Clinical syndromes and symptoms of ischemic stroke in the posterior cerebral artery territory
The localization of atheromatous lesions in the posterior cerebral artery or at the beginning of one of its branches, as well as the degree of narrowing, usually determine the onset, severity and nature of the clinical syndrome.
Other factors, including collateral flow through the posterior communicating artery or cortical branches and blood viscosity, also play a significant but less important role. However, even in the presence of an atherosclerotic plaque in the posterior cerebral artery, the mechanism responsible for the development of stroke is usually embolic occlusion of this artery or its branches. Changes in the posterior cerebral artery cause the appearance of syndromes, which are divided into two groups:
- Syndromes of damage to the midbrain, subthalamus and thalamus associated with atherosclerotic narrowing, atherosclerotic or embolic occlusion of the proximal precommunal segment of the posterior cerebral artery or the beginning of its penetrating branches
- Syndromes, cortical lesions caused by atherosclerotic narrowing, atherothrombotic or embolic occlusion of the postcommunal segment of the posterior cerebral artery
Proximal precommunal syndromes (central territory)
When the trunk of the posterior cerebral artery is occluded, an infarction develops with unilateral or bilateral involvement of the subthalamus and medial thalamus, as well as a lesion on the same side of the cerebral peduncle and midbrain with corresponding clinical symptoms. Obviously, with a non-functioning state of the posterior communicating artery (for example, its atresia are also symptoms of damage to the peripheral territory supplied by the post-communal segment of the posterior cerebral artery). If complete occlusion does not occur at the beginning of the posterior cerebral artery, then hemiplegia with infarction of the cerebral peduncle rarely develops. Partial proximal lesion syndromes suggest occlusion of the middle cerebral thalamo-perforating artery, but do not confirm it.
In superior lesion syndrome, characterized by involvement of the red nucleus and/or dento-rubro-thalamic tract, severe contralateral ataxia is noted.
In inferior lesion syndrome, third cranial nerve palsy and contralateral ataxia (Claude syndrome) or third cranial nerve palsy combined with contralateral hemiplegia (Weber syndrome) are observed.
When the subthalamic body of Lewis is involved in the process, contralateral hemiballismus may occur.
Occlusion of the artery of Percheron causes upward gaze paresis and hypersomnia. Such a lesion is often accompanied by abulia and a state of euphoria that contributes to the onset of abulia.
and MRI of the brain can detect bilateral lesions resembling a butterfly in their outlines in the subthalamus and middle lower parts of the thalamus. Extensive foci of infarction in the midbrain and subthalamus with bilateral occlusion of the trunk of the posterior cerebral artery usually develop secondary to embolism. In such cases, deep coma, bilateral pyramidal symptoms and “decerebrate rigidity” are observed.
Atheromatous occlusion of the penetrating branches of the thalamic and thalamo-geniculate group in their initial sections leads to the appearance of thalamic and thalamo-capsular lacunar syndromes. The most famous is the Dejerine-Roussy thalamic syndrome. Its main manifestations are contralateral loss of both superficial (pain and temperature) and deep (tactile and proprioceptive) sensitivity according to the hemitype. Sometimes only pain and temperature or vibration and muscle-joint sensitivity are affected. Most often, disorders are detected in the area of the face, arm, hand, torso, leg and foot, less often - only in one limb. Hyperpathy often occurs, and after several weeks or months, excruciating burning pain may develop in the affected areas. Patients describe it as squeezing, constricting, icy, cutting. This pain is persistent, debilitating, and poorly responsive to analgesics. Anticonvulsants are sometimes effective.
When the internal capsule is involved in the lesion of the posterior thigh, hemiparesis or hemiplegia is detected in combination with hemitype sensitivity disorders. Other associated movement disorders include hemiballismus, choreoathetosis, intention tremor, incoordination, and postural alignment of the hand and arm, especially during walking.
Post-communal syndromes (peripheral or cortical territory)
Infarcts in the area of the thalamus cushion can occur when there is obstruction of the posterior thalamic thalamo-geniculate penetrating branch of the postcommunal portion of the posterior cerebral artery. Occlusion of the peripheral portion of the posterior cerebral artery itself most often leads to the development of infarctions of the cortical surface of the medial side of the temporal and occipital lobes. A common symptom is contralateral homonymous hemianopsia. If the associative visual fields remain intact and only the cortex near the calcarine sulcus is involved in the pathological process, the patient suddenly feels a visual defect. Sometimes only the upper quadrant of the visual field is missing. Central vision can remain intact if the blood supply to the apex of the occipital pole is maintained from the branches of the middle cerebral artery.
When the medial temporal lobe and hippocampus are involved, sudden memory disturbances may occur, especially when the dominant hemisphere is affected, but these disturbances usually disappear because memory functions are carried out by both hemispheres of the brain.
With damage to the dominant hemisphere with the spread of the infarction in the lateral direction deep into the white matter with the involvement of the splenium of the corpus callosum in the pathological process, the development of alexia without agraphia is possible. Visual agnosia for faces, objects, mathematical symbols, and colors, as well as anosmia with paraphasia (amnestic aphasia), may also occur, even in the absence of damage to the corpus callosum.
With occlusion of the internal carotid artery, severe stenosis or occlusion of the posterior cerebral artery on the same side can reduce blood flow in the area of adjacent blood supply to the posterior and middle cerebral arteries. This often leads to visual agnosia, visual neglect and the inability to count objects located in the opposite half of the visual field. Sometimes occlusion of the posterior cerebral artery is accompanied by peduncular hallucinosis (visual hallucinations in the form of brightly colored scenes and objects), but the exact localization of the infarction in such cases remains not entirely clear.
Bilateral infarctions in the blood supply of the distal posterior cerebral artery lead to the development of cortical blindness. The patient is often unaware of the existing visual disturbances, but the pupil reacts normally to light. Even when the visual defect is completely unilateral or bilateral, small islands of vision may remain; in this case, the patient usually reports instability of vision, the impression that he manages to retain images of objects due to the preservation of the vision of their individual parts. In rare cases, only peripheral vision is lost, while central vision remains intact; in this case, the patient reports the presence of tubular vision.
Optical ataxia (inability to exercise visual control over the movements of the limbs), ocular ataxia (inability to shift the gaze to a certain point in the visual field), inability to count objects depicted in a picture or form an idea of the image in a picture, inability to avoid objects encountered along the way are characteristic of bilateral lesions of the associative visual pathways. This combination of symptoms is called Balint syndrome. It is usually observed in bilateral infarctions, which are believed to develop against the background of decreased blood flow in the distal posterior cerebral artery in the area adjacent to the middle cerebral artery, which occurs during cardiac arrest.
