Microangiopathy of the brain is a lesion of the smallest vessels, capillaries localized in cerebral structures. Pathological changes in the walls, narrowing or complete blockage of blood vessels occur.
The disease does not manifest itself as long as the body is able to cope with disturbances in trophism and nutrition of nerve tissue.
In some cases, the approaching catastrophe is not noticeable, which is why the clinical picture is extremely variable. Depends on the individual characteristics of the body and the localization of the process.
As a rule, the pathology affects all capillaries of the brain at once, but not equally. When assessing a person’s condition, individual, largest lesions are detected. This facilitates targeted therapy if surgical treatment is required.
Correction is mainly medicinal. If ineffective, surgery is prescribed.
Development mechanism
There are several provoking factors underlying this. They occur together or separately. It's more a matter of chance. In total there are 4 main ways:
- Consistently high blood pressure levels. A change in the nature of blood flow through the main vessels leads to stenosis (narrowing) of the arteries, a decrease in their elasticity and a reflex violation of capillary tone.
In addition, negative factors that provoke an increase in blood pressure (usually hormonal or toxic, from smoking, drinking alcohol) can also affect small vessels in the same way.
Then the process becomes complex. The entire brain is affected. Such a number of negative factors brings stroke closer every day.
- Inability to regulate vascular tone, changes in their physical properties due to hormonal instability. A textbook example of such a disorder is diabetes mellitus.
If treatment is not carried out, the body simply cannot provide homeostasis (a state of equilibrium). Hence the change in the tone of the capillaries, also arteries, veins.
Severe complications arise over a short period of time. Patients walk along the edge constantly.
- Improper functioning of the immune system. As a result, active synthesis of antigen-antibody complexes develops, followed by the formation of a special protein conglomerate—amyloid.
This substance settles on the walls of blood vessels and provokes degenerative changes over a short period of time. A similar mechanism applies to autoimmune ones. It is considered difficult to correct and dangerous because the prospects are vague.
- It is also possible for mineral salts to be deposited on the walls of the capillaries. Mainly calcium. This is a relatively common mechanism and occurs in children under one year of age. It is diagnosed during the same period.
In the initial stages, symptoms are not noticeable, but as they progress, health deteriorates.
Objectively, the clinical picture is presented by manifestations of nonspecific neurological deficit. Headaches, nausea, spatial disorientation and others are observed that cannot be linked to a specific disease.
Attention:
If you don't take control of the situation, the consequences are dire. Further development of deficiency, stroke, disability or death.
The timing of the negative scenario from beginning to end is different. In most patients, as a result of compensation of the body and adaptation of impaired blood flow, collaterals are formed. That is, parallel, additional networks of capillaries that were not there initially.
If they are sufficiently formed, the violations will not be so noticeable and the “X-hour” will come later. No one can say how much.
Symptoms of focal white matter gliosis
Clinical symptoms are determined by the size, location, and progression of neuroglial accumulations:
- Severe headaches - diffuse type;
- Instability of blood pressure, frequent hypertensive crises;
- Unsteady gait, lack of coordination;
- Decreased mnestic functions;
- Memory impairment.
Therapeutic techniques are ineffective in the presence of diffuse periventricular lesions. Large accumulations in a child are rarely observed, so symptoms do not occur.
What is dangerous about gliosis - prognosis for life and health
Life prognosis depends on the underlying cause of the disease. Clinical symptoms are determined by the severity of white matter damage. Affecting the functional centers of breathing and blood circulation can lead to death. Encephalitis and meningitis are dangerous, which often lead to an unfavorable prognosis and death.
Minor symptoms, favorable outcome for gliosis in the frontal lobes of the brain. Subcortical species are dangerous if they spread diffusely.
Classification
The main method of division is based on the types of pathological process and its origin.
Hypertensive form
As the name suggests, it develops mainly in patients with the same diagnosis. But not always. A symptomatic increase in blood pressure against the background of other diseases gives the same effect.
The longer the violation exists, the higher the tonometer numbers, the more significant the risks.
A latent pathological process is present in most patients, but not the entire array of situations is diagnosed, because doctors are busy assessing the condition of the arteries, and the capillaries are ignored, which is wrong.
