [18]. In some patients, amantadine, baclofen, zolpidem are effective; beta blockers (for example, propranolol) can reduce symptoms, but sometimes cause them to worsen.
Treatment of RLS has to be carried out over a long period of time over many years, and therefore it is very important to follow a unified treatment strategy. Sometimes it is carried out only during the period of intensification of symptoms, but often patients are forced to take certain drugs for life to maintain drug remission. It is better to start treatment with monotherapy, choosing a drug taking into account its effectiveness in each individual patient and the presence of concomitant diseases. If monotherapy is insufficiently effective or in cases where, due to side effects, it is not possible to achieve a therapeutic dose of one of the drugs, it is possible to use a combination of drugs with different mechanisms of action in relatively small doses. In some cases, it is advisable to rotate several drugs that are effective for a given patient, which allows them to maintain their effectiveness for many years.
Treatment of RLS in pregnant women is particularly challenging. None of the drugs commonly used for RLS are considered safe during pregnancy. Therefore, when RLS develops during pregnancy, they are usually limited to non-drug measures (for example, a walk and a warm shower before bed) and the administration of folic acid (3 mg/day), as well as iron supplements (if there is a deficiency). Only in severe cases is it permissible to use small doses of clonazepam, and if they are ineffective, small doses of levodopa.
Trazodone and monoamine oxidase inhibitors (MAOIs) can be used to treat depression in patients with RLS. Data on the effect of selective serotonin reuptake inhibitors in patients with RLS and PDC are contradictory. However, in some patients they can nevertheless improve the condition, which is explained by the suppression of the activity of dopaminergic neurons. Tricyclic antidepressants, like antipsychotics, are contraindicated.
Arterial diseases
Pain in the legs is caused by:
- atherosclerosis of the arteries of the lower extremities;
- obliterating endarteritis;
- thromboangitis obliterans;
- embolism and arterial thrombosis.
Atherosclerosis of the arteries of the lower extremities
Among diseases of the arteries of the lower extremities, atherosclerosis is the most common - in almost 90% of cases. It refers to obliterating vascular diseases (obliterating - leading to closure, fusion). Previously, the disease mainly affected older men. Unfortunately, there is now a tendency towards rejuvenation of this disease, and atherosclerosis occurs even in middle age. Cases of obliterating atherosclerosis in women have also become more frequent.
Risk factors are well known - smoking, low physical activity, lifestyle changes, hereditary factors, hypertension, coronary heart disease, diabetes mellitus, liver and biliary tract diseases, obesity, high cholesterol in the blood.
During the disease process, plaques consisting of cholesterol, other fats, calcium and connective tissue form on the inner walls of the arteries. The lumen of the arteries narrows. At rest, arterial circulation in the lower extremities may be sufficient, but during physical activity the increased oxygen demand of the muscles cannot be satisfied. The muscles respond to this with pain, which is how intermittent claudication appears. When walking, especially uphill, pain occurs in the calf muscles, forcing the patient to periodically stop for it to pass. If pain occurs in the entire leg, it means that the arteries at the pelvic level are affected by the pathological process. Unlike radiculitis, pain does not depend on sudden movements or turns of the body.
Instead of pain, you may experience cramps, weakness, or a feeling of heaviness in your legs.
The legs become cold and pale, and no pulse can be felt on them. At the last stage, trophic ulcers and foci of gangrene may form. If gangrene develops, amputation of the affected limb may be necessary to save the patient's life. Often, especially with high occlusions, when necrosis develops on the fingers, amputation is performed at the level of the upper third of the thigh, since with lower amputations it is difficult to achieve healing of the postoperative wound.
Find out more about the promotion >>>
Obliterating endarteritis
The International Classification of Diseases ICD-10 does not provide for such a diagnosis. It is necessary to use other diagnoses specified in this document - “arterial atherosclerosis”, “thromboangiitis obliterans”, “other specified peripheral vascular diseases”, “other unspecified peripheral vascular diseases”.
The disease affects mainly middle-aged and even young men. The exact cause of the disease is still not known. The role of cold and mechanical trauma, as well as autoimmune processes, is suggested.
The small arteries of the legs are affected. Unlike atherosclerosis, which develops gradually, obliterating endarteritis is characterized by an undulating course - exacerbations alternate with remissions. The symptoms and complications and outcomes are almost the same - intermittent claudication, possible amputation due to gangrene, etc.
Thrombangitis obliterans (Berger's disease)
This is a “disease of young men who smoke.” An autoimmune mechanism of development is suggested. Exacerbations alternate with remissions. Every second patient undergoes amputation at the level of the fingers, foot or thigh.
A feature of thromboangiitis obliterans and endarteritis is the symmetry of the damage to the extremities and the possible involvement in the process of not only the lower, but also the upper extremities. At the same time, atherosclerotic lesions are often unilateral and affect almost exclusively the legs.
Embolism and arterial thrombosis
In embolism, an artery is blocked by some substance (in thrombosis, a blood clot).
In the area fed by the blocked artery, diffuse pain occurs. The limb first turns pale, then turns blue. Her pulse can no longer be felt. Numbness appears, and in severe cases paralysis may develop. In such cases, if treatment is not started in a timely manner, everything ends with rapidly developing ischemia, wet gangrene and amputation of the limb.
Vein diseases
Leg pain is accompanied by:
- Varicose veins;
- phlebitis and thrombophlebitis;
- postthrombophlebitic syndrome.
Varicose veins
This disease is widespread and is a very pressing problem in medicine and cosmetology.
Find out more about the promotion >>>
Phlebitis and thrombophlebitis
Phlebitis is inflammation of a vein. Thrombophlebitis is a complication of phlebitis or varicose veins of the lower extremities. With thrombophlebitis, a blood clot forms in the inflamed vein. Pain is a concern and swelling of the legs is possible.
Deep vein thrombosis is fraught with complications, the most dangerous of which are venous gangrene of the limb (with high blockage and blockage of all outflow pathways of venous blood) and pulmonary embolism. The risk of thromboembolism is highest in the presence of an unfixed - floating thrombus. The larger the detached fragment of the blood clot, the greater the likelihood of an unfavorable outcome, including death.
A common complication of deep vein thrombophlebitis is postthrombophlebitis syndrome.