Finally, occlusion of the upper part of the basilar artery, usually caused by embolism, can give a clinical picture that includes all or any of the symptoms of damage to the central or peripheral territory of the blood supply. Pathognomonic for it are the sudden onset of the disease and the bilateral nature of the symptoms.
Variations in the development of cerebral arteries and epilepsy
The prevailing ideas about the mechanisms of development of cerebral ischemia imply the occurrence of a discrepancy between the available blood supply and the needs of brain tissue. The most important achievements in the field of clinical angioneurology include the modern concept of heterogeneity of ischemic stroke, which is based on the idea of the diversity of causes and mechanisms of development of acute focal ischemic brain damage. The amount of reversible and irreversible brain damage largely depends on the state of the hemodynamic, collateral, perfusion and metabolic reserves of the brain. Pathological tortuosity of the main arteries of the head - a hereditarily determined functional inferiority of connective tissue - occurs in at least 10% of the population. Among the main forms of lesions of intracranial arteries, kinks and loop formations, aneurysmal dilatations of arteries, and arteriovenous aneurysms are distinguished. Excessive tortuosity of blood vessels contributes to the formation of blood clots in them. In 71% of patients with arterial occlusion, a tortuous course of vessels was noted. Underdevelopment of the cerebral arteries in the form of hypoplasia or stenosis of the posterior inferior cerebellar artery and/or basilar artery, rarely the inferior anterior cerebellar artery and tortuosity of the vertebral artery are causes of hearing loss and deafness. Weak cerebral artery anastomoses cause cerebral ischemia after cervical discectomy. In Parkinson's and Alzheimer's diseases, neuroimaging and pathological studies have detected cerebrovascular lesions in 20-30% of cases, and vascular disease of the brain may be the basis of dementia. Structural changes in cerebral vessels, a decrease in blood flow velocity and the presence of 30% stenosis in the middle cerebral artery can be prerequisites for the development of stroke in patients with sleep apnea syndrome.
In case of Kimmerle anomaly, it is necessary to take into account the presence of congenital changes in the vertebral arteries. Dysplastic disorders in the area of the craniovertebral junction are 2 times more often noted with pathological tortuosity of the vertebral arteries, to a lesser extent due to hypoplasia of the vertebral arteries. Up to 51.9% of patients with Chiari malformation and syringomyelia have structural features of the cerebral arterial circle. Tortuosity, asymmetry and hypoplasia of the vertebral arteries with signs of impaired blood flow are characteristic of vertebrobasilar insufficiency due to cervical dorsopathy and were noted in 76.6% of cases with central vestibulocochlear syndrome.
The arterial bed of the brain is also affected in such systemic diseases of the body as rheumatoid arthritis, polyarteritis nodosa, Takayasu's disease, Henoch-Schönlein disease. When performing dental procedures in patients with Sturge-Weber disease or Recklinghausen disease, as typical neurofibromatosis, the development of threatening bleeding is possible. Primary damage to the cerebral arteries in the form of vasculitis and endarteritis underlies the development of neurosyphilis and leads to secondary damage to the nervous tissue and the occurrence of infarctions in the brain. Cerebral vasculitis and herpetic cerebral vasculitis can develop against the background of herpetic infection. With ischemic strokes, in 70% of cases in the brain tissue, along with changes caused by acute cerebrovascular accident, focal lesions are observed, similar to changes in meningoencephalitis caused by herpes zoster and herpes simplex.
Changes in the structure of the cerebral arteries must be taken into account when assessing cancer metastases, as well as in 40% of patients with severe traumatic brain injury when identifying traumatic subarachnoid hemorrhages and concomitant angiographic vasospasm.
In the course of carrying out research to study the relationship between variants of human cerebral arteries and cerebrovascular disorders within the framework of acute cerebrovascular accidents and chronic cerebral ischemia, we have developed observations about the relationship between variants of the structure and topography of human cerebral arteries with a number of other nosological units. In this regard, we present the results of our own research on the development of cerebral arteries in humans with various types of epilepsy.
We analyzed the state of the arterial bed of the brain in 748 outpatient and inpatient patients from 22 years to 81 years old, who were examined and treated in the neurological and neurosurgical departments of OKB No. 2 named after. Professor I.N. Alamdarov, Astrakhan in the period 1983-1998, the neurological departments of City Hospital No. 3 and City Hospital No. 4 of Tambov, the neurosurgical department of the Tambov Regional Hospital, the rehabilitation and health complex of the family “B. Lipovitsa", neurological offices and in day hospitals of City Hospital No. 4, Nodal Clinic at the station. Tambov JSC "Russian Railways" and the Central House of Children's Hospital "Tambovmedservice" LLC, as well as in the outpatient clinic "Home Doctor" (Tambov) during 1998-2009.
All patients underwent a comprehensive clinical and instrumental study, including data from a clinical examination by a neurologist, therapist and ophthalmologist, standard laboratory data, electrocardiography, fluorography or plain radiography of the chest organs. According to indications, consultations and examinations were carried out with a neurosurgeon, gynecologist, otolaryngologist, cardiologist, endocrinologist and psychotherapist; a study of the cognitive sphere using a brief mental status assessment scale or a mini-mental status study, transcranial Doppler sonography, electroencephalography. All patients underwent magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA).
According to the data obtained, variants of the structure and topography of the arterial circle of the cerebrum were verified in only 27 cases (61.4% of observations) out of 44 patients with epilepsy or encephalopathies with leading epileptiform syndromes. Among the analyzed group of patients with various types of epilepsy, the following variants of the structure and topography of the arterial circle of the cerebrum were identified: 1) bending of both anterior cerebral arteries in 1 (3.7%) patient; 2) hypoplasia of the left vertebral artery in 2 (7.4%) patients; 3) posterior trifurcation of both internal carotid arteries and anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 3 (11.1%) patients; 4) anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 6 (22.2%) patients (Fig. 1); 5) hypoplasia of the right vertebral artery, aplasia of the posterior communicating artery on the right in 4 (14.8%) patients; 6) hypoplasia of the right vertebral artery, hypoplasia of the basilar artery in 5 (18.5%) patients (Fig. 2); 7) anterior trifurcation of the left internal carotid artery, hypoplasia of the posterior communicating artery, hypoplasia of the right posterior cerebral artery in 3 (11.1%) patients; tortuosity of both vertebral arteries in 2 (7.4%) patients; 9) hypoplasia and tortuosity of both vertebral arteries in 1 (3.7%) patient. Below are quite indicative clinical observations from the totality of our own studies.