Cerebral microangiopathy amyloid type
Associated with the accumulation of this protein substance in the structures of capillaries. Leads to a fairly rapid development of neurological deficit.
It occurs mainly in patients over 60, which is associated with lifestyle and past illnesses. But the deviation does not have gender and age characteristics.
The pathology is autoimmune and requires correction of the functional activity of the body's defenses.
Lenticulostriate type
It is associated with the deposition of calcium salts on the walls of blood vessels, which does not occur normally. The process progresses extremely slowly, which is why symptoms appear late.
The disease is diagnosed mainly in children. According to research, the disorder occurs in every sixth birth. In Russia - the fourth.
This condition is not always considered a disease. There is an opinion that we are talking about a variant of the physiological norm.
If there are no symptoms and the nature of the trophism of nerve tissue is not changed, this is a feature of the body, not a pathology.
Diabetic form
One of the most common. Occurs as a complication of the named endocrine disorder. Diabetic angiopathy is severe and provokes critical disturbances in cerebral blood flow, since the arteries are also affected.
If the correct course of treatment is chosen, the condition is partially controlled, the likelihood of negative consequences is not so high. A complete correction is also possible.
But the effectiveness of the measures and the final result depend on the patient himself, his willingness to follow the specialist’s recommendations and discipline.
There are also classifications according to the course of the pathological process. Thus, angiopathy can be with or without the presence of foci of gliosis (scars, scars). The first option is one and a half to two times less common.
It is possible to subdivide the pathology according to the volume of the lesion. The extensive type is accompanied by the formation of many areas of impaired vascular function.
Attention:
Single lesions give mild symptoms and are much better treated. Because localization is clear, and you can clearly monitor the dynamics of the process.
Typifications are used to describe pathology in documentation and develop treatment methods.
Lesions on MRI of the brain: what does it mean?
The result of magnetic resonance imaging is a series of layer-by-layer images of the area under study. In the images, healthy tissue appears as alternating light and dark areas, depending on the concentration of fluid in it and the pulse sequence used. Based on the sections, the radiologist evaluates:
- development and position of individual structures;
- compliance of the MR signal intensity with the norm;
- condition of the gyri and grooves;
- size and structure of the ventricular system and subarachnoid space;
- parameters of the ear canals, orbits, accessory sinuses;
- structure of the vascular bed;
- structure of cranial nerves and cerebral membranes;
- the presence of signs of pathology (focal changes, swelling, inflammation, damage to the walls of arteries and veins).
Lipoma of the quadrigeminal cistern on MRI (circled)
MRI is prescribed if the patient has neurological abnormalities due to damage to brain tissue. Symptoms may include:
- headache;
- impaired coordination of movements;
- dysfunction of the organs of hearing or vision;
- disturbances in concentration;
- memory disorders;
- sleep problems;
- psychoemotional disorders;
- paresis/paralysis of the limbs and/or facial muscles;
- sensory disorders;
- seizures, etc.
Magnetic resonance imaging of the head allows the doctor to accurately determine the location of focal changes and find out the nature of the patient’s poor health. At the Magnit DC, specialists are armed with the latest MR scanning devices, which allow them to conduct research with high reliability.
Symptoms
The clinical picture at the initial and even advanced stages is blurry. Because microangiopathy does not always lead to severe blood flow disturbances. This takes time.
The body also compensates for the disorder by increasing the amount of nutrition due to the formation of new capillary networks. The so-called collaterals.
They cannot replace functional structures completely, but they are enough.
You also need to take into account the number of lesions, their size, and the type of microangiopathy itself. Individual characteristics of the body. Such an array of factors makes bringing the clinic to a common denominator a difficult task.
The following symptoms occur, with varying intensity and severity and at different times:
- Headache. The strength of discomfort varies. By nature it is pressing, shooting, burning. Located in the frontal and temporal lobes. A different location is possible. The intensity increases after physical activity, stress, and smoking. Consumption of coffee, alcohol, changes in climate zone and when exposed to other negative factors.
The pain is paroxysmal. They go away on their own within a few minutes or hours. The drugs help eliminate discomfort faster.
