Minimum brain dysfunction in children, or abbreviated “MMD,” is a syndrome that includes a complete problematic complex in the psychological and emotional sphere, arising from insufficient productivity of the central nervous system. Symptoms of MMD vary by age, most often occurring in infancy and adulthood.
For example, in very young children, minimal brain dysfunction results in few neurological symptoms. Older children suffer from mental retardation, hyperactivity and an inability to adapt to society, adapt to it and become one with it. The disease is diagnosed using psychological tests and various techniques. Treatment is carried out using pedagogical, psychotherapeutic, pharmacological means.
General information
MMD, like other similar diseases (encephalopathy, hyperkinetic chronic brain syndrome) is a pathological condition, the springboard for which is considered to be the central nervous system if disturbances, failures, deviations in behavior and actions regularly occur in its work, as well as problems with emotionality and in the vegetative sphere .
This syndrome was discovered and subsequently described by Dr. Clemens in 1966. Minimal brain dysfunction is rightly considered one of the most common diseases among children; as a rule, it is diagnosed in almost 5 percent of children in primary school; in preschool classes, the incidence rate is close to 22 percent.
Often, experts give a positive prognosis for treatment, but we must not forget about the etiology of the disease. Most children (almost 50 percent) lose clinical symptoms during development, personality formation, and growing up. Delays in psychological development can also be eliminated thanks to timely and high-quality treatment.
MANIFESTATIONS OF PATHOLOGY
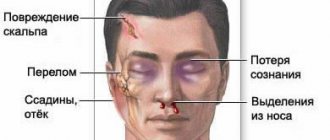
The first signs of a pathology such as minimal brain dysfunction in children can be noticed at a very early age. A modified shape of the skull and ears, deviations from the norm in the structure of the palate and tooth growth - all of these are visual manifestations of MMD in children.
The clinical picture of the pathology is quite extensive. It can have a variety of manifestations:
- autonomic disorders. These include excessive sweating, marbling of the skin, malfunction of the gastrointestinal tract (stool instability, frequent fluctuations in constipation and diarrhea), unstable pulse and functioning of the cardiovascular system;
- weak muscle tone and movement disorders. Muscle tone may be uneven, there is asymmetry of tendon reflexes, and lack of fine motor skills. It is especially difficult for such children to fasten buttons or tie shoelaces, and they have difficulty working with scissors, drawing with a pencil, or writing with a pen. Due to the fact that the facial muscles are also weakened, the child’s facial expressions are quite poor, he almost never makes faces or grimaces. Children with MMD have difficulty catching a ball, riding a bicycle, or walking in a straight line;
- The disorder also affects the behavior of children. Usually such kids are very active, they are restless, easily distracted, and find it difficult to concentrate on completing the assigned task;
- unstable emotional background. Children experience frequent mood swings.
Minimal brain dysfunction is accompanied by a high degree of depletion of nerve cells located in the upper layers of the cerebral cortex. The consequence of this is rapid fatigue, and certain difficulties arise with memory and the formation of a stock of general concepts. All this leads to mental and speech delays in development.
Children with MMD also experience difficulties in the social sphere. They find it easier to find a common language with children who are younger than them in age, while excessive excitability and a tendency to create conflict situations do not allow them to establish contacts with peers within the walls of preschool educational institutions. Such children may have problems falling asleep, they often toss and turn in their sleep, and most of them suffer from urinary incontinence.
Gradually, as the baby gets older, the clinical manifestations of the disorder disappear without a trace. According to statistics, in early preschool age, MMD is observed in approximately every fifth of children, and already in the elementary grades, the pathology can be found in one in 20 students. But this is only possible if special attention is paid to the upbringing and education of a child with MMD. Only in very rare cases do some of the symptoms of the disorder persist into adulthood.
Causes
Modern experts refer to MMD syndrome as damage to limited areas of the cerebral cortex or anomalies in the development of the central nervous system, occurring due to various factors. If such a syndrome develops in a child quite early, that is, between the ages of 3 and 6 years, then experts attribute this to problems with demonstrated pedagogy and neglect in the emotional and social sphere. Taking into account the early age of the child and the etiology of the disease, it is customary to distinguish 3 groups of factors that affect the brain and are catalysts for MMD syndrome: antenatal, intranatal, postnatal.