Among the analyzed group of patients with various types of epilepsy, the following variants of the structure and topography of the arterial circle of the cerebrum were identified: 1) bending of both anterior cerebral arteries in 1 (3.7%) patient; 2) hypoplasia of the left vertebral artery in 2 (7.4%) patients; 3) posterior trifurcation of both internal carotid arteries and anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 3 (11.1%) patients; 4) anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 6 (22.2%) patients (Fig. 1); 5) hypoplasia of the right vertebral artery, aplasia of the posterior communicating artery on the right in 4 (14.8%) patients; 6) hypoplasia of the right vertebral artery, hypoplasia of the basilar artery in 5 (18.5%) patients (Fig. 2); 7) anterior trifurcation of the left internal carotid artery, hypoplasia of the posterior communicating artery, hypoplasia of the right posterior cerebral artery in 3 (11.1%) patients; tortuosity of both vertebral arteries in 2 (7.4%) patients; 9) hypoplasia and tortuosity of both vertebral arteries in 1 (3.7%) patient. Below are quite indicative clinical observations from the totality of our own studies.
Example 1. Patient N., 54 years old, is observed in the Nodal clinic at the station. Tambov JSC "Russian Railways" with a diagnosis of encephalopathy as unspecified (epileptic and dyscirculatory) with polymorphic paroxysms (like Todd's palsy) against the background of abnormalities in the structure of the cerebral arteries. Complaints of noise in the head, unsteadiness when walking, attacks of weakness in the right limbs and loss of consciousness. Neurologically: there are no meningeal signs in consciousness, cognitive functions are reduced, emotionally labile, pupils d = s, convergence is weakened, slight weakness of the facial muscles on the right, paresis of the right hand up to 4 points, no sensory disorders, tendon reflexes are increased d > s, staggering in the Romberg position , coordination tests are performed with DetS missing, eyelid tremor. Ophthalmologist: hypertensive angiosclerosis of the retinal vessels of both eyes. Therapist: stage II hypertension, severity of arterial hypertension II, risk category 3. BAC: cholesterol - 4.5 mmol/l, β-lipoproteins - 3.5 g/l, creatinine - 69 µmol/l, urea - 7, 9 mmol/l. Prothrombin - 88%, fibrinogen - 4.25 g/l. ECG: syn, rhythm 80 per minute, normal position of the EOS. MRI and MRA: shown in Figure 1. Outpatient treatment: piracetam, glycine, Cavinton, cinnarizine, aminalon, Enap, Prestarium, indopamine. She underwent a course of treatment in a day hospital: Mexidol, magnesium sulfate, Prestarium, indopamide, mildronate, enalapril. The complaints remain the same. Neurologically - there are no meningeal signs in consciousness, cognitive functions are reduced, cranial nerves without dynamics, paresis of the right hand up to 4.5 points, staggering in the Romberg test, coordination tests with intention on both sides. Consulted at the Tambov psychiatric hospital, where a diagnosis was made: consequences of organic damage to the central nervous system of complex origin with polymorphic paroxysms. EEG: pronounced cerebral changes in biological and bioelectrical activity, practically no α-activity. In all regions the polyri is less than 5 μm. There is no regionality, no activation reaction, no assimilation. Persistent disorganization of the activities of central structures. Interest in the left temporal region, where a focus of slow-wave irritation was identified. Low functional state of the cortex with high sensitivity to hypoxia, with a decrease in the threshold of excitability of the trunk. Single discharges of the posterior trunk sections. Vascular influences are pronounced. Follow-up: while taking Depakine-Chrono, complaints decreased significantly, no attacks were noted.
Example 2. Patient VN., 21 years old, is observed in the Nodal clinic at the station. Tambov JSC Russian Railways with a diagnosis of epilepsy with polymorphic cerebral paroxysms and cognitive impairment. Observed since childhood - complaints of attacks with loss of consciousness. After starting treatment at the age of 14 in the neurological department of the Tambov Regional Children's Hospital, he was registered with a diagnosis of epilepsy, partial seizures with secondary generalization. EEG (Psychiatry and Narcology, 04/17/02): no paroxysmal activity was detected, unstable α-rhythm. Dysfunction of the diencephalic region. Vascular influences with increased autonomic excitability (06/15/04): AMI is moderate, but persistent, with low-amplitude dysrhythmia. Regionality is unclear. The activation reaction is reduced, there is no assimilation. No gross slow-wave or paroxysmal activity was detected. Reduced reactivity of the cortex. High vegetative excitability. Vascular influences 02.22.05: compared to 06.15.04, positive dynamics. General cerebral changes are moderate and of a regulatory nature. Moderate dysfunction of the diencephalic region with increased activity. An unstable α-rhythm appeared, fragmented. The reactivity of the cortex has improved. The sensitivity of the cortex to RFS has increased somewhat, which leads to a decrease in the threshold of excitability of the posterior brainstem structures. There are no paroxysmal tendencies of the cortex. Increased autonomic excitability. MRI and MRA: shown in Figure 2. Neurologically: there are no meningeal signs in consciousness, cognitive functions are slightly reduced, emotionally labile, distal hyperhidrosis, tremor of the eyelids and outstretched fingers, pupils d = s, converges, weakness of facial muscles on the right, in the Romberg position lung staggering, performs coordination tests, paresis, no sensory disorders, tendon reflexes d = s, Babinski's symptom is weakly positive on both sides, Epileptologist: cognitive disorders due to epilepsy. He constantly receives finlepsin (attacks are associated with irregular use of the drug).
Thus, we consider it necessary to draw the following conclusions. 1. Variations in the structure and topography of the arterial circle of the cerebrum can be considered as predictors of epileptiform phenomena in brain structures. 2. For various cerebral paroxysms, it is obviously advisable to study the arterial circle of the cerebrum. 3. Variants of the structure and topography of the arterial circle of the cerebrum in each specific case should be considered from the point of view of minor developmental anomalies.