- Dizziness. Inability to properly navigate in space. Usually low intensity.
- Due to insufficient blood flow, the patient becomes more sensitive to aggressive environmental factors. Changes in weather, vegetative-vascular crises, surges in blood pressure against the background of a new temperature regime, for example, when moving to another region or climate zone. Women have a much more difficult time with premenstrual syndrome, etc.
- Nausea. Rarely vomiting. Single episodes and not always.
- There is also an inability to control one’s own body normally. Weakness in the limbs, clumsiness, unsteadiness of gait, muscle discomfort, feeling of leaden heaviness. All these are parts of one whole.
- Asthenic phenomena. A person constantly feels tired. Weakness, fatigue, drowsiness, regardless of the time of day. All these are signs of insufficient trophism of cerebral tissues. The brain goes into an “economy” mode and does not spend energy as actively.
- Behavioral disorders. Aggressiveness, tearfulness, irritability for no apparent reason.
- Problems with thinking and cognitive sphere. Decreased speed and productivity, absent-mindedness, forgetfulness, attention deficit, inability to concentrate on a subject.
- Focal neurological signs. Disorders of the sensory organs and higher nervous activity. In severe cases, speech disorders are observed, the patient cannot perform arithmetic operations, write, read, etc.
This is not as pronounced as with a stroke, but attracts enough attention. Such signs are possible only with brain damage. What kind of plan - vascular, tumor, toxic or other - needs to be quickly clarified.
In rare cases, fainting and syncope are possible. They indicate a progressive disturbance of cerebral blood flow and indicate the severity of the process. A stroke is likely in the near future.
Symptoms are an unreliable diagnostic criterion. However, they must be taken into account.
Introduction
Cerebral microangiopathy (CMA), or cerebral small vessel disease, can be caused by a group of pathological processes, heterogeneous in etiology, that affect small arteries, arterioles, venules and capillaries of the brain. Cerebral angiopathy associated with age and/or arterial hypertension and age-dependent cerebral amyloid angiopathy are considered the most common sporadic forms of damage to small vessels of the brain. The term “hypertensive angiopathy” is widely used, but is somewhat misleading in that angiopathy is not always necessarily associated with hypertension, but often depends on other vascular risk factors, such as atherosclerosis, diabetes mellitus, age, etc. .
Pathogenetic aspects
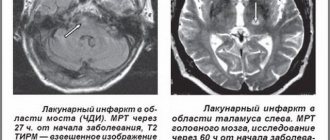
The consequence of microangiopathy is damage to the brain parenchyma, including lacunar infarctions, ischemic lesions of the white matter and intracerebral hemorrhages, located mainly in the structures of the subcortical region. According to modern STRIVE standards, MRI (magnetic resonance imaging) signs of CMA are recent small subcortical infarcts, lacunae, white matter hyperintensity, dilated perivascular spaces, microhemorrhages, and atrophy of the brain substance [1]. Over the past few decades, evidence has accumulated regarding the prevalence, clinical significance, and prognostic value of each of these changes. It is now absolutely clear that these structural changes are associated with clinical manifestations such as stroke, cognitive impairment, mental and movement disorders, disability and even mortality. In general, they are considered as markers of a negative prognosis [1, 2]. The mechanisms associated with vascular damage to the brain parenchyma are heterogeneous and not fully understood. But it is obvious that the initial stage of damage to the vascular wall is a dysfunction of the endothelium. The endothelium is a dynamic organ that acts as a functional and structural barrier between the blood and the vessel wall. Endothelial cells are the main regulator of vascular homeostasis, determining the correct interaction between circulating blood cells and smooth muscle cells of the vascular wall. The endothelium modulates blood flow, controls permeability to plasma components, and influences the adhesion and aggregation of platelets and leukocytes. Endothelial dysfunction is currently considered as one of the core mechanisms of structural and functional changes in cerebral vessels in CMA [1]. A fundamental sign of endothelial dysfunction is impaired bioavailability of nitric oxide (NO) and, accordingly, a decrease in vascular dilatation to endothelial stimuli.