The first group is characterized by acute viral diseases or exacerbation of chronic pathology in the mother of the child, which is characterized by long-term intoxication, poor nutrition, and disturbances in the metabolism of proteins, fats, and carbohydrates. With pathologies of pregnancy, they manifest themselves in the form of preeclampsia, eclampsia, and threats to involuntary termination of pregnancy. The list of numerous factors also includes a polluted environment, possible background radiation (depending on the area), improper use of pharmaceuticals, frequent drinking of alcohol, smoking tobacco, drug use, and other infectious diseases.
Minimal brain dysfunction can develop in a child directly during birth procedures. This is influenced by many factors, but the most important are the rapidity of labor, weak contractile function of the uterus, caesarean section, errors in the work of obstetricians, and not fully open birth canals. But even if the birth was successful and no pathologies appeared, it is still worth understanding that MMD can strike at any moment. As the child grows up, the factors influencing the syndrome also change. For example, at the ages of 3 to 6 years, the quality of pedagogical and social work plays a key role in the formation of the syndrome. If they are neglected, this can lead to unpleasant consequences...
Causes of minimal brain dysfunction
This pathology is most often the result of birth trauma. It can be obtained either during pregnancy or during childbirth itself. The child’s spine as a whole, and in particular its cervical spine, experiences enormous loads when moving along the birth canal. When the baby squeezes between the pelvic bones, he turns almost 360 degrees. This often causes displacement of the cervical vertebrae, and in the future, problems with blood supply.
Often the cause is the incorrect actions of the midwife, which lead to compression and deformation of the skull, and sometimes to its damage. Large fetus, cesarean section, rapid labor, etc. are also considered possible causes.
Also, the disorder may begin to develop during pregnancy. This may be due to reasons such as:
- unbalanced and unhealthy diet of the expectant mother;
- severe toxicosis;
- drinking alcohol and smoking;
- insufficient sleep and stress;
- premature birth or post-term pregnancy;
- risk of miscarriage;
- long labor;
- fetal hypoxia;
- infectious diseases;
- injuries to the child’s cervical spine during childbirth;
- use of potent pharmacology, etc.
There are cases when MMD occurs after the birth of a baby. The reasons for this may be unfavorable living conditions and failure to meet the basic needs of the child, complications after illness, or brain damage.
The pathology manifests itself at the level of the central nervous system, as a result of which speech, attention and behavior are impaired. It is worth noting that although some developmental processes in a child with MMD are slower than in healthy children, his intelligence, as a rule, is within normal limits.
Symptoms of MMD in a child
The initial clinical symptoms of the disease “minimal cerebral dysfunction” can begin to appear in a child, both after childbirth and already at preschool or school age. Each age group has different symptoms and manifestations.
At 1 year of life of a child with MMD syndrome, neurological symptoms are especially pronounced. A lack of tone appears, muscle underdevelopment is especially noticeable, tremors, myoclonic contractions, and hyperkinesia appear. The symptom can occur unexpectedly and even unreasonably; it is almost impossible to predict the onset of an attack.
For this age, poor sleep, lack of appetite, vision problems and gaps in mental development are an integral part of the disease. From 8 to 12 months, the child begins to have problems with motor skills and nerves; Against this background, the gastrointestinal tract feels unwell, so alternating diarrhea and constipation is commonplace for MMD in early childhood. Regular nausea and vomiting can also be called characteristic and characteristic.
From 1 year to 3 years, symptoms change slightly, taking on a different form. Excitability increases, excessive motor activity appears, sleep is disturbed, appetite may decrease slightly or disappear completely; as a rule, it is very difficult for the child to fall asleep, but he wakes up extremely quickly. At this age, the lack of mass in the body and the slow development of speech are especially clearly visible.
At 3 years old, the child becomes clumsy, quickly gets tired, he is uncontrollable, impulsive, problems with perception appear when he unreasonably disobeys his parents, thus negativism is formed. The child is constantly moving, although chaotically and seemingly senselessly, all this is strongly mixed with clumsiness.