Diagnosis and laboratory examination of ischemic stroke in the posterior cerebral artery territory
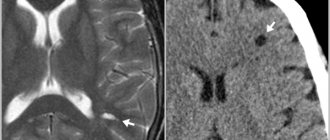
Infarction in the peripheral territory of the posterior cerebral artery can be easily diagnosed using magnetic resonance imaging (MRI) and computed tomography (). Meanwhile, the data are not sufficiently reliable for infarctions in the central zone of the blood supply of the posterior cerebral artery, especially those developing secondary to occlusive lesions of the penetrating branches of the posterior cerebral artery. Magnetic resonance imaging (MRI) of the brain can detect infarcts of this location with a diameter of more than 0.5 cm.
Angiography remains the only method that convincingly demonstrates atherosclerotic changes or embolic lesions of the posterior cerebral artery. The latest type of modern spiral computed tomography angiography (SCT angiography) with intravenous contrast makes it possible to identify occlusive lesions of small penetrating branches of the posterior cerebral artery.
MRI of the brain of a patient with intracerebral hemorrhage in the thalamus (indicated by arrows).
Thus, diagnosis of ischemic stroke in the posterior cerebral artery basin is based mainly on clinical data confirmed by the results of magnetic resonance imaging (MRI) and computed tomography angiography (CT angiography) with intravenous contrast.
Syndrome of blood flow insufficiency in the arteries of the vertebrobasilar system
Maksimova M.Yu., Piradov M.A. RMJ. 2021. No. 7. pp. 4-8 The article is devoted to the problem of blood flow insufficiency syndrome in the arteries of the vertebrobasilar system. Methods for diagnosing and treating vertebrobasilar insufficiency are presented, which should be aimed at preventing its progression, improving blood supply to the brain, and correcting certain syndromes and symptoms.
The independent clinical concept of “blood flow insufficiency syndrome in the arteries of the vertebrobasilar system” was formed in the 1950s, during the period of revision of views on the pathogenesis of ischemic cerebrovascular accidents (CVA) and the emergence of the concept of the leading role of cerebrovascular insufficiency in this case [1]. The peculiarities of the structure and functions of this arterial system, which provides nutrition to vital structures of the brain, and the uniqueness of clinical symptoms in case of disturbances of blood flow in it led to its identification in the latest version of the international classification into an independent symptom complex - “vertebrobasilar arterial system syndrome” within the framework of “transient transient cerebral ischemic attacks (attacks) and related syndromes” (International Classification of Diseases, 10th Revision, G45.0). Even earlier, a group of experts from the World Health Organization defined “vertebrobasilar insufficiency” as “a reversible impairment of brain function caused by a decrease in the blood supply to the area supplied by the vertebral and basilar arteries.” The ischemic nature and reversible nature of the disorders were emphasized, but the duration of neurological symptoms was not indicated, which previously did not allow them to be classified as transient ischemic attacks (TIA) and which has now become possible. Blood flow disturbances in the arteries of the vertebrobasilar system account for about 70% of all TIAs. Stroke with localization of focal changes in areas of the brain that receive blood through the arteries of this system develops 2.5 times less frequently than in regions belonging to the arterial basins of the carotid system [1].
Causes of blood flow insufficiency syndrome in the arteries of the vertebrobasilar system
The main causes of blood flow insufficiency syndrome in the arteries of the vertebrobasilar system, caused by arterial hypertension (AH) and atherosclerosis (AS), include [1, 2]:
- atherostenosis or atherobliteration of one of the vertebral arteries;
- characteristic arterial tortuosity, which in some cases can lead to kinking of the vertebral artery with the formation of septal stenosis and disruption of blood flow in it;
- congenital anomalies of the vertebral arteries (hypoplasia of one of the vertebral arteries, lateral displacement of the mouth of the vertebral artery), in which the insufficiency of blood flow in one of the vertebral arteries is compensated by another vertebral artery, but decompensation occurs against the background of AS and hypertension;
- compression of the vertebral artery by an osteophyte in the bone canal of the cervical spine, an articular process with instability of the cervical spine, an accessory cervical rib, a spasmodic neck muscle (posterior scalene muscle, longus colli muscle, inferior oblique muscle of the capitis), which is most often observed with congenital abnormally high entry vertebral artery into the spinal canal - at the level of 3–5 cervical vertebrae.
The syndrome of blood flow insufficiency in the arteries of the vertebrobasilar system can also be observed:
- with subclavian “steal syndrome”, in which, as a result of occlusion of the subclavian artery, blood flows not only to the entire vertebrobasilar system, but also to the arm through only one vertebral artery;
- with occlusion or severe atherostenosis of both internal carotid arteries
(ICA), since the vertebrobasilar system plays a significant role in the blood supply to the cerebral hemispheres and, under certain conditions, “steal syndrome” may occur; - with disturbances of general hemodynamics.
Subclavian “steal syndrome” is characterized by a phenomenon when a patient, during intensive work of the arm (retrogradely supplied with blood from the contralateral vertebral artery), experiences brainstem symptoms - most often dizziness. A certain contribution to the development of blood flow deficiency syndrome in the vertebrobasilar system can be made by changes in the rheological properties of blood (increased levels of fibrinogen, blood viscosity, platelet aggregation and hematocrit, increased rigidity of erythrocytes), leading to deterioration of microcirculation.
Diagnosis of blood flow insufficiency in the arteries of the vertebrobasilar system
Subjective data
The diagnosis of insufficiency of blood flow in the arteries of the vertebrobasilar system is based on a characteristic symptom complex that combines several groups of clinical symptoms found in patients with AS and hypertension.
These are visual and oculomotor disorders, disorders of statics and coordination of movements, vestibular disorders. In this case, the presumptive diagnosis is determined on the basis of at least two of these symptoms. They are short-lived and often go away on their own, although they are a sign of impaired blood flow in the arteries of this system, which requires clinical and instrumental examination. A thorough medical history is especially necessary to clarify the circumstances of the occurrence of certain symptoms [1, 2]. Visual disturbances
include a feeling of blurred vision, photopsia, scotoma, changes in visual fields, decreased visual acuity and are associated with transient ischemia of the occipital lobes of the brain.
Blurred vision in the form of a veil before the eyes and blurred vision often occurs at the height of a headache. Photopsia appear in the form of flashes of colored dots, most often red or green, black, with a light halo, as well as spots, fiery lightning, lines, rings, zigzags. Photopsia differ from the rainbow circles characteristic of glaucoma in that their appearance is not associated with an external light source; they also occur with closed eyes. Changes in visual fields are usually observed in the form of their concentric narrowing. Decreased visual acuity often develops after the onset of headache and progresses; vision deteriorates noticeably during headache attacks and after them. Oculomotor disorders
manifest themselves in the form of transient diplopia with mild paresis of the eye muscles and impaired convergence.
