Diagnosis of head injury due to concussion and contusion
As before, at the initial stage of diagnosis for traumatic brain injury, the first diagnostic method is radiography of the skull bones.
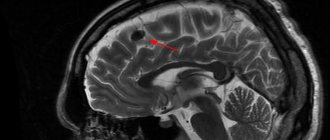
To study the location and extent of damage to brain tissue, MRI of the brain is best. In case of a concussion, the patient does not need to undergo a diagnostic MRI procedure of the brain. Carrying out a lumbar puncture (LP) for diagnostic purposes makes it possible to most accurately, compared with other methods, recognize subarachnoid hemorrhage and the degree of its severity, identify reactions of the meninges to TBI, and detect inflammatory complications of TBI and spinal injuries.
X-ray of the skull bones in case of a concussion or bruise of the brain.
The most typical signs and symptoms of traumatic brain injury occurring in the acute period after injury (a blow to the head, a fall, a car accident, etc.):
- scalp damage
- abrasions and swelling
- skull fracture
- nosebleeds and nasal discharge
- neck muscles are tense
- loss of consciousness
Signs and symptoms of traumatic brain injury (concussion, brain contusion).
Based on the results of a neurological examination, a diagnosis can already be made. If the diagnosis is preliminary and requires clarification, the patient will be given additional instrumental or laboratory diagnostic appointments.
Possible additional instrumental or laboratory diagnostic appointments to clarify the diagnosis of traumatic brain injury:
- REG, USDG of neck and brain vessels, EchoEG
- X-ray of the skull bones, cervical spine with functional tests
- MRI of the brain
- MRI angiography of cerebral vessels
- MRI of the cervical spine, etc.
- Lumbar puncture (LP) to analyze the composition of cerebrospinal fluid (CSF)
Magnetic resonance imaging of the brain (MRI) is performed when diagnosing a patient with a traumatic brain injury (bruise, compression of the brain, etc.).
Doctors' advice
Basic first aid for closed head injury is universal, but diagnosis and further treatment must be entrusted to professionals. The specialist, independently or using special approaches, will determine exactly whether you are dealing with a concussion or bruise and will draw up a suitable treatment regimen. Only in this case will the victim’s recovery be as fast as possible, and the negative consequences after the injury will be minimal.
Knowing the signs, symptoms, and distinctive features of a bruise and concussion, you can independently understand the situation. In any case, the actions of the victim, his relatives or eyewitnesses must be the same - it is necessary to urgently call an ambulance so that professionals can take care of the patient.
Glasgow Coma Scale (GCS)
When assessing the severity of a patient’s brain injury, specialists take into account the level of neurological deficit (loss of function) and the level of clarity of consciousness. For ease of assessment in clinical practice, all these indicators (focal neurological symptoms, level of consciousness) were compiled into a Glasgow Coma Scale (GCS) by neurosurgeons from the University of Glasgow in 1974 (Professors Graham Teasdale and Bryan J. Jennett).
Glasgow Coma Scale (GCS) for traumatic brain injury:
Index | Responsiveness | Point |
Movement (D) | Performing spontaneous movements on command | 6 |
| Purposeful pushing away in response to pain | 5 | |
| Withdrawal of a limb in response to pain | 4 | |
| Pathological flexion in response to pain (decortication) | 3 | |
| Abnormal extension in response to pain (decerebration) | 2 | |
| No motor response | 1 | |
Speech (R) | Orientation in space and time | 5 |
| Confused speech, disorientation | 4 | |
| Says incomprehensible words | 3 | |
| Makes strange sounds | 2 | |
| No voice response | 1 | |
Eye opening (D) | Spontaneous | 4 |
| To the command, addressed speech | 3 | |
| To the pain | 2 | |
| Doesn't open his eyes | 1 | |
General value | 3-15 |
Note: Coma points = D + R + G. Patients scoring 3 or 4 on the Glasgow Coma Scale have an 85% chance of dying or entering a residual vegetative state. Patients who score more than 11 on the Glasgow Coma Scale have only a 5–10% chance of death or a residual vegetative state and an 85% chance of moderate disability or full recovery. Mean Glasgow Coma Scale scores correlate with the proportional odds of recovery.