Children aged 3 years suffering from MMD syndrome are extremely restless, they often find it difficult to concentrate on one task or interest, and can easily be distracted by any noise, sound or other game that appears on the horizon. Seizures from too bright light, loud noises, ringing, and heat often occur. Children often suffer from traveling on buses, because they get motion sickness, feel dizzy, and experience nausea typical of motion sickness.
At the maximum level, minimal brain dysfunction manifests itself at a later age, when the child enters a group, kindergarten (age 4 to 6 years). In such children, one can notice excessive excitability, motor skills, both slow in development and overly active; confusion and absent-mindedness; poor memory, problems with perceiving information and understanding it; difficulties in mastering the educational program in kindergarten and school. Children with MMD find it difficult to learn to write, read, count even simple numbers, and solve examples.
While attending school, it becomes more difficult for a child to get along with his symptoms, as he begins to become aware of them, and also notices oddities in himself that are not typical for other children. He begins to close himself off from society, preferring to spend his free time alone, becomes selfish, and self-esteem and self-confidence decrease. But even in these cases, deviations from the rules occur. For example, against the background of an illness, a child may feel like a leader, but this will only be a symptom related to selfishness and detachment from social norms.
Minimal brain dysfunction as a factor in the maladjustment crisis in children
About the basic stages of development and the problem of the advisability of revising norms Child psychologists and psychotherapists are faced with the problems of minimal brain dysfunction (MBD) in children and adolescents in its most varied manifestations. For successful psychotherapy of these problems, it is not enough to rely on the request that parents of children with MDM come to the specialist with, since the request may turn out to be only the tip of the iceberg or may not relate to the problem voiced by the parents.
A very important point for putting forward a hypothesis and choosing psychotherapeutic tools for manifestations of MDM is the study of all issues relating to the course of the mother’s pregnancy, the characteristics of the birth itself, postpartum complications or infections suffered by the child, as well as the development of the child under 1 year of age relative to generally accepted developmental norms.
Studying the perinatal history of a child with MDM is also important in order to determine whether the child’s problems can be resolved without drug therapy or whether psychotherapy should be carried out simultaneously with observation and treatment by a child neurologist or psychiatrist.
Parents of children with MDM are often very sensitive to the concept of age norms, seeing their children clearly lagging behind developmental norms. Some parents of such children often categorically state that age standards are outdated, and each child has the right to an individual development standard, often citing doctors or foreign specialists and authors.
The issue of revising existing age standards has become acute in recent decades due to the growth of various types of deviant development in children from 0 to 7 years old. Among the reasons for this phenomenon, many authors name sharp civilizational leaps in the broadest sense, the consequences of destructive wars, environmental problems, and a decrease in the factor of natural selection of the population.
There are supporters of expanding the range of norms in the direction of reducing regulatory requirements among doctors, psychologists and neuropsychologists.
Reducing the regulatory requirements for age standards in children under 7 years of age, in our opinion, is unfounded, since age-related development standards should serve as a guideline that helps to timely identify and diagnose developmental abnormalities in order to take immediate measures to restore impaired functions of brain structures.
On the other hand, even if the percentage of mentally and somatically healthy children has decreased in recent years, this is unlikely to be a stable trend, taking into account the compensatory and adaptive capabilities of the developing brain to exogenous realities and the modern capabilities of organizing early diagnosis of the causes of deviant development, maladaptive crises of children with subsequent medication , physiotherapeutic, psychological correction.
Since in the ontogenesis of a full-fledged brain substrate, its structures and functional connections mature in stages, the norms of mental health are determined in accordance with generally accepted age stages of development based on genetic and cultural heritage. From the existing classifications of stages of development of an individual, in the most general form, the following main stages can be distinguished: 0 - 1, 1 - 3, 3 - 6(7), 6(7) - 13, 13 - 19, 19 - 60, 60 - until death .
The most important, basic in an individual’s life are the first 3 stages of development: 0 – 1, 1 – 3, 3 – 6(7), since these stages are what determine future mental and somatic health, character, emotional and volitional qualities, moral and ethical principles, behavioral stereotypes. It is during the period of development of a child up to 7 years old that the most active development of the brain occurs, the peak of neuroplasticity, which contributes to the accumulation and growth of adaptive mechanisms of the brain and the central nervous system as a whole.