In most patients, these disorders are among the initial manifestations of the disease, and in a quarter of them they serve as one of the main complaints with vertebrobasilar insufficiency. Static and dynamic ataxia are also among the permanent symptoms that are manifested by patient complaints of instability and staggering when walking and standing. Coordination of movements is significantly less impaired; a persistent change occurs, as a rule, with cerebellar infarctions. Vestibular disorders
manifest themselves in the form of sudden dizziness - systemic, which is characterized by a feeling of “rotation of objects”, “an inverted room”, and non-systemic with a feeling of “motion sickness”, nausea, and less often vomiting.
Spontaneous nystagmus is also detected, sometimes only after special tests with turning the head to the side and fixing it in these positions (De Klein test). The development of dizziness is associated with ischemia of either the vestibulocochlear organ or the vestibular nuclei and their connections. The vestibular nuclei are most sensitive to ischemia and hypoxia. In this case, dizziness as a monosymptom can be regarded as a sign of impaired blood flow in the arteries of the vertebrobasilar system only in combination with other signs of its impairment in patients with a relatively persistent otoneurological symptom complex. Less known, although not uncommon, are optic-vestibular disorders. These include symptoms of “shading shadow” and “convergent vertigo,” in which patients experience dizziness or unsteadiness when flashing light and shadow or when looking downward. Characteristic symptoms are attacks of sudden falling
without loss of consciousness (“drop attacks”), usually occurring during sudden turns or throwing back the head.
Syncopal vertebral Unterharnscheidt syndrome has been described, in which loss of consciousness and muscle hypotonia are observed in the absence of evidence of epilepsy and other paroxysmal conditions. Manifestations of diencephalic
disorders include severe general weakness, irresistible drowsiness, disturbances in the rhythm of sleep and wakefulness, as well as various autonomic-visceral disorders, a sudden increase in blood pressure (BP), and heart rhythm disturbances.
These disorders are associated with ischemia of the structures of the reticular formation of the brain stem. The described symptom complex has now been supplemented by other signs, which, in combination with them, also make it possible to judge the insufficiency of blood flow in the arteries of the vertebrobasilar system. At various stages of vertebrobasilar insufficiency, patients often complain of decreased memory
(“forgetfulness”), concentration disorders and instability of active attention. Most often, memory for names, numbers, and recently occurring events decreases. The ability to memorize new material decreases, it becomes more difficult to retain what has been read in memory, what is planned for implementation is forgotten, and the need to write it down arises. It becomes difficult for patients to comprehend a large amount of information, which leads to a certain decrease in performance and limitation of creative possibilities in people engaged in mental work. At the same time, professional memory and memory of past events are preserved. This applies more to RAM than to logical memory. Often, a decrease in memory and performance is regarded by others as a result of overwork, and not as a manifestation of cerebral vascular insufficiency. During neuropsychological research, the preservation of the level of generalization, the correspondence of judgments to the general educational and cultural level, and the preservation of the stock of ideas and skills are noted. Impaired cognitive functions significantly reduce the quality of life and also affect the progression of cerebrovascular insufficiency. Decreased memory for current events in patients with vertebrobasilar insufficiency is associated with chronic ischemia of the medial parts of the temporal lobes, primarily the hippocampus and mammillary bodies. With vertebrobasilar insufficiency, attacks of transient global ischemia are also observed, during which working memory (the ability to remember new information) is impaired for several hours. The patient looks absent-minded, he is disoriented in space and time, sometimes excited, persistently tries to find out from those around him where he is, how he got here, but being unable to remember the answers, he constantly asks the same questions. With the return of the ability to remember, orientation is also restored, only the episode itself is amnesic. Acute amnesia can also be caused by acute cerebrovascular accident in the basins of both posterior cerebral arteries. In this case, amnesia may be accompanied by limitation of visual fields (unilateral or bilateral hemianopia), visual agnosia, alexia, amnestic aphasia, and sensory impairment. The combination of a number of characteristic symptoms makes it possible to diagnose the syndrome of blood flow insufficiency in the arteries of the vertebrobasilar system, although in this case only the ischemic nature of the cerebrovascular accident and the localization of the source of ischemia are determined, and not the reasons that determined this nature.
Objective data
The most accessible and safest methods for determining insufficiency of blood flow in the arteries of the vertebrobasilar system are neurological examination and ultrasound methods of studying the vascular system of the brain.
Among the objective signs revealed during a neurological examination
, one should first of all mention nystagmus, static and dynamic ataxia.
In the Romberg test, the patient deviates to the side. Walking with eyes closed reveals unsteadiness and persistent deviation to one side in a patient with insufficient blood flow in the vertebrobasilar system. When performing the Unterberger test, the patient is asked to march in one place with his eyes closed for 1–3 minutes. Normally, it remains in place or moves slightly relative to the starting point or rotates slightly around its axis. A forward shift of more than 1 m and a rotation of more than 40–60° (after 50 steps in place) are considered pathological. The results of the Babinski-Weil test (“star test”) are interpreted in a similar way. With eyes closed, the patient is asked to take two steps forward, turn 180° and take two steps back. Any deviations to the side or rotation indicate dysfunction of the vestibular labyrinth. If the patient is asked to walk in the forward and reverse directions several times, then as a result of a deviation to one side, the trajectory of his movement resembles the outline of a star (hence the name of the test). It is also necessary to measure blood pressure in both arms in a sitting and lying position. Objective signs of the syndrome include differences in pulse and blood pressure in the arms and noise in the supraclavicular region. With a significant decrease in systolic blood pressure (more than 20 mm Hg) in an upright position, symptoms reminiscent of insufficiency of blood flow in the vertebrobasilar system should be attributed to orthostatic hypotension. Subclavian “steal syndrome” is characterized by a phenomenon when a patient, against the background of intense hand work, develops brainstem symptoms—usually dizziness. Doppler ultrasound
allows you to obtain data on blood flow in the vertebral arteries, linear speed and direction of blood flow in them.