The main consequence of impaired endothelium-dependent vasodilation is an increase in peripheral resistance. Arterial stiffness contributes to an increase in pulse pressure, and this is a hemodynamic stressor for the brain, since the latter has low resistance to pulse shock flow. Shock pressure primarily damages small-caliber cerebral vessels. Impaired functioning of penetrating arteries and arterioles leads to disruption of the mechanisms of autoregulation of cerebral circulation and disruption of the integrity of the blood-brain barrier [3]. An increase in the permeability of the blood-brain barrier is accompanied by extravasation of plasma components both directly into the arterial wall (which contributes to its thickening and disintegration) and into adjacent areas of the brain with the development of perivascular edema (which may be one of the mechanisms of white matter damage), as well as processes of aseptic inflammation. Additionally, vasoconstriction itself leads to local immunological inflammatory reactions, platelet aggregation, and blood clot formation. These processes culminate in histopathological disorders of the distal vessels, such as arteriosclerosis, lipohyalinosis, fibrinoid necrosis and microaneurysms, which can coexist in various combinations. These changes are an important stage that precedes damage to brain tissue. Prolongation of these processes entails disruption of the functioning of the membranes of nerve cells and their axons. Neuronal membranes are characterized by high metabolism due to the enzymatic activity of the enzyme complexes built into them, which ensure the functioning of the receptors. A decrease in the metabolism of membrane phospholipids under conditions of deteriorating perfusion is a key moment for the formation of “vicious circles” and the development of a whole cascade of pathophysiological reactions, primarily excitotoxic, and the triggering of mechanisms of “programmed” cell death (apoptosis).
Due to more unfavorable blood supply conditions, the subcortical and periventricular white matter of the cerebral hemispheres may suffer to a greater extent than the gray matter of the brain, which causes the clinical picture of chronic cerebral ischemia. As a result of damage to small vessels of the brain, perfusion in the frontal-subcortical areas of the brain is disrupted. Large areas of incomplete infarcts appear in the white matter with demyelination and loss of oligodendrocytes and axons.
Recently, studies have been accumulating showing the connection between arterial stiffness and structural changes in the brain [4, 5].
Clinical manifestation of CMA
Clinical manifestations vary widely depending on the severity and location of brain parenchymal damage, although complete parallels between MRI findings and clinical presentation are not observed. Some older adults with MRI evidence of CMA have no noticeable symptoms. This form is sometimes called “silent” CMA. But the majority have a distinct clinical picture that is a combination of progressive cognitive deficits, gait disturbances, sphincter dysfunction and psychiatric disorders.
Cognitive impairment. CMA associated with age and/or hypertension remains a major cause of vascular cognitive impairment. At least 45% of all cases of dementia are associated with CMA. An MRI predictor of vascular dementia is “silent” lacunar infarctions, which are asymptomatic [6]. Distinctive features of vascular cognitive disorders include impaired executive function, decreased attention, slower processing speed, decreased verbal fluency and delayed recall.
Gait and balance disorders are common in the older adult population, increasing the risk of falls, hospitalization, and mortality. Gait disturbance is considered the second most common consequence of CMA after cognitive impairment [7]. The gait is characterized by a slowing down and shortening of the step (shuffling senile gait in small steps), a violation of the regularity (cadence) of walking, an expansion of the base of walking and difficulties in initiating it (problems of the first step). Among MRI markers of CMA, white matter hyperintensity is most closely associated with balance and gait disturbances, primarily with slowing and shortening of steps [8].
Psychiatric symptoms resulting from CMA mainly include depression, anxiety, disinhibition, apathy, sleep disturbance, appetite disturbance, and in some cases agitation and hallucinations [9]. It has been established that mental disorders (depression and disinhibition) are more dependent on multiple cerebral microbleeds.
Sphincter disorders accompany cognitive deficits in patients in this category, but are often not considered by clinicians as a cerebral symptom. Urinary disorders include nocturia, urinary incontinence, increased frequency of urination, and involuntary urge to urinate. The most common symptom is nocturia, which occurs in approximately 60% of patients with CMA. 20% of patients (every fifth patient) suffer from frequent urination, involuntary urge and urinary incontinence. Frequent urination and nocturia predominate in men, while women more often complain of urinary incontinence. In general, sphincter disorders depend on the degree of damage to the white matter of the periventricular region [10].