It is believed that each stage of development for a child becomes the basis for the next stage of development, aimed at the further development of adaptation mechanisms. And, in fact, the concept of norm is assessed as the child’s ability to adapt to the environment, regardless of social, ethnic origin and in accordance with the tasks of the age stage, which in modern Russian psychology are determined by three factors: the social situation of development, the structure of consciousness and the leading type of activity.
Crisis of maladaptation of brain structures, mistaken for an age crisis
Child psychologists and psychotherapists working to overcome the various negative manifestations of MDM in preschool-age children often have to counsel parents who complain that their children's behavior is like one never-ending crisis. Trying to figure out what’s wrong, parents begin to visit different specialists in order to understand the real nature of the child’s maladjustment.
Other parents, on the contrary, are concerned that their children did not have any age-related crises and begin to worry that the harmonious development of their children up to 6 years old may later, in adolescence, lead to some kind of “super crisis”, since they did not “get over” the age-related crises of younger ages. In fact, what the so-called age-related crises are not the norm, as evidenced by the development and behavior of children who live their childhood safely without any age-related crises.
In the early 30s of the last century, periodic crises of maladjustment in children were called by the famous scientist L. S. Vygotsky age-related crises that every child must go through. Age crises were described by scientists in accordance with the stages of child development they identified: 0 - 1 year, 1 - 3 years, 3 - 7 years. Despite the fact that such famous psychologists as D.B. Elkonin [15], A.N. Leontiev [9], in subsequent years they recognized that age-related crises are not inevitable companions of a child’s mental development, that healthy children with a reasonably controlled educational process manage without manifestations of an age-related crisis; unfortunately, to this day in Russian psychology, age-related crises are traditionally recognized by many as the norm .
This, in our opinion, may be due to the fact that most clinical psychologists, child psychologists and neuropsychologists, due to the specifics of their work, encounter not healthy children, but children with minimal brain dysfunction (MBD). In addition, they traditionally perceive maladaptive crises as an age-related norm and often as a result of environmental influences, and not as a neurological problem of disruption of compensatory, adaptive mechanisms of the brain, the central nervous system, associated with the problem of disruption of the morphofunctional capabilities of the brain with the possible influence of environmental factors.
L.S. Vygotsky explained the concept of age-related crises by the fact that ontogenesis is a regular process of changing stable and critical ages, understanding the development of a child as discrete, revolutionary, and not evolutionary and continuous. The age crisis as a necessary transition to a higher stage of development, to the next psychological age, is determined, according to L.S. Vygotsky, the destruction of the usual social situation of development and the emergence of another [3].
As many researchers note, the peaks of maladjustment crises, including manifestations of attention deficit hyperactivity disorder, often occur at approximately 3 and 6 years of age. This is, in all likelihood, not due to the problem of the destruction of the social situation of development of the previous period, as L.S. believed. Vygotsky, but with the impossibility of solving the problems of the next stage of development.
The inability of the brain, and the central nervous system as a whole, to cope with new demands on the child under conditions of increasing mental and physical stress is explained, in our opinion, by the breakdown of the compensatory mechanisms of brain structures due to minimal birth injuries received by the child, which manifest themselves in children under 7 years of age with various syndromes and in different conditions. intensity.
The many faces of maladjustment in MDM
The absence of a diagnostic criterion for MDM in ICD-10 gives some specialists reason to believe that MDM is not a medical term, but a term coined by psychologists and speech therapists who refer completely healthy children to them. Often, a neurologist can explain inappropriate behavior, enuresis, tics, nail biting and other problems of a child by an age crisis, citing the fact that each child has an individual developmental norm and that there are no developmental norms now, and we must wait until the brain itself matures, and all the child’s problems will “outgrow” themselves. Until now, some neurologists, when detecting excessive hyperactivity of a child, consider this a sign of spoilage, without delving into the reasons for the manifestation of MDM, without, unfortunately, linking them with troubles in the intrauterine period, birth injuries or postpartum infections of the child.