Compression-functional tests make it possible to assess the condition and resources of collateral circulation, blood flow in the carotid, temporal, supratrochlear and other arteries. Duplex scanning allows you to determine the condition of the artery wall, the structure and surface of atherosclerotic plaques that stenose these arteries. Transcranial Doppler ultrasound with pharmacological tests is important for determining cerebral hemodynamic reserve. Data on the condition of the great arteries of the head (MAG) and intracerebral arteries obtained from CT and MRI angiography are extremely informative. X-rays
of the cervical spine can provide information about the condition of the structures around the vertebral arteries and the effect of these structures on the vertebral arteries and the blood flow in them;
functional tests are used in this case. A special place among instrumental methods is occupied by otoneurological research
, especially if it is supported by electronystagmographic and electrophysiological data on auditory evoked potentials characterizing the state of brain stem structures, as well as MRI of these structures. The algorithm for using the listed instrumental research methods is determined by the logic of constructing a clinical diagnosis.
Treatment of vertebrobasilar insufficiency
Treatment of vertebrobasilar insufficiency is aimed at preventing its progression, improving blood supply to the brain, and correcting individual syndromes and symptoms.
The most effective measures in this direction are the elimination or correction of the main risk factors
for the development of vertebrobasilar insufficiency, which include smoking, hyperlipidemia, AS of the cerebral arteries, hypertension, diabetes mellitus, obesity, heart disease, disorders of the rheological properties of the blood, psycho-emotional stress, alcohol abuse [3 ].
A large place in the prevention of the progression of vertebrobasilar insufficiency is occupied by recreational activities, climate therapy at local resorts, in low-altitude conditions, at sea resorts, balneotherapy (radon, brine, carbon dioxide, sulfide, iodine-bromine baths). Moderate physical activity (therapeutic exercises, walking, swimming) and regular mental exercise are needed. The diet
should not be burdensome for the patient (do not overeat, limit the consumption of animal fats, easily digestible carbohydrates and foods rich in cholesterol, reduce the total calorie content of food, introduce fresh vegetables and fruits, wholemeal products, fish products into the diet).
Smoking is excluded and alcohol consumption is limited. When treating vertebrobasilar insufficiency, the following measures should be taken: early detection; determination of the severity of clinical symptoms; exclusion or correction of the main risk factors for the development of cardiovascular diseases; dynamic observation; timely initiation of treatment; its duration and continuity; treatment of concomitant somatic, neurological and mental disorders; medical, professional and social rehabilitation. Methods of drug treatment
of chronic musculoskeletal disorders include: antihypertensive therapy, the use of lipid-lowering drugs, improving blood supply to the brain using antithrombotic drugs, neuroprotective therapy [3, 4].
One of the most promising neuroprotective drugs from the perspective of evidence-based medicine is citicoline
[4, 5].
Citicoline, a natural endogenous compound also known as cytidine-5'-diphosphocholine (CDP-choline), is a mononucleotide consisting of ribose, cytosine, pyrophosphate and choline. When taken orally, citicoline is rapidly absorbed and hydrolyzed into choline and cytidine in the intestinal wall and liver. These substances enter the systemic circulation, pass through the blood-brain barrier and recombine to form citicoline within the central nervous system [6]. Phosphatidylcholine in brain cell membranes is broken down into fatty acids and free radicals by phospholipases under ischemic conditions. By restoring the activity of Na+/K+-ATPase of the cell membrane, reducing the activity of phospholipase A2 and participating in the synthesis of phosphatidylcholine, the membrane-stabilizing effect of citicoline is realized. In addition, citicoline affects the formation of free fatty acids, the synthesis of acetylcholine and an increase in the content of norepinephrine and dopamine in nervous tissue. Citicoline is also able to inhibit glutamate-induced apoptosis and enhance neuroplasticity mechanisms [7]. The first studies of citicoline, conducted at the end of the twentieth century, concerned patients with vascular dementia. Thus, R. Lozano et al. (1986) observed 2067 elderly patients treated in geriatric psychiatry departments and found a positive effect of a 2-month course of citicoline therapy on the severity of neuropsychological symptoms [8]. In a study by B. Chandra (1992), assessing the effectiveness of the drug in 146 patients with vascular dementia, it was demonstrated that therapy with citicoline at a dose of 750 mg/day IV for 2 months. led to a significant improvement in cognitive function scores (assessed on the MMSE scale) compared to placebo. Moreover, the effect of therapy was maintained after 10 months. after completion of treatment [9]. In 2005, a Cochrane review of the effectiveness of citicoline in the treatment of cognitive and behavioral impairment due to chronic cerebrovascular insufficiency in elderly patients was published [10]. The review included the results of 14 randomized placebo-controlled trials involving 1336 patients. The average dose of citicoline in these studies was 1000 mg/day, the duration of treatment was 3 months. The effectiveness of treatment was assessed using tests for memory, attention, and behavior. The review demonstrated the positive effect of citicoline on behavioral disorders, as well as improving memory. The only significant limitation of this review was the short duration of the included clinical studies. In subsequent years, researchers focused on studying the drug's effectiveness in patients with mild cognitive impairment (MCI) and post-stroke cognitive impairment. Thus, according to M. V. Putilina (2009), already at the initial stages of manifestations of cognitive impairment in patients with chronic cerebrovascular insufficiency, the use of citicoline (at a dosage of 1000 mg IM or IV for 10 days followed by oral administration in the form of a solution for oral administration for 3 months) contributes to the regression of these disorders. In addition, the drug has a positive effect on concomitant emotional, affective and behavioral disorders in this group of patients [11]. In 2013, the results of two controlled studies evaluating the effect of the drug on cognitive function in patients with chronic cerebrovascular diseases were published. In a placebo-controlled study, L. Alvarez-Sabin et al. (2013) took part in 347 elderly patients (mean age 67.2±11.3 years) who had suffered a stroke and had cognitive impairment. In the active treatment group (172 patients), citicoline was prescribed at a dose of 2000 mg/day per os for 6 months, then 1000 mg/day for another 6 months. The criteria for the effectiveness of treatment were the results of a neuropsychological examination (a battery of tests for memory, attention, executive (regulatory) functions, time orientation), as well as an assessment of clinical outcomes using the modified Rankin Scale after 6 and 12 months. after starting treatment. Long-term therapy with citicoline resulted in a slowdown in the progression of cognitive impairment and better functional recovery (compared to placebo) due to improved attention, regulatory functions, and time orientation [12]. The IDEALE study assessed the effectiveness of citicoline in the long-term treatment of vascular MCI in elderly patients. 349 patients with MCI of predominantly vascular origin were prescribed citicoline (265 patients) at a dose of 1000 mg/day per os for 9 months. or placebo (84 patients). Treatment with citicoline had no effect on measures of functional daily activities compared with placebo. At the same time, during treatment with citicoline, there was a positive dynamics of cognitive functions when assessed on the MMSE scale (improvement after 9 months by an average of 0.5 points); in the placebo group, progression of cognitive impairment was observed (after 9 months - worsening by an average of 1.9 points) (p=0.0001). Thus, long-term therapy with citicoline is associated with a decrease in the rate of progression of cognitive impairment in patients with vascular MCI [13]. Recently, new generic dosage forms have been widely introduced into practice. Among them is the domestic drug Neypilept
. The drug is produced from the Japanese substance of the KYOWA company in the form of a solution of 125 and 250 mg/ml for IV and IM administration, as well as two oral forms - an oral solution of 100 mg/ml in bottles of 30 ml and 100 ml. The volume of the 100 ml bottle corresponds to the sachet form of the original drug. As part of post-registration multicenter randomized studies, Neypilept was compared with the original drug in 152 patients in the acute period of ischemic stroke in the carotid system (RCT No. 396 of June 24, 2013) [14] and the effectiveness and safety of its oral form was studied in 128 patients with cognitive impairment (RCT No. 145 dated March 26, 2015) [15]. The results of the studies demonstrated the tolerability and effectiveness of Neypilept in these conditions comparable to the original drug [16, 17].