Clinical diagnosis of CMA
The progression of the disease in some patients can lead to the development of dementia with limitation of basic types of daily activities and dependence on outside help. Progression of movement disorders (walking and balance) often leads to falls, which significantly limit the patient's mobility. The burden of vascular dementia for the patient, his environment and society as a whole is an important factor that motivates the doctor to early pathogenetic therapy aimed at preventing the progression of the disease and stabilizing the patient’s functional abilities. Detection of cognitive decline in the early stages of the disease in patients in this category may provide a unique opportunity for preventive therapy to prevent the development of vascular dementia. However, for a long time, CMA is asymptomatic and is usually ignored. Therefore, it is important to focus not only on cognitive impairment, but also on nonspecific cerebral symptoms. The earliest clinical marker of insufficiency of cerebral perfusion are disorders of the anxiety-depressive spectrum, manifested by a variety of nonspecific complaints - mainly asthenic circle, behind the facade of which soft cognitive impairments are hidden. Usually this is a violation of regulatory cognitive functions and attention with complete preservation of everyday independence and professional skills.
These patients rarely complain of sadness, a sad mood, or a dreary expectation of the future. On the contrary, nonspecific somatic symptoms of depression are put forward by patients as the main complaints (asthenia, fatigue, pain, poor sleep, loss of appetite, etc.). Anxiety often accompanies late-life depression. A mask for the mental symptoms of depression can also be irritability and grumpiness, which are often considered by others as characteristics of old age. Difficulties in diagnosing depression in older people are associated not only with the peculiarities of the clinical picture of depression, but also with the predominant appeal of patients in this category to general somatic doctors who do not have the skills and experience in assessing mental status. However, the disease can be suspected if there are individual symptoms of anxiety and/or depression, which is available to a doctor of any specialization. It is important that anxiety and depressive symptoms are associated with impairments in other functional areas.
The combination of impaired concentration with mild or moderate symptoms of the anxiety-depressive spectrum and subtle changes in gait in the form of slowing down, shortening the step, and instability indicate the clinical debut of vascular encephalopathy. Typically, the complaints presented by patients are not formally related to objective findings in the neurological status. Therefore, the clinician needs to actively question the patient in detail about the sensations hidden behind a particular complaint. For example, the complaint of dizziness often does not indicate an illusion of movement, but postural instability; the complaint of a constant feeling of heaviness in the head is a subjective correlate of cognitive impairment. The skill of questioning the patient is extremely important for correctly assessing the clinical picture at the onset of the disease. A combination of affective symptoms with mild cognitive impairment and mild gait difficulties may be an indication for an MRI study of the brain, which helps to verify various types of morphological changes associated with the pathology of small cerebral arteries, the main of which are diffuse damage to the white matter (leukoencephalopathy), lacunar heart attacks, microhemorrhages, secondary cerebral atrophy.
As the disease progresses, cognitive deficits worsen. The doctor should not neglect the patient's active complaint of forgetfulness. It is necessary to analyze how the patient's “forgetfulness” affects his daily functioning. It is also important to obtain objective evidence from relatives about the patient’s recent excessive forgetfulness. For example, evidence that the patient cannot remember new names or has difficulty with counting operations. Moderate cognitive impairment is characterized by constant forgetfulness and fatigue when performing normal mental work. The described disorders cause difficulties for the patient, but do not deprive him of his independence. Such a patient cannot properly organize his activities, gets tired quickly, and often makes mistakes due to inattention. When talking with a patient, the doctor may notice that the patient finds it difficult to fully describe the medical history on his own and does not understand the doctor’s recommendations. If such a patient finds himself at a doctor’s appointment with an accompanying person, for example a relative, then when trying to answer the doctor’s question, he turns to the accompanying person, looking for support or tips. This phenomenon is called the “turning head symptom.” The presence of many nonspecific complaints in an elderly patient should also alert the clinician, especially if the patient cannot explain their essence. Cognitive disorders of a vascular nature are necessarily accompanied by disturbances in the neurological status, in particular, gait is almost always impaired. These gait abnormalities can easily be seen even by a physician who is not trained in neurological examination. The patient's gait becomes slow, he experiences difficulty starting to walk, turning, sometimes shuffles, and may fall. In general, the gait resembles “careful” walking. The patient may actively complain of instability.