The term MDM first appeared in the 30-40s of the last century. The term MDM received official recognition at the Oxford International Group for the Study of Child Neurology in 1962. It was recommended to include in this category children with mild neurological disorders, with problems in learning, behavior, with attention disorders with intact intelligence, but with signs of immaturity and delayed maturation of certain mental functions.
Until 1994, MDM was considered a clinical diagnosis in the ICD. Due to the diversity and heterogeneity of clinical manifestations, MDM was excluded as a diagnostic and clinical criterion in the new edition of ICD-10, and its various manifestations were scattered across different sections for the convenience of formal classification.
Extensive research led by the Czech doctor Z. Trzesoglava back in the seventies revealed a variety of neurotic signs in children with MDM: onychophagia, finger sucking, obsessive stereotypical movements and tics, increased anxiety and fearfulness, mental exhaustion, headaches with fatigue, impaired appetite, sleep , stuttering. In addition to impaired attention (93%), hyperactivity (80%), and impulsivity (65.7%), researchers noted many other clinical manifestations in the observed children: 77% had more than 5 minor neurological disorders (hyperkinesis, finger tremor, impaired coordination of movements etc.), in 71% of cases - increased emotional lability, irritability, tearfulness, in 68% - impaired visual perception and spatial orientation, in 50% of cases - speech and pronunciation disorders [13].
As a result of observing a large contingent of children and adolescents, a group of scientists led by Professor V.M. Troshin in the nineties noted that MDM can be considered as diffuse cerebral dysregulation, which causes a delay in the maturation of connections between different brain structures. Based on the results of this study, O.V. Khaletskaya, V.M. Troshin defined MDM as “the outcome of mild organic damage to the brain, against the background of which various neurotic reactions, behavioral disorders, difficulties in schooling, impaired maturation of higher brain functions, and various neurosis-like disorders are observed”[14].
Subsequent research, for example, under the guidance of Professor B.R. Yaremenko, it was recognized that MDM is an organic basis for the disharmonious development of higher mental functions, various autonomic and somatic disorders, neuroimmunological reactions, specific developmental disorders of the musculoskeletal system associated with prenatal damage and natal damage to the cervical vertebrae [16]. Some scientists (Fesenko Yu.A.) [13] consider MDM to be the cause of all borderline neuropsychiatric disorders.
Thus, in domestic neurology, MDM most often continues to be considered and studied by scientists as an important clinical category as a complex clinical problem and as an etiological factor in various clinical manifestations, while in many Western countries it is considered only within the framework of attention deficit hyperactivity disorder.
The role of neuroplasticity in MDM
The morphofunctional readiness of the brain to adapt to the environment, its neurobiological maturity based on phylogenetic heritage is closely related to plasticity - one of the most important properties of the brain and the nervous system as a whole, which allows you to adequately respond to the actions of environmental stimuli and contributes to the development of adaptation processes. Plasticity underlies the formation of reflexes, learning processes, restoration and replacement of a functional defect of the nervous system after injuries received, including after birth injuries in the form of MDM.
Plastic rearrangements are not limited to the morphological substrate, influencing structural and functional processes, providing constant plastic changes under the influence of the environment. However, brain plasticity is not always able to carry out compensatory changes and ensure the overlap of impaired functions. This occurs, in particular, due to quantitative and qualitative dysregulation, for example, due to chronic brain hypoxia, which involves the brain in the pathological development of intrasystem, intersystem and interhemispheric connections.
Due to the fact that plasticity regulates not only the compensatory mechanisms of the brain, but also the development of pathological processes, forming generations of pathologically enhanced excitation - a pathological system, the latter lead to the formation of a neuropathological syndrome, or a crisis of dysregulation.
As a result of neuroplasticity, “a pathological system can be formed from primary and secondary altered parts of damaged systems, turning into endogenous mechanisms for the further development of the pathological process” [8].
In all pathological processes, disturbances in metabolism and the function of the corresponding brain structures are observed. In this understanding of dysregulatory, or maladaptive, crises as a pathological system, neither epileptic seizures nor systemic neuroses can be explained by the manifestation of compensatory mechanisms of the brain, as some scientists are trying to prove.