The classification of traumatic brain injury is based on many factors. An alternative traumatic brain injury severity scale.
| Severity | Structural changes (MRI, ) | Loss of consciousness | Confusion | Post-traumatic (retrograde) amnesia | Glasgow Coma Scale (GCS), points |
| Light | Norm | 0–30 min (<20 min – 1 h) | Time of injury <24 h | <24 h | 13–15 |
| Average | Norm or pathology | >30 min but <24 h | >24 h | 1–7 days | 9–12 |
| Heavy | Norm or pathology | >24 h | >24 h | >7 days | 3–8 |
Pathophysiological changes and intensive care in traumatic brain injury
- Autoregulation of cerebral blood flow is one of the most important systems for maintaining the balance of intracerebral pressure. Small vessels of the brain respond to hydrostatic pressure and regulate their tone to maintain constant cerebral blood flow within the range of mean arterial pressure from 60 to 160 mm Hg. Art. Once the pressure regulation curve shifts to the right in severe brain injury, random changes in systemic blood pressure can lead to severe and linear changes in cerebral blood flow that lead to pathological and irreversible conditions such as cerebral hypoperfusion (cerebral ischemia) or hyperperfusion (cerebral hyperemia).
- Changes in cerebral blood flow volume and systemic blood pressure lead to dilation (vasodilation) or narrowing (vasoconstriction) of cerebral vessels. Cerebral vasodilation (dilation of the lumen of blood vessels) can lead to a decrease in systemic blood pressure. This causes an increase in cerebral blood volume and a rise in intracranial pressure. This vascular response can also be initiated by hypoxemia, dehydration, or hypocapnia (due to hyperventilation therapy).
- A decrease in cerebral perfusion pressure causes vasodilation (dilation) of cerebral vessels and a subsequent increase in cerebral blood volume. A decrease in cerebral perfusion pressure is often associated with a decrease in systemic blood pressure. By exceeding the capacity of autoregulation, hyperperfusion may increase the risk of brain congestion. Conversely, when systemic blood pressure falls below the limit of the body’s ability to correct it, a decrease in cerebral perfusion pressure and the occurrence of cerebral ischemia are possible.
- Excessive hyperventilation causes vasoconstriction (vasoconstriction) and decreased cerebral blood flow, leading to cerebral ischemia. As a result of cerebrovascular sensitivity to blood CO2 levels, dilatation (widening) of blood vessels in the brain caused by increased partial pressure of carbon dioxide (PaCO2) can increase intracranial pressure and contribute to an increase in blood volume in the brain (cerebral edema). If this occurs, the outcome for patients with severe traumatic brain injury may be poor. On the other hand, when the partial pressure of carbon dioxide (PaCO2) in the blood falls, the blood vessels in the brain constrict (vasoconstriction), leading to a decrease in blood volume and ultimately a decrease in intracranial pressure.
- An increase in endogenous catecholamines (sympathetic system-induced catecholamine release) causes peripheral vasoconstriction (vasoconstriction), which increases systemic blood pressure (neurogenic hypertension) after traumatic brain injury. As a result, systemic blood pressure will be maintained despite the presence of hypovolemia. Mannitol, as an osmotic diuretic, has historically been used in patients with increased intracranial pressure. When used off-label, however, mannitol causes excessive intravascular dehydration (dehydration). As a result of dehydration and hemodynamic disturbances, an unstable state of cerebral blood flow is formed with episodes of sudden hypotension. To prevent sudden catastrophic drops in blood pressure (hypotension) after traumatic brain injury (TBI), routine use of mannitol and intravascular dehydration should be avoided.