Syndromic diagnosis includes establishing the fact of a decrease in cognitive abilities compared to the individual norm and assessing the severity of cognitive impairment. Neupsychological tests can provide significant assistance in syndromic diagnosis. The easy-to-use Mini-Cog test is used for cognitive screening. The most sensitive and specific for mild cognitive impairment is the Montreal Cognitive Assessment Scale (MoCa), which includes the study of various cognitive areas: concentration, executive functions, memory, language, visual-constructive skills, abstract thinking, calculation and orientation.
At the second stage of the diagnostic search, the most likely cause of cognitive disorders is determined, i.e. nosological diagnosis is carried out. If a patient is suspected of having a history of cognitive deficits, one should try to identify and weigh risk factors for vascular cognitive impairment: arterial hypertension of unknown duration, overweight, cardiac pathology, impaired glycemic control, etc. Somatic examination is absolutely necessary to diagnose the leading vascular risk factor or an equivalent complex of such factors, for example metabolic syndrome.
To verify the vascular nature of cognitive impairment, the results of neuroimaging are of great importance. According to modern requirements, the diagnosis of vascular cognitive disorders is not valid in the absence of neuroimaging confirmation. The assessment of structural changes associated with microangiopathy has improved significantly over the past decade with advances in neuroimaging.
Therapeutic approaches
There is growing evidence that CMA is a more dynamic process than originally thought. The damage progresses over time, and the long-term impact on brain damage varies widely, opening up unprecedented opportunities for targeted therapy. In the early stages of CMA, treatment is carried out taking into account risk factors and is aimed at preventing or significantly slowing down the progression of the disease, incl. development of acute conditions.
Basic strategies:
- normalization of blood pressure (BP), carbohydrate and lipid metabolism if they are disturbed;
- combating smoking, obesity and physical inactivity;
- limiting the consumption of alcohol, salt, animal fats.
To implement these measures, first of all, the patient should be motivated to follow a proper diet rich in antioxidants and increase physical activity. Persons who prefer the so-called Mediterranean diet, are less likely to have cognitive impairment [11]. Numerous studies demonstrate the benefit of lowering blood pressure to a target level of systolic blood pressure less than 130 mm Hg, primarily in relation to lacunar strokes [12]. The position regarding statins is currently being reviewed. If it was previously believed that statins were necessary primarily to reduce low-density lipoprotein levels, now we have convincing evidence of their cardiovascular protection. Statins improve vasomotor reserve and endothelial function by inhibiting vascular superoxide production [13] and improving NO bioavailability. Thus, the antioxidant properties of statins are beginning to be considered as an independent therapeutic effect in patients with CMA. At the same time, large-scale studies of the use of antiplatelet therapy in patients with CAM show conflicting data regarding target symptoms [14]. It is likely that some specific categories of patients, such as patients with diabetes, may benefit most from the use of antiplatelet agents. The use of vitamin B12, folate and vitamin E also appears to be beneficial in selected cases. With age, the absorption of vitamin B12, an important coenzyme in cognitive processes, decreases. Annual testing of vitamin B12 levels after age 65 is a very significant aspect of preventing cognitive deficits associated with hypovitaminosis.
Of course, the system of these measures has a positive effect on endothelial function and the NO system, but it is not optimal, which requires the search for more effective agents that affect both the endothelium and clinical symptoms. One candidate for targeting the endothelium and cell membranes is Gingko Biloba extract (GBE). The leaves of Ginkgo biloba, a "living fossil", have been used as traditional herbal medicine for hundreds of years in China. Today, EGB-based drugs are widely used both in the East and in the West. Medicinal plants are gaining popularity due to the various benefits they have, such as fewer side effects, relatively low cost and high availability, and high patient compliance due to their long history of use. Research into EHD (EGb 761) has been ongoing for many years. Early studies showed that the extract was superior to placebo in improving symptoms of dementia, and this was confirmed by later studies. The GINDEM-NP, GOTADAY, and GOT-IT studies showed that 240 mg/day of EGb 761 improved cognitive function, decreased neuropsychiatric symptoms, increased activities of daily living, and increased quality of life in patients with mild to moderate dementia compared to placebo. and the results were reproduced in independent studies.