An example of such an attempt to “justify” a dysregulatory crisis with compensatory mechanisms is, in our opinion, the following statement: “Hyperactivity is a kind of protective mechanism that temporarily restores normal connections in the cerebral cortex and thereby preserves the intellectual development of the child” [13] or: “Hypothesis of the compensatory mechanism of enuresis: up to a certain time, the act of involuntary urination is “needed” by the body to normalize sleep functions, since with its help the “switching” of sleep stages occurs” [13].
On the contrary, dysregulatory, or maladaptive, crises, no matter in what form they manifest themselves (hyperactivity, enuresis, logoneurosis, alalia, obsessive movements, onychophagia, tics, affective reactions, aggressiveness, stuttering, etc.), as a rule, are an indicator of a breakdown of compensatory capabilities of the central nervous system. And at the same time, they indicate that subtle signs of MDM were not diagnosed or treated until 1 year of age, which gradually led to disregulation crises due to the formation of pathological systems, or determinants, that peak at approximately 3–6 years.
MDM is considered to be the result of organic brain damage in children, but it passes into the present residual stage, in fact, due to the high neuroplasticity and replacement abilities of the brain, only after the first year of the child’s life. From 1 year to 7 years, while the brain and central nervous system continue to remain sufficiently plastic and responsive to regular comprehensive rehabilitation measures, the latter have the most positive effect on the restoration of the consequences of damaged brain structures and functional connections between them.
However, the same high neuroplasticity against the background of MDM with chronic cerebral hypoxia, hypertension, hydrocephalus without effective treatment can form pathological systems, dysregulatory mechanisms that underlie the development of neuroses, psychogenia, paroxysms, motor, behavioral, cognitive, speech and other disorders.
MDM - time bomb
If we use the term “birth injuries”, meaning all the unfavorable development factors from intrauterine to postpartum complications of the child, then, as is known, almost all newborns receive birth injuries of varying degrees. Thanks to the neuroplasticity of the central nervous system, some children with microdamages of the brain substrate are completely restored without external intervention in a favorable environment. It is believed that it is these children who have the opportunity for evolutionary progressive development without any dysregulation or maladaptation crises, which is considered a sign of healthy mental and physical development, or the norm.
Considering the high prevalence of MDM as residual phenomena of birth injuries in the prenatal, natal and postnatal periods (according to various studies, from 21 to 99%), which in the future causes up to 80% of various neuropsychic, somatic, cognitive disorders of children and adults, it is important note the timeliness of identifying symptoms at risk of developing MDM.
Symptoms are considered minimal only because they are hardly noticeable, but in reality they represent a serious medical and social problem. Various mild neurological disorders in the first months of a child’s life, unfortunately, do not attract the attention of specialists, especially inexperienced parents.
However, as the child grows and develops, birth injuries can gradually manifest themselves in different clinical forms. For example, in the form of a sluggish sucking reflex, lack of appetite, restless sleep, frequent crying for no reason, decreased or increased muscle tone, asymmetry of the halves of the body, unusual postures, greater or less than normal weight, any lag from generally accepted norms of age-related development.
In most cases, MDM is diagnosed only at approximately 3–6 years of age, when pathological determinants have already formed and long and persistent treatment is required to minimize the consequences of MDM, depending on the clinical variant of the pathological process. If rehabilitation measures for such a manifestation of MDM as hyperactivity syndrome are applied by specialists to children from 2-3 years of age, then, most often, by the age of 7, most maladaptive manifestations can be overcome.
If children begin to receive the necessary treatment later, at 6-7 years of age, then, unfortunately, children with MDM who have delays in mental and speech development, problems of hyperactivity and attention disorders may develop school and social maladaptation in primary school and adolescence. or there will be a need to study in correctional classes of different levels.
As most researchers note, diagnosis and treatment of clinical manifestations of MDM should be as early as possible, when the compensatory capabilities of the brain are still great, before a pathological stereotype has formed. Many scientists and practitioners emphasize the need for clinical monitoring of children with MDM from birth to 8 years.