Conclusion
It should be emphasized that timely and systematic treatment can prevent the progression of cerebrovascular insufficiency and significantly improve the quality of life of patients. The adequacy and effectiveness of taking citicoline (Neipilept) is of particular importance. Adequacy of therapy implies a course of taking the drug, as well as cooperation between the patient and the attending physician in prescribing and carrying out treatment, the goals of which are to preserve the ability to work and maintain the patient’s quality of life. The following areas for assessing the effectiveness of treatment for vertebrobasilar insufficiency can be recommended (as early as 6–12 months from the start of treatment): reduction or disappearance of cerebral complaints, improvement of cognitive functions (primarily memory).
The original article was published on the RMJ website (Russian Medical Journal): https://www.rmj.ru/articles/nevrologiya/Sindrom_nedostatochnosti_krovotoka_varteriyah_vertebrobazilyarnoy_sistemy/#ixzz5NyXkC9vV
Appointment form...
Treatment of ischemic stroke in the posterior cerebral artery territory
Cerebral infarctions in the posterior cerebral artery basin are usually secondary and develop against the background of embolism from the underlying segments of the vertebrobasilar system or from the heart cavity. In order to prevent repeated embolisms of the arterial lumen, anticoagulants (heparin) are prescribed. For atherosclerotic occlusion of the posterior cerebral artery, specific treatment is not required. Symptoms of a transient ischemic attack of the brain in the basin of the posterior cerebral artery can be caused by atherothrombotic stenosis of its proximal (underlying) section or one of its penetrating branches (lacunar TIA).
The course of such atherosclerotic lesions of the posterior cerebral artery remains unspecified. Therefore, there are no clear comparative data on the effectiveness of anticoagulants and antiplatelet agents or the prescription of one or another therapy in comparison with its absence. In general, the mildest way to treat ischemia or ischemic stroke in the posterior cerebral artery is to prescribe antiplatelet agents (aspirin, trental).
Ischemic stroke (cerebral infarction) - symptoms and treatment
General events
When treating ischemic stroke, it is customary not to reduce blood pressure quickly if it is high, especially in the first days of the disease.
Low blood pressure should be increased - this is done by doctors; do not give the patient any medications on your own. Uncontrollable, severe vomiting is a common problem in the period immediately after a stroke, especially when the basilar artery is affected. This creates problems in the patient's nutrition. If vomiting does not stop, or there is dysphagia, then a feeding tube is inserted. The lack of electrolytes is compensated for by infusion therapy. The airway should be closely monitored.
Thrombolytic therapy
Thrombolytic therapy is the only therapy for acute ischemic stroke whose effectiveness has been proven in large studies.
No more than 4.5 hours should pass from the onset of the first symptoms of a stroke to the administration of a thrombolytic, so prompt hospitalization is important.
Vascular occlusion occurs in the arterial or venous bed. Thrombotic medications dissolve the clot, but the drug must be delivered to the thrombotic area.
Thrombolytic agents first appeared in the 1940s. The active development of drugs in this group has led to the fact that there are currently five generations of thrombolytics:
- The first thrombolytics are natural substances that convert plasmagen into plasmin, thereby causing active bleeding. These ingredients are isolated from the blood. This group of drugs is rarely used, as severe bleeding is possible. This generation includes: Fibrinolysin, Streptokinase, Urokinase, Streptodecase, Thromboflux.
- The second generation are substances obtained based on the achievements of genetic engineering using bacteria. This generation of drugs has been well studied and has virtually no side effects. Act directly on blood clots. This generation includes: Alteplase, Actilyse, Prourokinase, Gemaz. Purolase, Metalise.
- Third generation - these drugs are able to quickly find a blood clot and act on it for a longer period of time. Most effective in the first three hours: Reteplase, Tenecteplase, Lanoteplase, Antistreplase, Antistreptolase.
- Fourth generation - these drugs are in development and are characterized by a rapid and intense effect on the blood clot. Insufficiently studied.
- The fifth generation is a combination of natural and recombinant active substances.
In the recovery phase, when the patient’s condition almost always improves to one degree or another, speech therapy assistance, as well as occupational therapy and exercise therapy, are important.
Infusion therapy
Anticoagulants (heparin and indirect anticoagulants) are prescribed only when the doctor’s instructions will be followed and it is possible to monitor blood clotting [8].
Anticoagulants
Anticoagulants prevent the formation of fibrin threads and thrombus formation, help stop the growth of already formed blood clots, as well as the effect of endogenous fibrinolytic enzymes on blood clots [11].
Anticoagulant treatment can be started only after intracerebral bleeding has been ruled out.
Direct coagulants : heparin and its derivatives, direct thrombin inhibitors, as well as selective inhibitors of factor X (Stewart-Prower Factor - one of the blood clotting factors).
Indirect anticoagulants:
- Vitamin K antagonists: phenindione (Phenilin), warfarin (Warfarex), acenocoumarol (Sincumar);
- Heparin and its derivatives: heparin, antithrombin III, dalteparin (Fragmin), enoxaparin (Anfibra, hemapaxan, Clexane, Enixum), nadroparin (Fraxiparin), parnaparin (Fluxum), sulodexide (Angioflux, Vessel Due F), bemiparin (Cibor);
- Direct thrombin inhibitors: bivalirudin (Angiox), dabigatran etexilate (Pradaxa);
- Selective factor X inhibitors: apixaban (Eliquis), fondaparinux (Arixtra), rivaroxaban (Xarelto).