Currently, its use for vascular protection is receiving much attention. EGB has been shown to act as an antioxidant and free radical scavenger, membrane stabilizer, platelet activating factor inhibitor, vasodilator, and metabolic regulator [15]. An increasing number of clinical studies are accumulating on the use of EGB in the treatment of cardiovascular diseases, peripheral vascular diseases and diabetic vascular complications. More than 40 experimental studies have shown that EGB has a significant protective effect on experimental focal cerebral ischemia [16].
EGB combines well with most medications, including antihypertensive drugs. However, blood pressure monitoring is recommended when a patient first begins taking EGB, as ginkgo biloba has been shown to lower blood pressure in some studies [17]. But the results of most special studies indicate that gingo biloba does not affect blood pressure [18, 19]. The medicine is safe to use in patients taking antiplatelet agents. Several randomized controlled trials have shown that ginkgo biloba does not increase the risk of bleeding when added to aspirin at doses up to 500 mg/day [20, 21]. The safety and tolerability of EGb 761 have been shown to be excellent across different drug doses [22].
Conclusion
Early diagnosis and treatment of clinical manifestations of CMA are the most important components of the prevention of vascular dementia. The inclusion of a safe drug based on EGB in the complex treatment of CMA is pathogenetically justified and can increase the availability of treatment for patients in this category.
Causes
Development factors are different. Among the possible:
- Past severe infectious processes. Especially affecting the brain. It is this disorder that often becomes a trigger, a trigger for amyloidosis. The immune system begins to react inadequately to imaginary stimuli.
- Cardiovascular pathologies. Already named hypertension or symptomatic increase in blood pressure.
- Diabetes. The real scourge of patients with this diagnosis is problems with vessels of various sizes throughout the body. In addition, it may be influenced by other hormonal diseases. Like pathologies of the thyroid gland, adrenal glands.
- Smoking, alcoholism. Bad habits.
- Also excessive physical activity.
- Genetic disorders.
- Malfunctions of the immune system. Against the background of other disorders or as a primary deviation, which rarely happens.
Microangiopathy of cerebral vessels can be polyetiological, that is, due to a group of reasons. All of them are taken into account to determine the path of fundamental treatment.
Types of disease
Microangiopathy of the brain is divided into four forms:
- Cerebral amyloid type of disease. This form is formed in response to pathological protein deposition, and appears most often in old age.
- Lenticulostriate appearance. Children are at risk for this disease. According to the latest data, microangiopathy of this type is a normal variant, but requires constant monitoring.
- Diabetic form of the disease. With the progression of diabetes mellitus, an increase in the syndrome of cerebral manifestations is observed.
- The hypertensive type of microangiopathy is typical for patients suffering from hypertension.
In one case or another, the production of collagen and glycoproteins increases, which leads to a thickening of the capillary membrane. The result is a decrease in the quality of metabolic processes, deterioration of nutrition at the site of vascular damage, and the formation of foci of gliosis.
Diagnostics
The examination is the task of neurologists. If necessary, a specialist in vascular surgery is involved.
The list of activities is always identical, with minor deviations:
- Oral questioning of the patient. It is necessary to identify complaints and make a list of symptoms. This will allow you to determine the direction of further diagnostics.
- Anamnesis collection. In particular: infectious processes suffered in the recent past, current and chronic pathologies, family history of diseases, bad habits.
- General and biochemical blood tests.
- Electroencephalography. To determine the functional activity of cerebral structures.
- MRI or CT scan of the brain. It is possible to conduct two studies at once. Used to identify the location, number of lesions, and severity of the disorder.
Dopplerography and duplex scanning are also possible. To determine the quality of trophism of nerve tissue.