The reason for registering with a neurologist is any complicated childbirth. You should be wary of all the so-called conditionally indirect signs of MDM. Among them, for example, the following can be noted: hydrocephalic and hypertensive syndromes, torticollis, malpresentation of the fetus, absence of a cry or a weak cry after childbirth, asphyxia of varying nature and intensity, rapid labor, tight entanglement of the umbilical cord, a long anhydrous period, cesarean section, multiple pregnancy, Rh incompatibility, prematurity or postmaturity of the fetus, too much or too little weight, instability of the cervical vertebrae, severe pregnancy, intrauterine infection, etc.
MDM is considered the mildest outcome of perinatal injuries compared to two other types of clinical manifestations depending on the severity of brain damage and location: cerebral palsy with severe motor impairment, which can be accompanied by intellectual defects of varying degrees, and organic damage to the central nervous system with severe cognitive defects and/or manifestations of RDA with mild motor impairment.
Birth injuries, or birth injuries, received by children with cerebral palsy and children with MDM are assessed as diffuse brain lesions and have the same causes of origin, differing only in the severity of the lesion. Due to the fact that most children with cerebral palsy begin to receive the necessary regular treatment immediately after birth, then, especially with moderate and mild forms of cerebral palsy, most of the damaged brain structures are restored in sick children. Numerous studies show that this demonstrates the enormous compensatory capacity of the brain associated with plasticity, which can be activated with the help of well-chosen treatment. With complex regular treatment of mild forms of cerebral palsy, begun immediately after birth, the consequences of cerebral palsy are minimal or completely unnoticeable.
At the same time, the experience of monitoring children with MDM up to the age of seven while staying in a psychoneurological sanatorium shows that among them there are practically no children who received any treatment before the age of 1 year. Most often, they do not receive any treatment at their place of residence, not to mention the necessary comprehensive treatment. When examined in a sanatorium, they often exhibit many manifestations of MDM.
Thus, taking into account the negative consequences that MDM leads to, we consider it necessary to pay attention to the importance of early diagnosis of MDM, both by indirect signs in accordance with the norms of child development, and with the use of modern methods of hardware diagnostics, as well as the organization of comprehensive regular treatment in during the first year of the child’s life and follow-up with a neurologist for children with MDM up to 8 years of age.
As is known, the exclusion of the diagnostic and clinical term MDM from ICD-10, which made it possible to dissolve it in various syndromic manifestations, does not mean that such a diagnosis does not exist. Considering MDM only in the format of attention deficit hyperactivity disorder narrows the problem to behavioral and cognitive disorders, when its other clinical manifestations are considered as concomitant or separate nosological forms, and not as a negative result of one pathological process. This generally changes the picture of understanding the etiology of MDM and the need for an individual approach to the treatment of MDM, depending on the characteristics of the manifestation of the syndrome or a combination of syndromes within one diagnosis.
In order to promptly begin correctional classes with the involvement of various specialists, to provide adequate psychotherapeutic assistance to children with MDM in a timely manner, it is important to consider maladaptive, or disregulatory, crises precisely as manifestations of a breakdown of the compensatory mechanisms of the brain in children with MDM, and not to perceive this as a mandatory manifestation of an age-related crisis , as previously thought.
It is hoped that timely diagnosis and treatment of MDM as an important medical and social problem will finally become a priority in modern neonatology, child neurology, psychiatry, psychology, psychotherapy and pediatrics, taking into account an interdisciplinary approach.
The abstracts of the report at the International Conference in Moscow were published in the journal “Psychotherapy” (2012)
Diagnosis of MMD
MMD is diagnosed using several methods. Most often, specialists collect anamnesis and conduct physical and laboratory tests. Using anamnesis, you can determine the etiology and detect primary symptoms. Such information at the age of 3 to 6 years helps to determine the severity and neglect of the syndrome. Speaking about physical research, special emphasis is placed on the physiology of the child, the work of her reflexes and their symmetry.
A complete examination of a school-age child will not provide a lot of useful information; nevertheless, the main role in the examination is played by psychological diagnostics, which allows the doctor to understand at what level of development the child is and what the degree of his illness is. When examining, most doctors use proven and reliable Gordon or Wechsler tests.