- Hyperglycemia also often develops after severe brain injury or a similar stressful event. High blood glucose levels after traumatic brain injury (TBI) appear to be associated with higher severity of brain injury and poorer neurological patient outcome. Until now, little is known about the role of blood glucose in the formation of secondary mechanisms of neuronal damage after brain injury. The best time to initiate glucose-containing fluids for nutritional maintenance is also questionable, as acute hyperglycemia (increased blood glucose levels) can alter the patient's neurological outcome. It remains to be seen whether hyperglycemia alone is capable of causing inflammation of brain tissue in acute critical conditions involving the accumulation of neutrophils.
Treatment of head injury due to concussion and contusion
Depending on the severity of the manifestations and causes of the headache symptom, focal disturbances in the neurological status, and the level of consciousness disorder in the patient, with a diagnosis of concussion and brain contusion confirmed by the attending physician, the following therapeutic actions are possible:
- bed rest
- drug therapy (NSAIDs, analgesics, hormones)
- blockades - injections of anesthetics into the attachment points of the posterior cervical muscles
- lumbar puncture
- manual therapy
- physiotherapy (UHF, SMT, etc.)
- physiotherapy
- acupuncture
- surgical treatment
Lumbar puncture (LP) is performed to measure cerebrospinal fluid pressure, study the patency of the subarachnoid space of the spinal cord, and determine the color, transparency and composition of the cerebrospinal fluid.
Lumbar puncture is used for accelerated sanitation of cerebrospinal fluid and restoration of cerebrospinal fluid flow, including after surgery. In such cases, in the absence of contraindications, up to 10-20 ml of cerebrospinal fluid or more are removed.
Attention! If you have complaints of long-term or chronic, as well as acute headache, you should contact a neurologist or neurosurgeon for advice first. A very common mistake is made by relatives of a patient with traumatic brain injury (TBI), when self-diagnosis begins with tomography, ultrasound, EEG, etc. At the same time, there is no hint of an attempt to consult a neurotrauma specialist in person.
With head injuries, a person, especially a child, receives various bruises and abrasions. But if the bruise is too severe, it can also lead to a concussion. How to distinguish a regular bruise from a concussion?
Nature has safely hidden our brain in the skull, where it is protected by bones and intracranial fluid, which absorbs shock. If the bruise is too severe, the brain may shift relative to its normal position and hit the skull from the inside. Does this almost always result in a concussion?
Signs of a concussion:
- severe dizziness after a blow,
- noise in ears,
- weakness and feeling of apathy,
- headache,
- There may be a short-term loss of consciousness.
In addition to these common symptoms, there may also be dangers such as stupefaction or confusion, as well as retrograde amnesia - in this condition, a person forgets events that happened before or during the injury. It has been noticed that the longer the period of “forgotten”, the more severe the condition.
Along with the listed symptoms, respiratory and cardiac problems may also occur, which is manifested by an uneven pulse and rapid breathing. Such symptoms indicate damage to the medulla oblongata, which is responsible for the basic functions of the body - breathing and heart rate.
If a person has suffered a severe head injury and is experiencing any of the symptoms mentioned, he should be seen by a doctor. Since the brain is a very delicate organ, disruption of its functioning can affect the entire body, and only a doctor can make the correct diagnosis and prescribe the optimal treatment
.
An encephalogram, computed tomography, and MRI are used to diagnose a concussion.
If the doctor has diagnosed a concussion, the patient is prescribed strict bed rest for 1-2 weeks and medications that stimulate cerebral circulation.
First aid for concussion
— Apply ice or a cloth soaked in cold water to the bruise if there is no blood.
- Rinse the wound with clean water and apply a gauze pad.
— If there is a suspicion of a severe head or spinal injury, the patient should not be moved until the ambulance arrives.
ethnoscience
also offers his own methods for alleviating concussion.
1 tbsp. Pour a spoonful of horsetail into a glass of boiling water, leave and drink ¼ cup 4 times a day.
Pour a glass of boiling water over arnica flowers (1 tablespoon) and leave for 2 hours. Take 2 tbsp. spoons 3 times a day before meals.
St. John's wort (2 tablespoons) pour a glass of water and bring to a boil. Strain the resulting broth and drink 2 glasses a day for a week.