What do white and black spots mean on MRI images?
Zones of altered MR signal may indicate:
- tissue ischemia;
- edema;
- necrosis;
- purulent melting;
- tumor transformation;
- metastatic lesion;
- gliosis;
- demyelination;
- degeneration, etc.
The radiologist describes the signal intensity, size and location of the lesion. Taking into account the information received, the patient’s complaints and data from previous examinations, the specialist can assume the nature of the pathological changes.
Acute disseminated encephalomyelitis on MRI
Treatment
Therapy involves solving three problems. Eliminating the root cause, relieving symptoms, preventing complications.
There are two methods: conservative or surgical. In the vast majority of cases, the use of medications and, if necessary, lifestyle adjustments are sufficient. What medications are prescribed?
For hypertension and symptomatic increase in blood pressure:
- Means for lowering blood pressure. Beta blockers (Propranolol, Anaprilin, Metoprolol), ACE inhibitors (perindopril in different variations), calcium antagonists (Diltiazem or Verapamil), diuretics (Veroshpron, Hypothiazide), also diuretics, also centrally acting medications (Moxonidine).
- Statins. To adjust the concentration of cholesterol and other lipids in the bloodstream.
In addition, patients are advised to correct their diet (minimum fat and up to 7 grams of salt per day), adequate drinking regimen (1.3-1.8 liters or more, as needed, taking into account the recommendations of a specialist).
Diabetes:
- Antihyperglycemic agents, insulin as needed.
- Statins.
It is also possible to use medications to lower blood pressure levels.
Lenticulostriate type:
The deposition of calcium salts does not always require correction. There is no specialized treatment. Symptomatic drugs are used.
As for the amyloid form:
- A nicotinic acid. The main means of combating violations.
- Immunosuppressants, glucocorticoids (Prednisolone and analogues), cytostatics as needed. But this occurs extremely rarely. The purpose of these drugs is to reduce the activity of the body's defenses.
Systematic administration of vitamin-mineral complexes is indicated for all categories of patients.
Physiotherapy and acupuncture have proven themselves well.
Surgical correction is rarely needed. If there are clear foci of microangiopathy and there is a critical disturbance in the nutrition of nerve tissue in this particular area of the brain. With an additional condition: the drugs do not help.
Attention:
None of these methods can completely eliminate the disorder in the later stages. Foci of gliosis and scars do not disappear anywhere.
However, there is every chance of bringing the disorder under control. Moreover, the body, through the development of collaterals, can cope quite well on its own. You just need to support him.
Possible complications
{banner_banstat9}
Consequences are relatively rare. Years pass from the development of microangiopathy to the final outcome. However, you cannot relax.
Possible problems include:
- Stroke. Acute cerebrovascular accident. Provokes the death of nerve tissue. Severe disability with neurological deficit. The death of a person is possible and even probable.
- Encephalopathy. The process is similar, but there is no destruction of cerebral structures yet.
- Vascular dementia. Dementia due to insufficient brain nutrition.
Complications develop spontaneously. Treatment is the only way to prevent them.
Where do gliosis foci appear?
If you have a headache due to nosology, MRI will detect multiple areas of glial tissue. The lesions affect different parts of the brain. They are located with equal probability both inside the white matter and superficially.
Forms of gliosis according to the structure of the foci:
- Fibrous – morphological defects contain most of the fibers;
- Marginal - zones are localized superficially under the shell;
- Vascular - the proliferation of small capillaries predominates;
- Anisomorphic – chaotic arrangement of glial elements predominant over the fibers;
- Perivascular – neuroglia are located around the affected vessels (with vasculitis);
- Focal - a limited area at the site of inflammation;
- Diffuse – spread of the process to the brain and spinal cord;
- Supratentorial - single foci of gliosis of vascular origin in the brain are formed during human aging, after childbirth. The course is asymptomatic.
Magnetic resonance imaging of the brain allows one to count foci of gliosis. Tomograms show the structure of the areas. The wider the focus, the more clinical symptoms of central nervous system damage.
Dynamic examination (repeated MRI) allows us to evaluate the increase in the size of brain lesions.