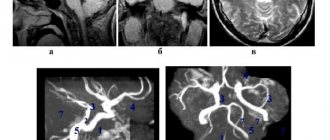
It is extremely important to assess the state of the central nervous system. The assessment is determined using EEG studies, rheo- and echoencephalography, neurosonography, computed tomography and magnetic tomography. In the diagnosis of minimal cerebral dysfunction syndrome, tests obtained using CT or MRI play an important role.
Treatment of MMD in children
MMD in children is treated comprehensively, including both pedagogical and psychotherapeutic interventions. In addition to social correction methods, treatment with pharmaceuticals and physical education is used to develop the body, muscles, and bone health. Of course, the most important role is given to social correction, which helps the child adapt to society and the team, as well as cure the psychological symptoms of the disease: isolation, detachment, selfishness, and so on.
The importance of the parental factor cannot be excluded from the list of procedures and techniques important for treating a child. During MMD, specialists place great emphasis on the microclimate in the child’s family. Doctors recommend that parents more often resort to “encouragement”, that is, praising the child for any success, both at school and in society; use less constructions using the words “no” and “cannot”.
It is better to reduce the amount of time spent on the computer, phone, or set-top box. Children with MMD need games that involve attentiveness, concentration, and activity, that is, they should choose reading, puzzles, construction sets, and drawing. This will improve memory, reading, logic, writing.
It will not be possible to do without pharmaceutical drugs that help relieve individual symptoms. The prescribed courses directly depend on the degree, neglect and symptoms of the disease. Sedatives, tranquilizers, and antidepressants can be used. In addition to medications, they often resort to the use of massages and exercise therapy. Methodically, sports exercises are introduced into treatment, affecting the correction of movement, dexterity, and physical fitness. The child learns to swim, run properly, ski, roller skate, and skate.
SELECTION OF TREATMENT SCHEME
Correcting minimal brain dysfunction in children requires an integrated approach. Usually, an individual program is drawn up for each child, which takes into account the characteristics of the clinical picture and etiology.
MMD therapy is carried out in several areas:
- Pedagogical methods help minimize the consequences of social and pedagogical neglect and promote the child’s adaptation to the team. Social educators work not only with the child, but also with his parents. They advise encouraging the child, focusing on his successes and achievements, using the words “no” and “no” less, talking to the child with restraint, calmly and gently. Watching TV and playing on the computer should take no more than 40-60 minutes a day. Preference should be given to such games and activities that involve attention and concentration (puzzles, construction sets, drawing, etc.).
- Psychotherapeutic methods are aimed at correcting mental retardation. A psychologist and psychotherapist chooses ways to influence his little patient based on his age. If the child is still too young to contact the doctor, then the work is carried out mainly with his parents. It is necessary that a positive psychological microclimate be established in the family - the outcome of treatment largely depends on this.
- Drug treatment is prescribed extremely rarely. Taking medications allows you to relieve individual symptoms, for example, sleeping pills help normalize sleep, sedatives help calm an overly excitable baby, etc. In some cases, stimulants, tranquilizers and antidepressants may be recommended.
- Physiotherapy can improve the functioning of the nervous system, both central and peripheral, as well as restore their functioning as much as possible. The most effective in correcting this type of disorder are various types of massage, hydrokinesitherapy, and a set of therapeutic exercises. Sports activities such as running, cycling or skiing, as well as swimming will be useful. During sports activities, the child must concentrate and show dexterity, and this also has a positive effect on the treatment process for MMD.
Experts in most cases give positive prognoses for children with MMD. Approximately 50% of patients “outgrow” their disease, and in adolescence and adulthood the symptoms of the pathology disappear completely. However, in a number of patients, some of the manifestations of the disease remain for life.
People with MMD are characterized by inattention and impatience, they have difficulty communicating with people around them, they often have problems in their personal lives and when trying to create a full-fledged family, and it is difficult for them to learn professional skills.
Predictions and prevention
Experts' forecasts for children with MMD are usually positive and favorable, because in extremely rare cases, the childhood disease develops into adolescence or even adulthood - often the disease and symptoms disappear in childhood. In rare cases, the psyche is disturbed during treatment. Preventive measures include a rational diet for the mother, giving up bad habits, regular visits to antenatal clinics to monitor pregnancy and treat concomitant pathologies, and a full examination to select the most appropriate method of delivery.