Antiplatelet agents
The administration of antiplatelet agents improves the passage of fluid in the brain tissue and prevents the development of acute disruption of the blood supply to the brain [6].
Antiplatelet agents prevent platelets from sticking together, thereby preventing the formation of blood clots.
Classification of antiplatelet agents by mechanism of action:
- aspirin, indobufen, trifluse (stop the action of cyclooxygenase-1, COX-1);
- ticlopidine, clopidogrel, prasugrel, ticagrelor, cangrelor (stop the functioning of the ADP receptor P2Y12 on platelet membranes);
- abciximab, monofram, eptifibatide, tirofiban; xymelofiban, orbofiban, sibrafiban, lotrafiban and others (glycoprotein (GP) Iib/IIIa antagonists);
- dipyridamole and triflusal (cAMP phosphodiesterase inhibitors);
- iloprost (adenylate cyclase enhancer);
- ifetroban, sulotroban and others (suppress the TXA2/PGH2 receptor);
- atopaxar, vorapaxar (antagonize the AR receptor (protease activated receptors) of thrombin).
Aspirin is a commonly used drug in this group. If anticoagulants are contraindicated, then antiplatelet agents can be used.
Surgery
Carotid endarterectomy is a prophylactic surgical procedure performed to remove atherosclerotic plaque from the arteria carotis communis (common carotid artery).
When a cerebellar stroke develops with compression of the brain stem, in order to save the patient’s life, a surgical operation is performed to relieve intracranial pressure in the posterior cranial fossa.
Decongestant therapy
There are different and quite opposite opinions regarding the use of corticosteroids for ischemic stroke, but doctors still actively use them to reduce cerebral edema: they prescribe dexamethasone 10 mg intravenously or intramuscularly, then 4 mg intravenously or intramuscularly every 4-6 hours.
Osmotic agents . Mannitol - increases plasma osmolarity, thereby fluid from tissues, including from the brain, moves into the bloodstream, creating a pronounced diuretic effect, and a large amount of fluid is removed from the body. Cancellation can have a rebound effect.
Anticonvulsants
They must be prescribed for the development of ischemic stroke with epileptic seizures.
Rehabilitation after stroke
Rehabilitation measures begin in the early period of the disease and continue after discharge from the hospital. They include not only drug treatment, massage, physical therapy, speech therapy classes, but also require the involvement of other specialists in psychological, social and labor rehabilitation.
Along with the restoration of impaired functions, rehabilitation includes:
- prevention of post-stroke complications;
- prevention of recurrent strokes.
Basic principles of rehabilitation after stroke:
- early start of rehabilitation measures;
- systematicity and duration, which is possible with a well-organized step-by-step construction of rehabilitation;
- inclusion of specialists of various profiles in the rehabilitation process, individualization of rehabilitation programs;
- active participation in the rehabilitation process of the patient himself, his relatives and friends.
The duration of rehabilitation is determined by the timing of restoration of impaired functions. Recovery of motor functions occurs mainly in the first 6 months after a stroke. During this period, intensive motor rehabilitation is most effective. Rehabilitation treatment for patients with aphasia should be longer and carried out during the first 2-3 years after a stroke.
The complexity of rehabilitation consists of using not one, but several methods aimed at overcoming the defect.
For movement disorders, the rehabilitation complex includes:
- methods of kinesiotherapy (passive and active gymnastics, training in walking and self-care skills);
- correction of motor dysfunction using biofeedback and electrical stimulation using feedback;
- methods of overcoming spasticity and treatment of arthropathy.
For speech disorders, the main thing is regular classes with a specialist in the restoration of speech, reading and writing (speech therapist-aphasiologist or neuropsychologist).
The following model of staged rehabilitation after a stroke is most optimal:
Stage 1 - rehabilitation begins in the angioneurological department (or in the regular neurological department of a clinical hospital), where the patient is delivered by ambulance;
Stage 2 - at the end of the acute period (the first 3-4 weeks), the following options for referring patients are possible:
- 1st option - the patient with complete restoration of impaired functions is discharged for outpatient follow-up treatment or transferred to a sanatorium;
- 2nd option - a patient with a pronounced motor deficit, who by the end of the acute period is still unable to move independently or moves with great difficulty, and needs outside help with self-care, is transferred to the rehabilitation department of the hospital where he was taken by ambulance;
- Option 3 - patients with moderate and mild motor defects, who can move independently within the hospital and provide basic self-care, are transferred to a rehabilitation center. Patients who, during their stay in the rehabilitation department of the hospital (2nd option) have learned to walk independently and simply take care of themselves in everyday life, are also transferred to the rehabilitation center.
Stage 3 - outpatient rehabilitation: rehabilitation in special rehabilitation sanatoriums and at home.
Outpatient rehabilitation is carried out on the basis of rehabilitation departments of clinics or recovery rooms or in the form of a “day hospital” at rehabilitation departments of hospitals and rehabilitation centers. In rehabilitation sanatoriums there can be patients who can fully care for themselves and move independently not only indoors, but also outside. For those patients who cannot independently get to a clinic or day hospital, rehabilitation assistance (classes with a physical therapy methodologist and classes on speech restoration) is provided at home, with the obligatory training of relatives.
Contraindications and limitations to active rehabilitation
The following concomitant diseases limit or prevent active motor rehabilitation:
- frequent attacks of angina pectoris;
- heart failure;
- high and poorly controlled blood pressure;
- chronic pulmonary diseases: bronchial asthma with frequent attacks, obstructive bronchitis;
- severe forms of diabetes mellitus;
- cancer;
- acute inflammatory diseases;
- some diseases and pathologies of the musculoskeletal system: severe arthritis and arthrosis, amputated limbs.
Psychoses and severe cognitive impairment (dementia) are limitations for carrying out not only motor, but also speech rehabilitation.
There are limitations for rehabilitation treatment in conventional rehabilitation centers: extremely limited mobility of patients (lack of independent movement and self-care), impaired control of the functions of the pelvic organs, and impaired swallowing. Rehabilitation of such patients, as well as patients with severe cardiac and pulmonary pathologies, is carried out in rehabilitation departments located on the basis of large clinical multidisciplinary hospitals, according to special rehabilitation programs.